Neutrophilic panniculitis is a rare skin condition that can leave many scratching their heads. This inflammatory disorder affects the fat layer beneath the skin, causing painful nodules and plaques. But what exactly triggers this condition? Neutrophilic panniculitis often results from infections, autoimmune diseases, or even certain medications. Symptoms can vary widely, making it tricky to diagnose. Treatment usually involves addressing the underlying cause and may include anti-inflammatory drugs or immunosuppressants. Understanding this condition is crucial for managing its symptoms effectively. Ready to dive into some intriguing facts about neutrophilic panniculitis? Let's get started!
Key Takeaways:
- Neutrophilic panniculitis is a rare condition causing painful lumps under the skin. It can be triggered by infections, medications, or autoimmune disorders, and requires tailored treatment for relief.
- Ongoing research is exploring new treatments and diagnostic techniques for neutrophilic panniculitis. Living a healthy lifestyle and seeking support can help manage the condition and improve quality of life.
What is Neutrophilic Panniculitis?
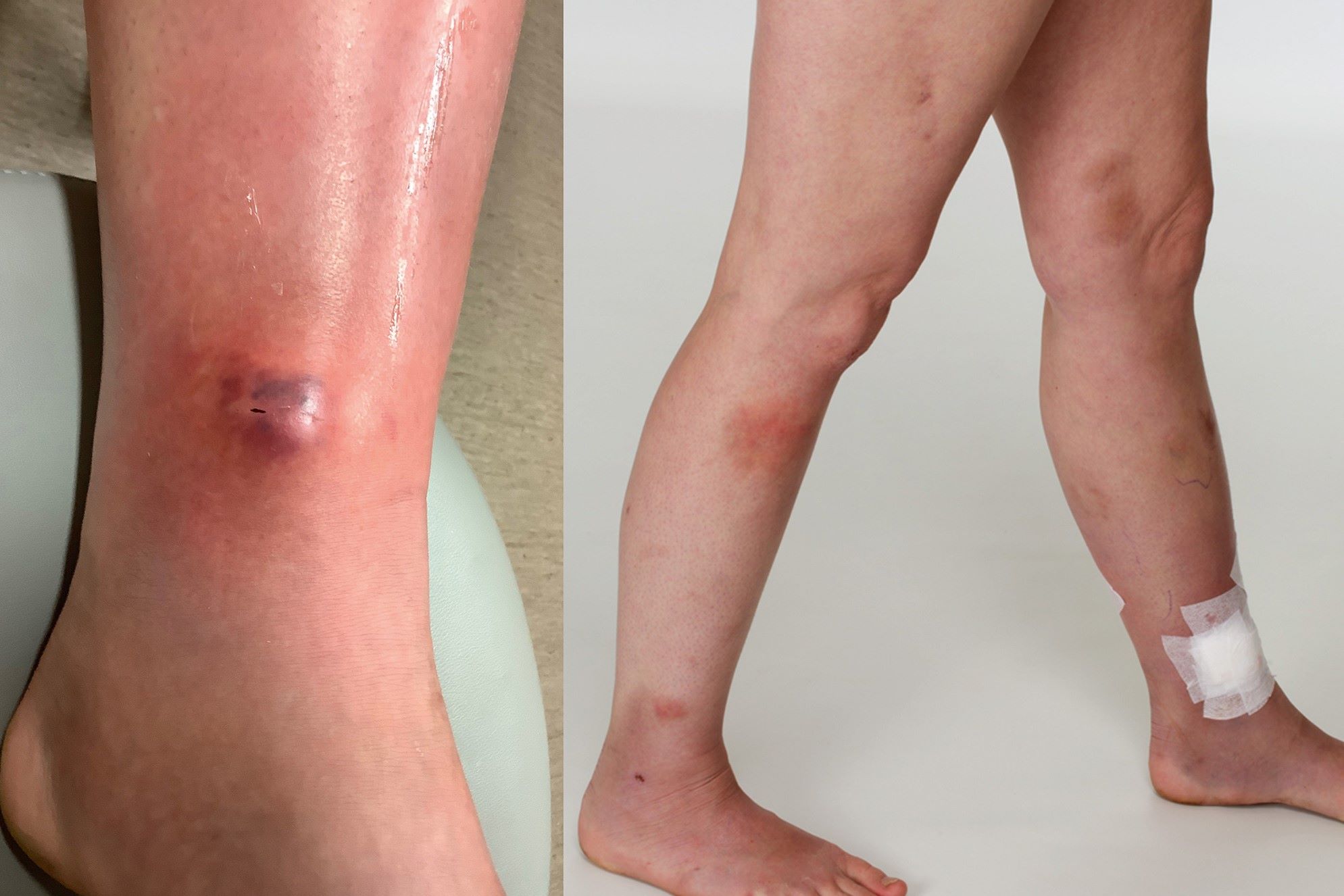
Neutrophilic panniculitis is a rare inflammatory condition affecting the subcutaneous fat layer. It involves the infiltration of neutrophils, a type of white blood cell, into the fat tissue. This condition can cause painful nodules and other symptoms.
-
Neutrophilic panniculitis primarily affects the subcutaneous fat layer, leading to inflammation and pain.
-
The condition is characterized by the presence of neutrophils, which are a type of white blood cell, in the affected tissue.
-
It can cause painful nodules or lumps under the skin, often accompanied by redness and swelling.
Causes and Risk Factors
Understanding the causes and risk factors of neutrophilic panniculitis can help in managing and preventing the condition. While the exact cause is often unknown, several factors may contribute.
-
The exact cause of neutrophilic panniculitis is often unknown, making it a challenging condition to diagnose and treat.
-
Autoimmune disorders, where the body's immune system attacks its own tissues, can be a contributing factor.
-
Infections, particularly bacterial infections, can trigger the condition in some individuals.
-
Certain medications, including antibiotics and chemotherapy drugs, have been linked to the development of neutrophilic panniculitis.
Symptoms and Diagnosis
Recognizing the symptoms and understanding the diagnostic process is crucial for early detection and treatment. Symptoms can vary widely among individuals.
-
Common symptoms include painful nodules or lumps under the skin, often accompanied by redness and swelling.
-
Fever and general malaise can also be associated with neutrophilic panniculitis, indicating a systemic inflammatory response.
-
Diagnosis typically involves a combination of clinical examination, medical history, and biopsy of the affected tissue.
-
Imaging studies, such as ultrasound or MRI, may be used to assess the extent of the inflammation and rule out other conditions.
Treatment Options
Effective treatment options are essential for managing symptoms and improving quality of life. Treatment plans are often tailored to the individual's specific needs.
-
Treatment often involves the use of anti-inflammatory medications to reduce pain and swelling.
-
Corticosteroids, either oral or topical, are commonly prescribed to manage inflammation.
-
Immunosuppressive drugs may be used in cases where autoimmune disorders are a contributing factor.
-
Antibiotics may be necessary if a bacterial infection is identified as a trigger.
Complications and Prognosis
Understanding potential complications and the overall prognosis can help patients and healthcare providers manage expectations and plan for long-term care.
-
Complications can include chronic pain and persistent inflammation, which may require ongoing treatment.
-
In severe cases, the condition can lead to tissue necrosis, where the affected tissue dies due to lack of blood flow.
-
The prognosis varies widely among individuals, with some experiencing complete resolution of symptoms and others requiring long-term management.
Research and Future Directions
Ongoing research is crucial for improving our understanding of neutrophilic panniculitis and developing more effective treatments.
-
Researchers are investigating the underlying mechanisms of the condition to identify potential targets for new therapies.
-
Clinical trials are exploring the efficacy of novel anti-inflammatory and immunosuppressive drugs.
-
Advances in genetic research may help identify individuals at higher risk for developing neutrophilic panniculitis.
-
Improved diagnostic techniques, including advanced imaging and molecular testing, are being developed to enhance early detection and treatment.
Living with Neutrophilic Panniculitis
Living with neutrophilic panniculitis can be challenging, but there are strategies to manage symptoms and improve quality of life.
-
Regular follow-up with a healthcare provider is essential for monitoring the condition and adjusting treatment as needed.
-
Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can help support overall health and well-being.
-
Stress management techniques, such as meditation and yoga, may help reduce the impact of stress on the immune system.
-
Support groups and counseling can provide emotional support and practical advice for managing the condition.
Interesting Facts
Here are some additional interesting facts about neutrophilic panniculitis that you might find intriguing.
-
Neutrophilic panniculitis is more common in adults than in children, although it can occur at any age.
-
The condition can sometimes be mistaken for other types of panniculitis or skin conditions, making accurate diagnosis important.
-
Some cases of neutrophilic panniculitis are associated with systemic diseases, such as rheumatoid arthritis or inflammatory bowel disease.
-
Despite its rarity, neutrophilic panniculitis has been documented in medical literature for over a century, highlighting the ongoing need for research and awareness.
Final Thoughts on Neutrophilic Panniculitis
Neutrophilic panniculitis, a rare inflammatory condition, affects the subcutaneous fat layer. Recognizing its symptoms, such as tender nodules and skin discoloration, can lead to early diagnosis and treatment. While the exact cause remains unclear, links to autoimmune diseases and infections have been noted. Treatment often involves corticosteroids and immunosuppressive drugs to manage inflammation and pain.
Understanding this condition helps in managing it better and improving the quality of life for those affected. Staying informed and consulting healthcare professionals at the first sign of symptoms can make a significant difference.
Remember, while neutrophilic panniculitis is rare, awareness and timely medical intervention are key to managing it effectively. Stay vigilant, stay informed, and don't hesitate to seek medical advice if you notice any unusual skin changes.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
