Fritsch–Asherman Syndrome is a rare condition that can have a significant impact on women's reproductive health. Characterized by the formation of scar tissue in the uterus, this syndrome often results from surgical procedures like dilation and curettage (D&C). Women with this condition may experience symptoms such as reduced menstrual flow, pelvic pain, or even infertility. Understanding the causes, symptoms, and treatment options is crucial for those affected. This blog post will provide 25 essential facts about Fritsch–Asherman Syndrome, offering valuable insights for anyone seeking to learn more about this condition. Let's dive into the key aspects of this syndrome and how it can be managed effectively.
Key Takeaways:
- Fritsch–Asherman Syndrome, or intrauterine adhesions, can cause menstrual irregularities, pelvic pain, and infertility. Early diagnosis and hysteroscopic surgery are key for treatment and fertility management.
- Scar tissue formation in the uterus can impact a woman's fertility and increase the risk of pregnancy complications. Treatment options include hysteroscopic surgery, hormonal therapy, and follow-up care for managing Fritsch–Asherman Syndrome.
What is Fritsch–Asherman Syndrome?
Fritsch–Asherman Syndrome, also known as intrauterine adhesions, is a condition where scar tissue forms inside the uterus. This can lead to various reproductive issues and other health complications. Here are some key facts about this syndrome:
-
Named After Pioneers: The syndrome is named after Heinrich Fritsch and Joseph Asherman, who first described the condition in the late 19th and early 20th centuries.
-
Scar Tissue Formation: It involves the formation of scar tissue (adhesions) within the uterine cavity, which can cause the walls of the uterus to stick together.
-
Common Cause: The most common cause is trauma to the uterine lining, often due to surgical procedures like dilation and curettage (D&C).
-
Symptoms Vary: Symptoms can range from light or absent menstrual periods to severe pelvic pain and infertility.
-
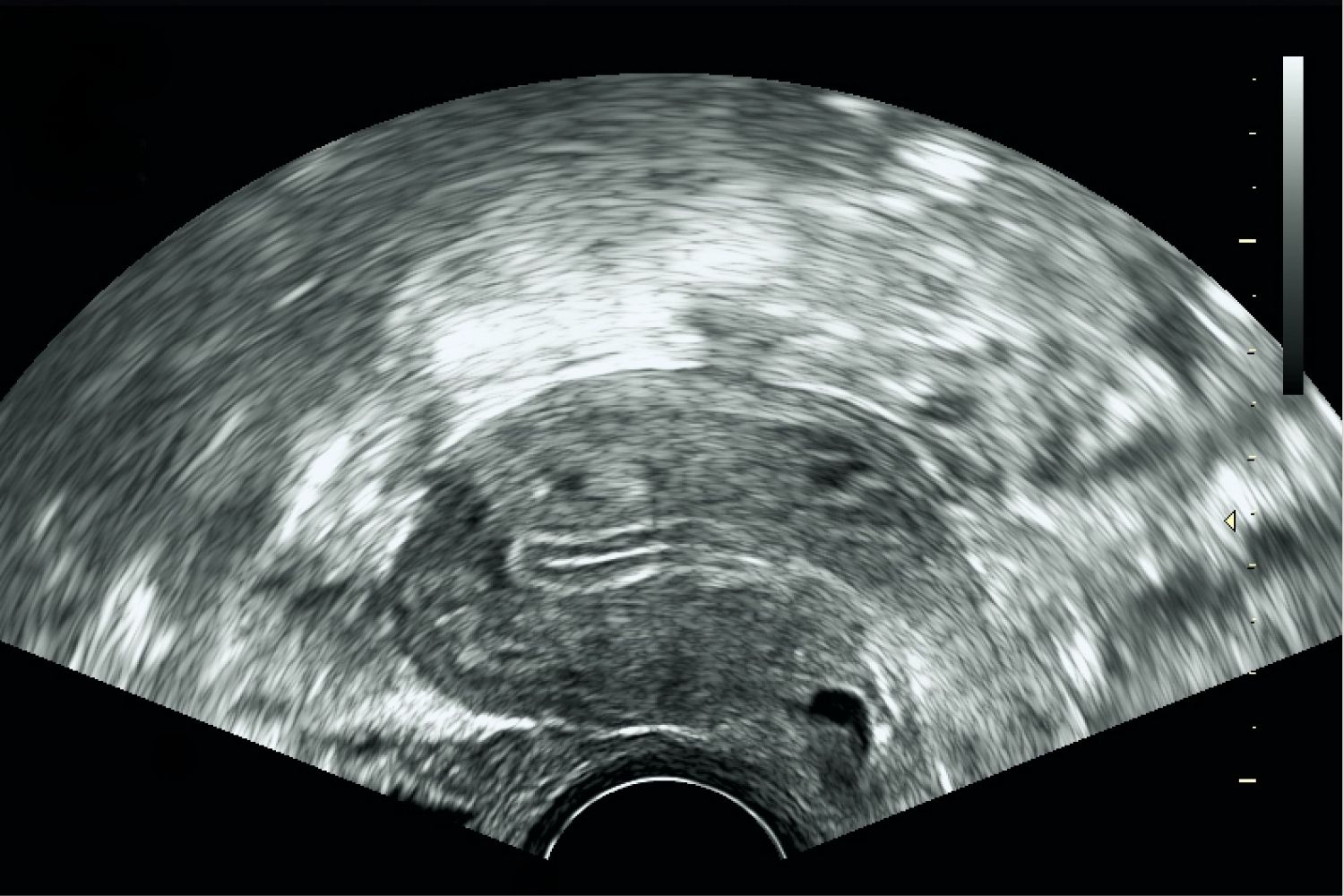
Diagnosis: Diagnosis is typically made through hysteroscopy, a procedure that allows doctors to view the inside of the uterus.
Causes and Risk Factors
Understanding the causes and risk factors can help in early detection and management of Fritsch–Asherman Syndrome.
-
Postpartum Complications: Complications after childbirth, such as retained placenta or postpartum hemorrhage, can increase the risk.
-
Infections: Pelvic infections, particularly those involving the endometrium, can lead to the development of adhesions.
-
Multiple Surgeries: Women who have undergone multiple uterine surgeries are at a higher risk.
-
Tuberculosis: In rare cases, genital tuberculosis can cause intrauterine adhesions.
-
Radiation Therapy: Radiation treatment for pelvic cancers can damage the uterine lining, leading to scar tissue formation.
Symptoms and Diagnosis
Recognizing the symptoms and understanding the diagnostic process is crucial for timely treatment.
-
Menstrual Irregularities: One of the most common symptoms is irregular or absent menstrual periods.
-
Infertility: Many women with this syndrome experience difficulty conceiving.
-
Recurrent Miscarriages: Recurrent pregnancy loss can be a sign of intrauterine adhesions.
-
Pelvic Pain: Chronic pelvic pain is another symptom that can indicate the presence of adhesions.
-
Hysterosalpingography: This imaging test uses dye and X-rays to visualize the uterine cavity and can help in diagnosing the condition.
Treatment Options
Various treatment options are available to manage and treat Fritsch–Asherman Syndrome.
-
Hysteroscopic Surgery: The primary treatment involves hysteroscopic surgery to remove the adhesions.
-
Hormonal Therapy: Post-surgery, hormonal therapy may be used to promote healing of the uterine lining.
-
Intrauterine Device (IUD): In some cases, an IUD is placed to keep the uterine walls apart during healing.
-
Antibiotics: If an infection is present, antibiotics are prescribed to treat it.
-
Follow-Up Care: Regular follow-up care is essential to monitor for recurrence of adhesions.
Impact on Fertility
Fritsch–Asherman Syndrome can significantly impact a woman's fertility and reproductive health.
-
Reduced Implantation: Scar tissue can interfere with the implantation of a fertilized egg.
-
Ectopic Pregnancy: There is an increased risk of ectopic pregnancy due to altered uterine environment.
-
Assisted Reproductive Technologies (ART): Some women may require ART, such as IVF, to achieve pregnancy.
-
Pregnancy Complications: Even after successful treatment, there can be complications during pregnancy, such as preterm labor.
-
Emotional Impact: The emotional toll of dealing with infertility and recurrent miscarriages can be significant, requiring psychological support.
Final Thoughts on Fritsch–Asherman Syndrome
Understanding Fritsch–Asherman Syndrome is crucial for anyone dealing with reproductive health issues. This condition, characterized by the formation of scar tissue in the uterus, can lead to menstrual irregularities and infertility. Early diagnosis and treatment are key to managing symptoms and improving fertility outcomes. Treatments range from surgical intervention to hormonal therapies, depending on the severity. Awareness and education about this syndrome can empower individuals to seek timely medical advice. If you or someone you know is experiencing symptoms, consulting a healthcare professional is essential. Knowledge is power, and being informed about Fritsch–Asherman Syndrome can make a significant difference in one's reproductive health journey. Stay proactive, stay informed, and take control of your health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
