What is bacterial meningitis? Bacterial meningitis is a severe infection that inflames the protective membranes covering the brain and spinal cord, known as the meninges. This condition can be life-threatening if not treated quickly. Common bacteria causing this disease include Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Symptoms often start suddenly and include high fever, severe headache, stiff neck, and nausea. Living in close quarters, like dorms, increases the risk. Vaccines can prevent some types of bacterial meningitis, making them crucial for those at higher risk. Immediate medical attention is essential for anyone showing symptoms.
What is Bacterial Meningitis?
Bacterial meningitis is a severe infection that inflames the protective membranes around the brain and spinal cord. Understanding its causes, symptoms, and treatments can help in managing this life-threatening condition.
- Definition: Bacterial meningitis is an inflammation of the meninges caused by bacterial infection.
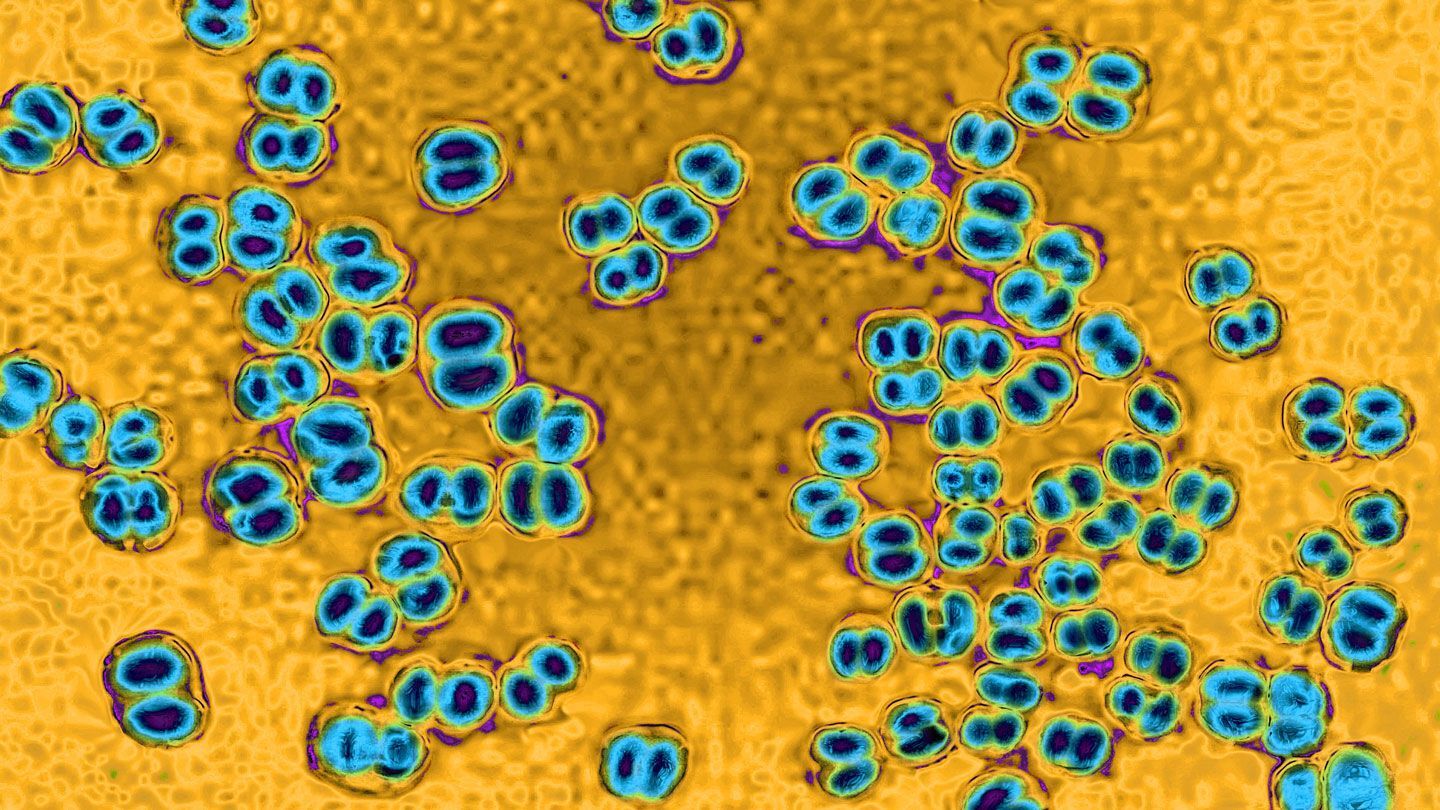
- Causes: The most common causes include Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, and Streptococcus agalactiae (group B streptococcus).
- Transmission: The disease spreads through saliva exchange, such as kissing, sharing drinking containers, utensils, cigarettes, and toothbrushes.
- Symptoms: Common symptoms include high fever, severe headache, rash or purple patches on the skin, vomiting, light sensitivity, stiff neck, confusion, sleepiness, nausea, lethargy, and seizures.
Who is at Risk?
Certain behaviors and living conditions can increase the likelihood of contracting bacterial meningitis. Knowing these risk factors can help in taking preventive measures.
- Risk Factors: Sharing cigarettes, water bottles, eating utensils, food, and kissing, along with living in close quarters like dorms or group homes, heighten the risk.
- Incidence: About 3,000 Americans are affected annually, with 100-125 cases on college campuses, leading to 5-15 deaths among college students each year.
- Mortality Rate: The mortality rate varies from 10-15%, with up to 34% in some cases despite modern antibiotics and improved critical care.
Complications and Long-term Effects
Bacterial meningitis can lead to severe complications if not treated promptly. Understanding these potential outcomes underscores the importance of early diagnosis and treatment.
- Complications: These can include permanent brain damage, kidney failure, learning disabilities, hearing loss, blindness, limb damage requiring amputation, gangrene, coma, and convulsions.
- Neurological Damage: Damage to neurons, especially in hippocampal structures, can cause persistent neuropsychological deficits in survivors.
Treatment and Prevention
Immediate medical attention and preventive measures like vaccination are crucial in managing bacterial meningitis. Here’s what you need to know about treatment and prevention.
- Treatment: Antibiotic treatment is essential and should be administered immediately. Vaccinations are also recommended for those in close quarters, particularly college students 25 years old or younger.
- Vaccine Effectiveness: Vaccines are effective against four of the five most common bacterial types causing 70% of the disease in the U.S., but they do not protect against all types.
- Vaccine Side Effects: The most common side effects are redness and minor pain at the injection site, typically lasting up to two days.
- Vaccine Duration: Vaccination takes 7-10 days to become effective, with protection lasting 3-5 years.
- Vaccine Availability: Vaccination is available at healthcare providers and is very safe.
Diagnosis and Medical Emergency
Early diagnosis and immediate treatment are vital for a better prognosis. Here’s how bacterial meningitis is diagnosed and why it’s considered a medical emergency.
- Diagnosis: Diagnosis is made by a medical provider based on clinical symptoms and lab results from spinal fluid and blood tests.
- Early Diagnosis: Early diagnosis and treatment can greatly improve recovery chances.
- Medical Emergency: Bacterial meningitis is a medical emergency requiring immediate diagnosis and treatment.
Inflammation and Brain Involvement
The inflammation caused by bacterial meningitis affects not just the meninges but also the brain and spinal cord. This section delves into the inflammatory process and its impact on the brain.
- Inflammation: The hallmark of bacterial meningitis is the recruitment of highly activated leukocytes into the cerebrospinal fluid (CSF), leading to inflammation.
- Brain Involvement: The inflammatory process affects the brain parenchyma (meningoencephalitis), the ventricles (ventriculitis), and spreads along the spinal cord.
Epidemiology and Global Impact
The epidemiology of bacterial meningitis has changed over the years, especially with successful vaccination campaigns. However, challenges remain, particularly in resource-poor countries.
- Epidemiology: The epidemiology has dramatically changed over the last 20 years, with Haemophilus influenzae disappearing in developed countries due to successful vaccination campaigns.
- Community-Acquired: Bacterial meningitis is often community-acquired, with common causes including Streptococcus pneumoniae and Neisseria meningitidis.
- Resource-Poor Countries: In resource-poor countries, challenges include underlying diseases like AIDS, tuberculosis, malnutrition, and advanced disease presentation at emergency rooms.
Antibiotic Resistance and Molecular Basis
Understanding the molecular basis of bacterial meningitis and the issue of antibiotic resistance is crucial for developing effective treatments and public health strategies.
- Antibiotic Resistance: The proportion of resistant isolates depends on geographical and other factors, with pneumococci showing up to 35% resistance.
- Molecular Basis: The molecular basis involves specific features of the immune system in the central nervous system (CNS), allowing pathogens to replicate and induce inflammation.
Clinical Features and Diagnosis
The clinical features of bacterial meningitis can vary, making diagnosis challenging. Here’s how medical professionals identify and confirm the disease.
- Clinical Features: Features vary depending on the cause, disease course (acute, subacute, or chronic), brain involvement, and systemic complications like sepsis.
- Initial Diagnosis: Initial diagnosis can be made by clinical examination followed by a lumbar puncture. The diagnosis is supported or confirmed by growing the bacteria from cerebrospinal fluid or blood specimens, rapid diagnostic tests, or polymerase chain reaction (PCR).
Public Health and Surveillance
Effective public health responses and surveillance are essential for controlling bacterial meningitis outbreaks and monitoring trends.
- Serogroups and Susceptibility: Identifying serogroups and antibiotic susceptibility is important for defining control measures. Molecular typing and whole genome sequencing identify more differences between strains and inform public health responses.
- Treatment Variability: Meningitis caused by viruses or bacteria can have similar symptoms, but appropriate treatment and care vary depending on the cause. Bacterial meningitis requires immediate antibiotic treatment.
- Medical Attention: Anyone showing signs or symptoms should seek immediate care at a hospital or health center to verify if they have meningitis, confirm the cause of infection, and determine the right treatment and care.
- Sequelae Impact: Meningitis sequelae can have an enormous impact on individuals, families, and communities both financially and emotionally. Complications such as deafness, learning impairment, or behavioral problems may go untreated if not recognized by carers and healthcare workers.
- Surveillance: Surveillance from case detection to investigation and laboratory confirmation is essential for controlling meningitis. Main objectives include detecting and confirming outbreaks, monitoring incidence trends, estimating disease burden, monitoring antibiotic resistance profiles, and estimating the impact of control strategies.
- Public Health Responses: Public health responses to meningitis outbreaks involve molecular typing and whole genome sequencing to identify more differences between strains and inform public health responses. This helps in defining control measures and preventing further spread of the disease.
Interprofessional Team and Risk Factors
An interprofessional team approach and awareness of risk factors in different age groups are crucial for effective management and prevention of bacterial meningitis.
- Interprofessional Team: An interprofessional team is crucial in caring for patients with bacterial meningitis. This team includes healthcare providers, nurses, and other support staff who work together to improve care coordination and communication to advance treatment, minimize complications, and improve outcomes.
- Risk Factors in Children: In children, risk factors for developing bacterial meningitis include exposure to saliva through sharing utensils or kissing, and living in close conditions such as sharing a room in a dormitory.
- Risk Factors in Adults: In adults, risk factors include certain medical conditions such as a weakened immune system, cerebrospinal fluid leaks, and not having a spleen. Additionally, group settings like college campuses and travel to certain regions increase the risk.
Common Bacterial Causes
Different bacteria can cause meningitis, each with its own risk factors and modes of transmission. Here are some of the most common bacterial causes.
- Group B Streptococcus: Group B streptococcus is a common cause of bacterial meningitis in newborns and young infants, often transmitted during birth.
- Streptococcus pneumoniae: Streptococcus pneumoniae is a leading cause of bacterial meningitis in all age groups, particularly in older adults and those with underlying health conditions.
- Haemophilus influenzae: Haemophilus influenzae type b (Hib) is a significant cause of bacterial meningitis in children, but vaccination has significantly reduced its incidence.
- Neisseria meningitidis: Neisseria meningitidis is a common cause of bacterial meningitis among young adults, particularly in close-knit groups like college students.
- Listeria monocytogenes: Listeria monocytogenes is a less common cause of bacterial meningitis but is particularly dangerous for pregnant women, older adults, and those with weakened immune systems.
- Mycobacterium tuberculosis: Mycobacterium tuberculosis, which causes tuberculosis (TB), is a less common cause of bacterial meningitis but can be transmitted through coughing or sneezing.
- Transmission through Food: Listeria monocytogenes can spread through contaminated food, particularly in individuals who do not wash their hands well after using the toilet.
Prevention and Screening
Preventive measures like vaccination and screening can significantly reduce the risk of bacterial meningitis. Here’s how you can protect yourself and others.
- Prevention through Vaccination: Vaccines are the most effective way to protect against certain types of bacterial meningitis. There are vaccines available for Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae type b, and Mycobacterium tuberculosis.
- Pregnancy Screening: Pregnant women should talk to their healthcare provider about getting screened for group B streptococcus to prevent neonatal infections.
- Importance of Immediate Medical Attention: Bacterial meningitis is a medical emergency requiring immediate attention. Delaying treatment can result in increased intracranial pressure, seizures, coma, and death.
Final Thoughts on Bacterial Meningitis
Bacterial meningitis is a serious condition that demands immediate attention. Knowing the causes, symptoms, and risk factors can save lives. Vaccination remains a key preventive measure, especially for those in close living quarters like college dorms. Early diagnosis and treatment with antibiotics are crucial for recovery. Despite advancements, the mortality rate and potential complications like brain damage and hearing loss highlight the disease's severity. Public health responses and surveillance play vital roles in controlling outbreaks and monitoring antibiotic resistance. Understanding the molecular basis and clinical features helps in better managing the condition. Remember, bacterial meningitis is a medical emergency. If you or someone you know shows symptoms, seek medical help immediately. Stay informed, stay vaccinated, and stay safe.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.