Experimental Allergic Encephalomyelitis (EAE) is a widely studied animal model for multiple sclerosis (MS). Researchers use EAE to understand the mechanisms behind MS and to test potential treatments. This model helps scientists explore how the immune system attacks the central nervous system, leading to inflammation and damage. EAE is induced in animals, usually mice or rats, by injecting them with myelin proteins, which triggers an immune response similar to that seen in MS patients. Understanding EAE is crucial for developing new therapies and improving the lives of those affected by MS. Let's dive into 30 intriguing facts about this important research tool.
Key Takeaways:
- EAE is a disease in animals that helps scientists understand and test treatments for multiple sclerosis (MS). It mimics MS symptoms and has led to important discoveries about the immune system.
- While EAE has been helpful, it doesn't fully represent MS in humans. Scientists are working on better models and treatments by combining EAE findings with clinical data.
What is Experimental Allergic Encephalomyelitis?
Experimental Allergic Encephalomyelitis (EAE) is a widely studied animal model of multiple sclerosis (MS). Researchers use EAE to understand the mechanisms of MS and to test potential treatments. Here are some fascinating facts about EAE:
- EAE is an autoimmune disease that affects the central nervous system (CNS) of animals, primarily rodents.
- It was first described in the 1930s by Thomas Rivers and colleagues.
- EAE is induced by injecting animals with myelin proteins or peptides, which triggers an immune response against the CNS.
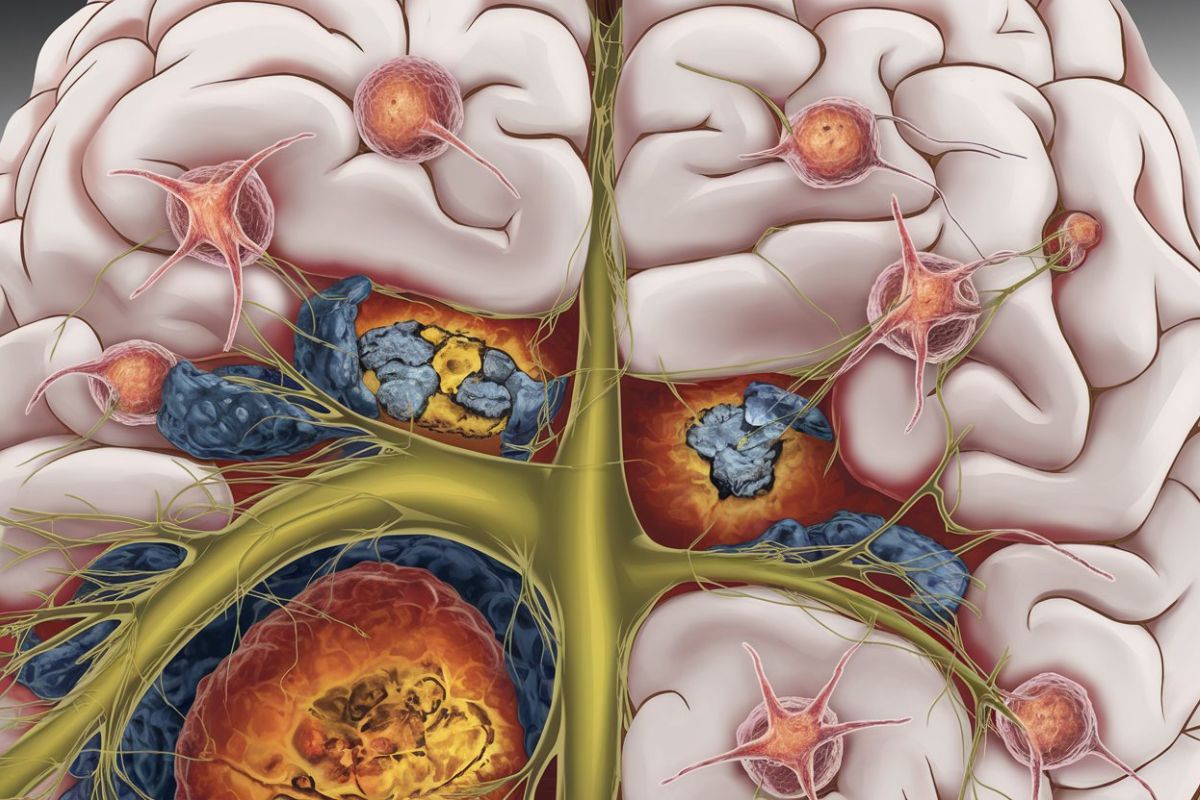
- The disease is characterized by inflammation, demyelination, and axonal damage in the CNS.
- EAE can be induced in various species, including mice, rats, guinea pigs, and primates.
- The most commonly used animal model for EAE is the mouse, due to its genetic similarities to humans and ease of manipulation.
- EAE is used to study the pathogenesis of MS, as it shares many clinical and pathological features with the human disease.
- Researchers use EAE to test new drugs and therapies for MS before they are tested in humans.
- EAE has helped identify several key immune cells involved in MS, such as T cells, B cells, and macrophages.
- The disease can be induced using different myelin proteins, such as myelin basic protein (MBP), proteolipid protein (PLP), and myelin oligodendrocyte glycoprotein (MOG).
How EAE is Induced
Inducing EAE in animals involves specific procedures and materials. This process helps researchers create a consistent model for studying MS.
- EAE induction typically involves injecting animals with a myelin antigen emulsified in an adjuvant, such as complete Freund's adjuvant (CFA).
- Pertussis toxin is often administered alongside the myelin antigen to enhance the immune response and facilitate disease development.
- The choice of myelin antigen and adjuvant can influence the severity and course of the disease.
- Different strains of mice exhibit varying susceptibility to EAE, which can be useful for studying genetic factors in MS.
- EAE can be induced through active immunization (injecting myelin antigens) or passive transfer (injecting activated immune cells from a donor animal with EAE).
Symptoms and Pathology of EAE
EAE presents with a range of symptoms and pathological features that resemble those seen in MS. Understanding these aspects is crucial for developing effective treatments.
- Common symptoms of EAE include paralysis, weight loss, and reduced mobility.
- The disease often progresses through distinct phases, including an acute phase with severe symptoms and a chronic phase with milder, persistent symptoms.
- Inflammation in the CNS is a hallmark of EAE, with immune cells infiltrating the brain and spinal cord.
- Demyelination, or the loss of myelin sheaths around nerve fibers, is a key pathological feature of EAE.
- Axonal damage and loss of neurons can occur in severe cases of EAE, leading to permanent neurological deficits.
Research and Therapeutic Insights from EAE
EAE has provided valuable insights into the mechanisms of MS and has guided the development of new therapies. Here are some key findings from EAE research:
- EAE studies have identified several cytokines and chemokines that play crucial roles in the disease process, such as interferon-gamma (IFN-γ) and interleukin-17 (IL-17).
- Researchers have discovered that regulatory T cells (Tregs) can suppress the immune response in EAE, offering potential therapeutic strategies for MS.
- EAE has been used to test the efficacy of various immunomodulatory drugs, such as fingolimod and natalizumab, which are now approved for treating MS.
- The model has also been instrumental in evaluating the potential of stem cell therapies for repairing CNS damage in MS.
- EAE research has highlighted the importance of the blood-brain barrier in MS, as its disruption allows immune cells to enter the CNS and cause damage.
Limitations and Future Directions
While EAE has been invaluable for MS research, it has some limitations. Researchers are continuously working to improve the model and develop new approaches.
- EAE does not fully replicate the complexity and heterogeneity of MS in humans.
- The disease course in EAE is often more rapid and severe than in MS, which can limit the model's relevance for studying chronic aspects of the disease.
- Some therapeutic interventions that show promise in EAE may not be effective in humans, highlighting the need for additional validation in clinical trials.
- Researchers are exploring alternative animal models and advanced techniques, such as humanized mice and organ-on-a-chip systems, to better mimic MS.
- Future research aims to integrate findings from EAE with clinical data to develop more targeted and effective treatments for MS.
Final Thoughts on Experimental Allergic Encephalomyelitis
Experimental Allergic Encephalomyelitis (EAE) offers a window into understanding autoimmune diseases like multiple sclerosis. This condition, induced in lab animals, helps researchers study the immune system's attack on the central nervous system. EAE models have been pivotal in developing treatments and therapies for human autoimmune disorders.
Researchers use EAE to test new drugs, understand disease mechanisms, and explore genetic factors. Despite its complexity, EAE remains a cornerstone in immunology research. It has led to significant breakthroughs, including the development of immunomodulatory therapies.
Understanding EAE not only advances scientific knowledge but also brings hope for better treatments for autoimmune diseases. The ongoing research in this field continues to shed light on the intricate workings of the immune system, paving the way for future medical advancements.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
