Ichthyosis hystrix of Curth-Macklin (IHCM) is a rare genetic skin disorder characterized by thick, spiky scales that resemble porcupine quills. IHCM affects the skin's ability to shed dead cells, leading to a buildup of rough, dark patches. This condition is usually present at birth or develops in early childhood. IHCM is inherited in an autosomal dominant pattern, meaning only one parent needs to carry the gene for a child to be affected. Symptoms can vary widely, from mild to severe, impacting daily life and self-esteem. Treatment focuses on managing symptoms through moisturizing creams, keratolytic agents, and sometimes retinoids. Understanding IHCM can help those affected and their families navigate this challenging condition.
Key Takeaways:
- IHCM is a rare genetic skin disorder with thick, spiky scales. It's caused by a gene mutation and can affect mental health and social interactions. Treatments focus on symptom management and support is crucial.
- Research for IHCM offers hope for the future, including potential gene therapy and stem cell research. Clinical trials and patient registries play a key role in advancing understanding and treatment options.
What is Ichthyosis hystrix of Curth-Macklin (IHCM)?
Ichthyosis hystrix of Curth-Macklin (IHCM) is a rare genetic skin disorder. It is characterized by thick, spiky scales on the skin. This condition can be quite challenging for those affected. Here are some intriguing facts about IHCM.
Genetic Basis of IHCM
IHCM is rooted in genetics. Understanding its genetic foundation helps in grasping the nature of this condition.
- IHCM is inherited in an autosomal dominant manner. This means only one copy of the altered gene is needed to cause the disorder.
- The gene responsible for IHCM is KRT1. Mutations in this gene disrupt normal skin cell function.
- KRT1 encodes keratin 1, a protein crucial for skin integrity. Keratin 1 helps form the structure of the outer skin layer.
- Mutations in KRT1 lead to abnormal keratinization. This results in the thick, spiky scales characteristic of IHCM.
Symptoms and Physical Manifestations
The symptoms of IHCM are quite distinct. They primarily affect the skin but can vary in severity.
- Thick, spiky scales cover large areas of the body. These scales can be dark and rough.
- The scales often appear in infancy or early childhood. They tend to worsen over time.
- Affected areas can include the face, scalp, and limbs. The scales can cause discomfort and social challenges.
- Skin may become prone to infections. The thickened skin can crack, creating entry points for bacteria.
Diagnosis and Identification
Diagnosing IHCM involves several steps. Medical professionals use various methods to confirm the condition.
- Clinical examination is the first step in diagnosis. Doctors look for characteristic skin changes.
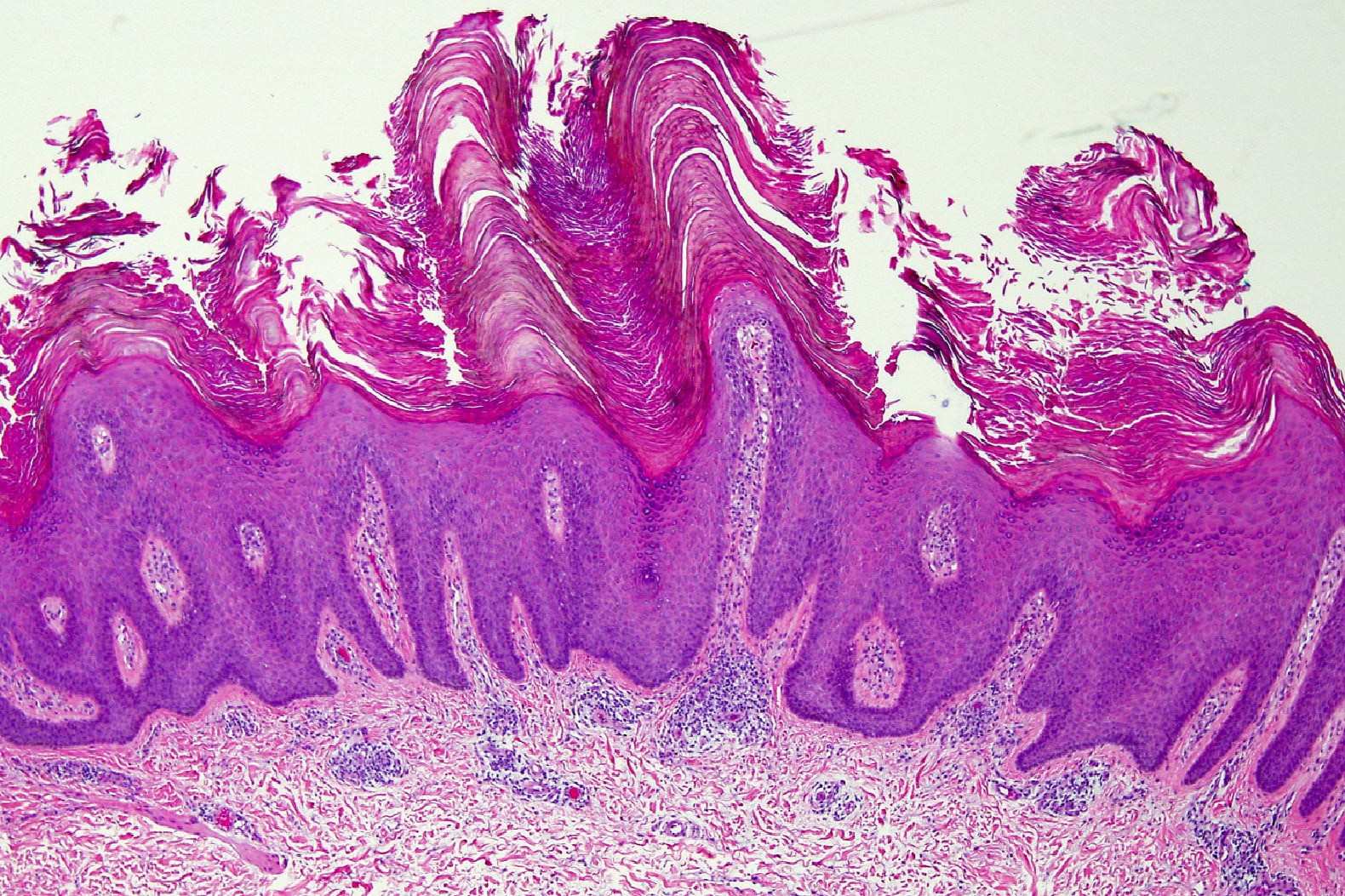
- Skin biopsy can provide more information. A small sample of skin is examined under a microscope.
- Genetic testing confirms the diagnosis. Identifying mutations in the KRT1 gene is definitive.
- Family history is also considered. A pattern of similar skin issues in relatives can support the diagnosis.
Treatment and Management
Managing IHCM focuses on alleviating symptoms. There is no cure, but treatments can improve quality of life.
- Topical treatments help soften the scales. Moisturizers and keratolytic agents are commonly used.
- Oral retinoids can reduce skin thickening. These medications help normalize skin cell growth.
- Regular skin care routines are essential. Gentle cleansing and moisturizing can prevent complications.
- Antibiotics may be needed for skin infections. Prompt treatment of infections is crucial.
Psychological and Social Impact
Living with IHCM can affect mental health and social interactions. Support is important for those affected.
- Visible skin changes can lead to social stigma. People with IHCM may face bullying or discrimination.
- Psychological support can help. Counseling and support groups provide emotional assistance.
- Education about the condition is vital. Raising awareness can reduce stigma and promote understanding.
- Family support plays a key role. Loved ones can offer practical and emotional help.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of IHCM. Advances in science offer hope for the future.
- Gene therapy is a potential future treatment. Correcting the genetic mutation could address the root cause.
- Stem cell research may offer new solutions. Regenerating healthy skin cells could be a game-changer.
- New medications are being developed. Researchers are exploring drugs that target specific pathways involved in IHCM.
- Clinical trials are crucial for progress. Participation in trials helps test new treatments and gather data.
- Patient registries support research efforts. Collecting information from those with IHCM aids in understanding the condition.
The Final Word on Ichthyosis Hystrix of Curth-Macklin
Understanding Ichthyosis hystrix of Curth-Macklin (IHCM) helps us appreciate the complexities of rare skin disorders. This condition, marked by thick, spiky skin, affects individuals in unique ways. While IHCM is rare, awareness and research can lead to better management and support for those affected.
Genetic factors play a significant role in IHCM, making early diagnosis crucial. Treatments focus on symptom relief, often involving moisturizers and keratolytic agents. Though there's no cure, advancements in dermatology offer hope for improved quality of life.
By spreading knowledge about IHCM, we can foster empathy and support for those living with this condition. If you or someone you know is affected, consult a dermatologist for personalized care. Stay informed, stay compassionate, and let's continue to support those with IHCM.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
