Giant Ganglionic Hyperplasia might sound like a mouthful, but understanding it can be quite simple. This rare condition, also known as Castleman disease, involves abnormal growth of lymph nodes. Imagine your body's defense system going into overdrive, causing these nodes to swell. While it can affect anyone, it’s most commonly seen in adults. Symptoms often include fever, night sweats, and unexplained weight loss. Treatment varies based on the type and severity, ranging from medication to surgery. Curious about more details? Keep reading to uncover 20 intriguing facts about this unusual medical condition.
Key Takeaways:
- Giant Ganglionic Hyperplasia (GGH) is a rare condition affecting nerve cell clusters, causing symptoms like abdominal pain and digestive issues. Early diagnosis and multidisciplinary management are crucial for improving quality of life.
- Research on GGH is ongoing to understand its genetic basis, improve diagnosis, and develop better treatments. Increased awareness among healthcare providers can lead to earlier diagnosis and better management of the condition.
What is Giant Ganglionic Hyperplasia?
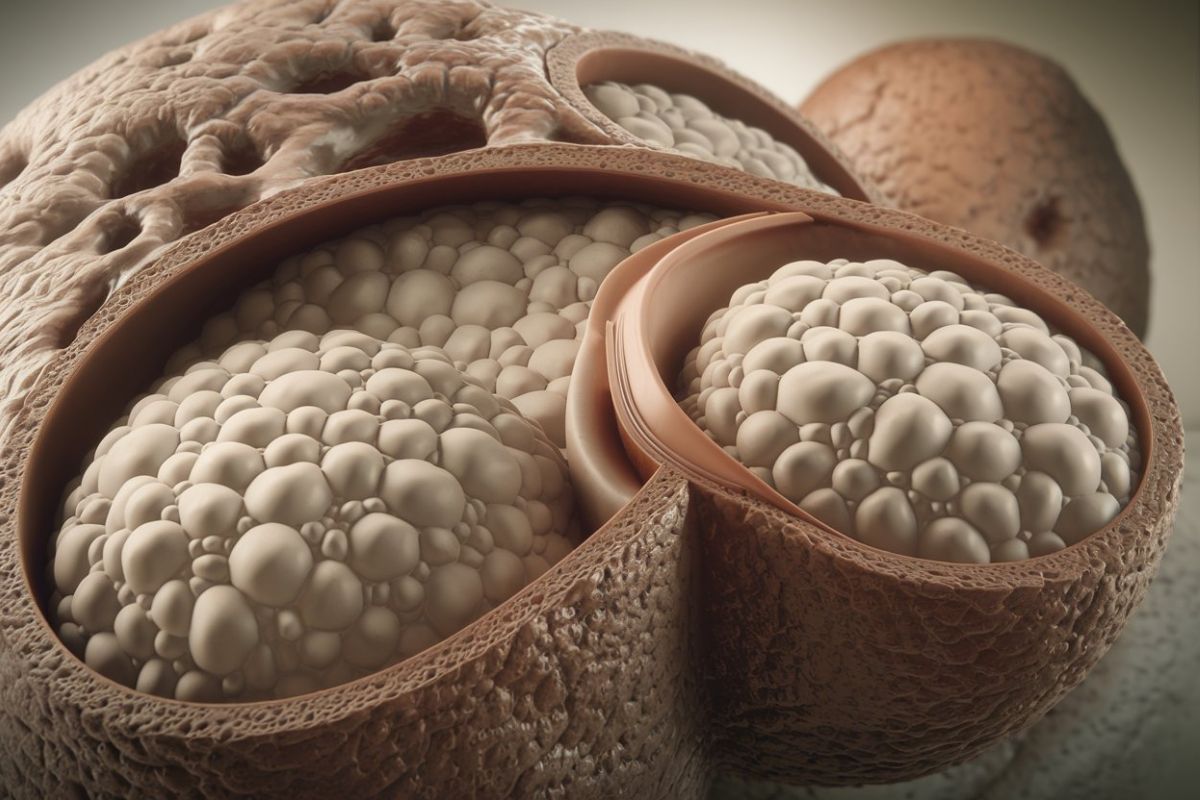
Giant Ganglionic Hyperplasia (GGH) is a rare medical condition that affects the ganglia, which are clusters of nerve cells. This condition can lead to various symptoms and complications. Here are some intriguing facts about GGH.
-
GGH is also known as ganglioneuromatosis, a term that highlights its connection to nerve cell clusters.
-
It primarily affects the autonomic nervous system, which controls involuntary bodily functions like heart rate and digestion.
-
The condition can be congenital, meaning present at birth, or acquired later in life.
-
Symptoms often include abdominal pain, constipation, and diarrhea due to the involvement of the digestive system.
-
GGH can sometimes be associated with other genetic disorders, such as multiple endocrine neoplasia type 2B (MEN2B).
Causes and Diagnosis of GGH
Understanding the causes and how GGH is diagnosed can provide insight into this complex condition.
-
The exact cause of GGH is not well understood, but genetic mutations are believed to play a significant role.
-
Diagnosis often involves a combination of imaging studies, such as MRI or CT scans, and biopsy of affected tissues.
-
Genetic testing can help identify mutations associated with GGH, aiding in diagnosis and management.
-
Early diagnosis is crucial for managing symptoms and preventing complications.
-
Misdiagnosis is common due to the rarity of the condition and its similarity to other gastrointestinal disorders.
Treatment and Management of GGH
Managing GGH requires a multidisciplinary approach involving various medical specialists.
-
Treatment options are limited and often focus on managing symptoms rather than curing the condition.
-
Surgical intervention may be necessary to remove affected ganglia or relieve obstructions in the digestive tract.
-
Medications can help manage symptoms like pain, constipation, and diarrhea.
-
Regular follow-up with healthcare providers is essential to monitor the condition and adjust treatment as needed.
-
Lifestyle changes, such as dietary modifications, can also help manage symptoms and improve quality of life.
Research and Future Directions
Ongoing research aims to better understand GGH and develop more effective treatments.
-
Scientists are exploring the genetic basis of GGH to identify potential targets for therapy.
-
Advances in imaging technology are improving the ability to diagnose and monitor GGH.
-
Clinical trials are investigating new medications and treatment approaches for managing GGH.
-
Patient registries and databases are being established to collect data and improve understanding of the condition.
-
Increased awareness and education about GGH among healthcare providers can lead to earlier diagnosis and better management of the condition.
Final Thoughts on Giant Ganglionic Hyperplasia
Giant Ganglionic Hyperplasia, also known as Castleman Disease, is a rare condition that affects the lymph nodes and related tissues. Understanding its symptoms, causes, and treatments can help those affected manage their health better. This disease can present in various forms, from localized to multicentric, each with unique challenges. Early diagnosis and appropriate treatment are crucial for improving outcomes. Researchers continue to study this condition to find more effective therapies and possibly a cure. Awareness and education about Giant Ganglionic Hyperplasia can lead to better support for patients and their families. If you or someone you know is dealing with this disease, seeking medical advice and connecting with support groups can make a significant difference. Stay informed, stay proactive, and remember that advancements in medical science are continually being made.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
