What is a pericardium congenital anomaly? A pericardium congenital anomaly is a rare heart condition present at birth. The pericardium, a double-walled sac containing the heart, can have defects or be completely absent. These anomalies can lead to complications like heart compression or abnormal heart positioning. Some individuals might not experience symptoms, while others could face serious health issues. Understanding these anomalies helps in early diagnosis and treatment. This blog post will explore 25 intriguing facts about pericardium congenital anomalies, shedding light on their causes, symptoms, and potential treatments. Get ready to learn more about this unique heart condition!
Key Takeaways:
- Pericardium congenital anomalies are rare heart conditions that can go unnoticed, but may lead to complications like chest pain and abnormal heart rhythms.
- Treatment options range from regular monitoring to surgery, highlighting the importance of early detection and management for individuals with this condition.
What is a Pericardium Congenital Anomaly?
A pericardium congenital anomaly refers to a rare condition where the pericardium, the protective sac around the heart, develops abnormally. These anomalies can range from partial absence to complete absence of the pericardium. Understanding these anomalies helps in diagnosing and managing potential heart-related issues.
- Rare Occurrence: Only about 0.01% of the population is affected by pericardium congenital anomalies.
- Asymptomatic Nature: Many individuals with this condition show no symptoms and may never know they have it.
- Partial Absence: Most common form is the partial absence of the pericardium, often on the left side.
- Complete Absence: Complete absence of the pericardium is less common but can lead to more significant heart issues.
- Genetic Factors: Some cases are linked to genetic mutations, though the exact cause is often unknown.
Symptoms and Diagnosis
Symptoms can vary widely, and diagnosis often requires specific imaging techniques. Here are some key points about symptoms and how doctors diagnose this condition.
- Chest Pain: Some individuals may experience chest pain, especially during physical activity.
- Shortness of Breath: Difficulty breathing can occur, particularly during exertion.
- Heart Murmurs: Abnormal heart sounds may be detected during a physical exam.
- Echocardiogram: An ultrasound of the heart can help visualize the pericardium and detect anomalies.
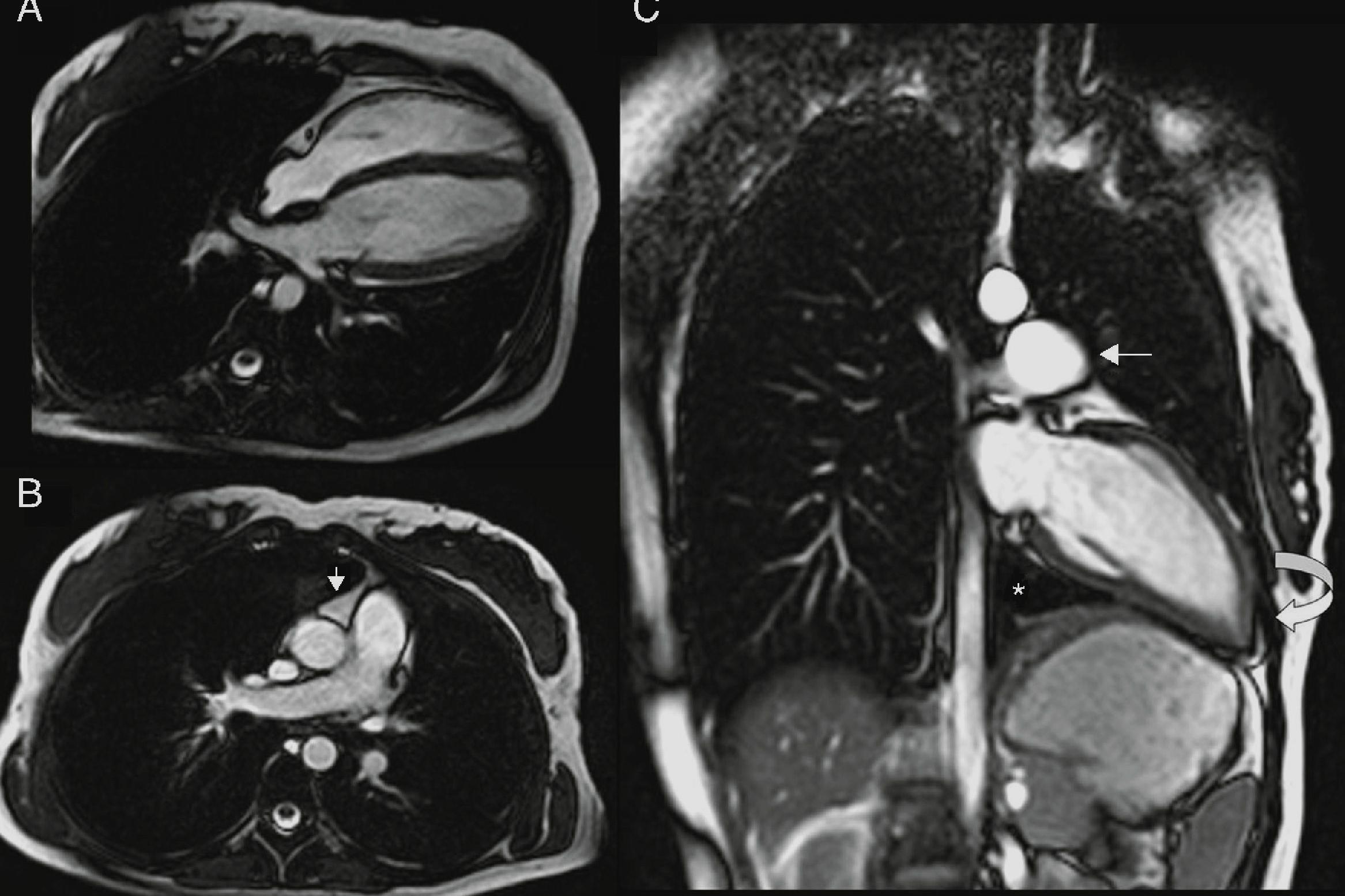
- MRI and CT Scans: These imaging techniques provide detailed views of the heart and pericardium, aiding in diagnosis.
Potential Complications
While many people with pericardium congenital anomalies live normal lives, there are potential complications that can arise.
- Heart Displacement: The heart may shift position within the chest cavity, leading to complications.
- Compression of Heart Structures: Absence of the pericardium can cause compression of heart structures, affecting function.
- Increased Risk of Herniation: The heart may herniate into the chest cavity, which can be life-threatening.
- Arrhythmias: Abnormal heart rhythms can develop due to the altered structure of the heart.
- Sudden Cardiac Death: In rare cases, severe complications can lead to sudden cardiac death.
Treatment Options
Treatment depends on the severity of the anomaly and the presence of symptoms. Here are some common approaches.
- Monitoring: Asymptomatic individuals may only require regular monitoring by a cardiologist.
- Medications: Drugs to manage symptoms like chest pain or arrhythmias may be prescribed.
- Surgical Intervention: In severe cases, surgery may be needed to correct the anomaly or address complications.
- Lifestyle Modifications: Patients may be advised to avoid strenuous activities that could exacerbate symptoms.
- Regular Check-ups: Ongoing medical check-ups are crucial to monitor heart health and detect any changes early.
Interesting Facts
Here are some intriguing facts about pericardium congenital anomalies that highlight the uniqueness of this condition.
- Historical Cases: The first documented case was reported in the 16th century.
- Animal Studies: Research on animals has provided insights into the development and impact of these anomalies.
- Incidental Findings: Many cases are discovered incidentally during imaging for unrelated issues.
- Gender Differences: Males are slightly more likely to have this condition than females.
- Research Advances: Ongoing research aims to better understand the genetic and developmental factors involved.
Final Thoughts on Pericardium Congenital Anomaly
Understanding pericardium congenital anomaly can be a game-changer for those affected. This rare condition, involving the sac around the heart, often goes unnoticed due to its subtle symptoms. Early detection and proper medical care are crucial for managing the condition effectively. Awareness among healthcare professionals and the general public can lead to better outcomes.
Patients with this anomaly should maintain regular check-ups and follow their doctor's advice closely. Advances in medical technology and research continue to improve diagnosis and treatment options. Staying informed about the latest developments can make a significant difference.
By spreading knowledge about pericardium congenital anomaly, we can help those affected lead healthier lives. Remember, early intervention is key. If you or someone you know shows symptoms, seek medical advice promptly. Let's work together to ensure everyone gets the care they need.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
