Warfarin is a medication often prescribed to prevent blood clots. But did you know it can have significant effects during pregnancy? Antenatal infection refers to infections that occur before birth, potentially impacting both the mother and the developing baby. Combining these two topics, we delve into the intricate relationship between warfarin use and antenatal infections. Understanding how warfarin interacts with pregnancy and infections is crucial for expecting mothers and healthcare providers. This blog post will provide 25 essential facts about warfarin and antenatal infections, shedding light on their complexities. Whether you're a mom-to-be, a concerned family member, or a medical professional, these facts will help you navigate this important subject.
Key Takeaways:
- Warfarin helps prevent blood clots, but it needs close monitoring and can be affected by diet. Pregnant women may need alternative medications to avoid complications.
- Antenatal infections during pregnancy can have serious implications for both the mother and the baby. Close monitoring and early detection are crucial for preventing complications.
Understanding Warfarin
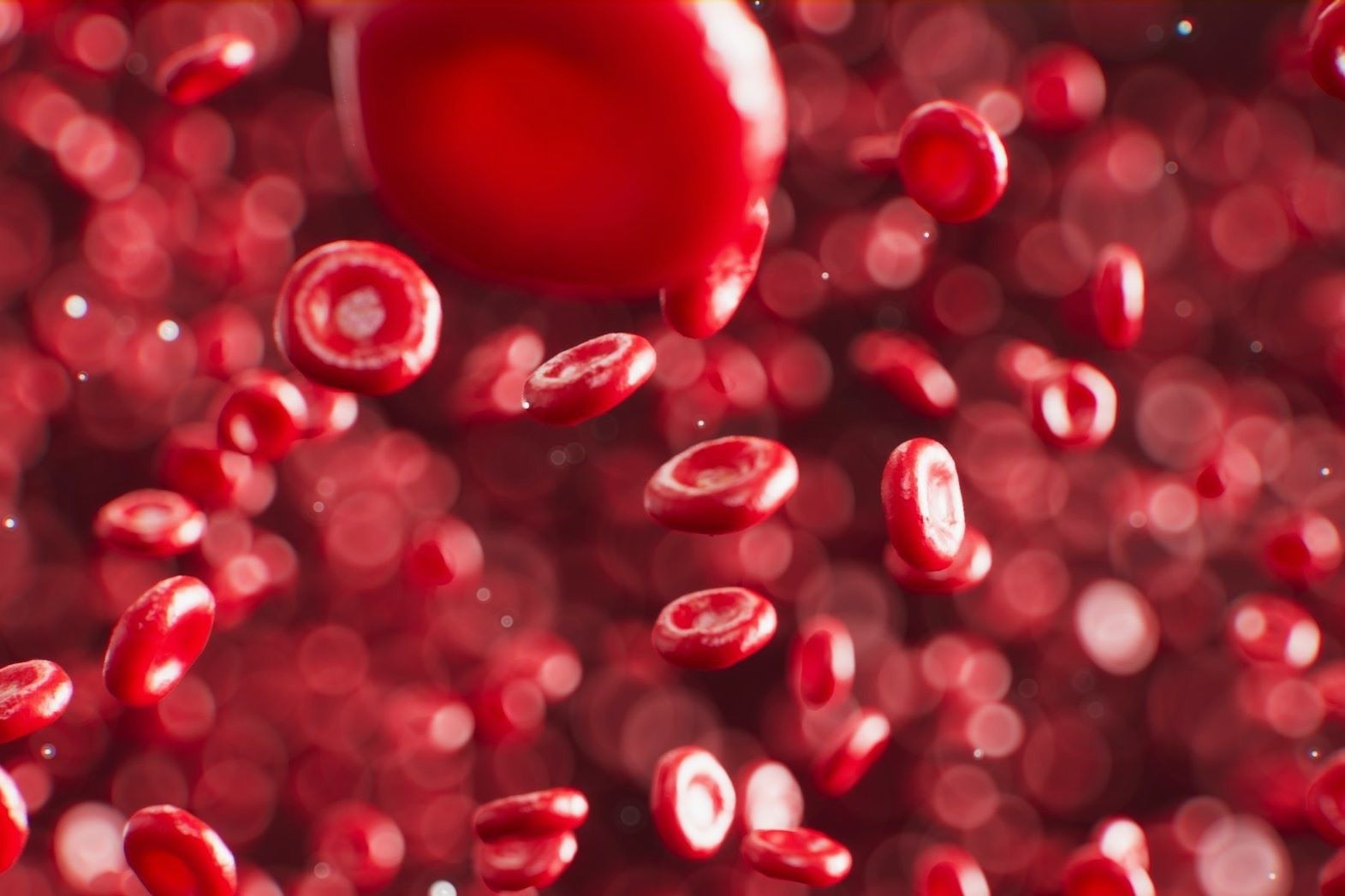
Warfarin is a medication commonly used to prevent blood clots. It's crucial for people with certain heart conditions, but it comes with its own set of facts that are important to know.
-
Warfarin is an anticoagulant. This means it helps prevent blood clots from forming or growing larger.
-
It was originally used as a rat poison. Before its medical use, warfarin was employed to kill rodents.
-
Warfarin requires regular blood tests. Patients need frequent INR (International Normalized Ratio) tests to ensure the dosage is correct.
-
Diet affects warfarin's effectiveness. Foods high in vitamin K, like leafy greens, can interfere with its action.
-
It has a narrow therapeutic range. This means the difference between an effective dose and a harmful dose is small.
Warfarin and Pregnancy
Warfarin use during pregnancy is a complex issue. It can have significant effects on both the mother and the developing fetus.
-
Warfarin can cross the placenta. This means it can affect the developing baby.
-
It is classified as a Category X drug. This classification indicates that it can cause birth defects.
-
Warfarin embryopathy is a risk. This condition includes nasal hypoplasia and stippled epiphyses in the fetus.
-
First trimester is the most critical. The risk of birth defects is highest during the first 12 weeks of pregnancy.
-
Alternatives are often recommended. Heparin is usually preferred during pregnancy because it does not cross the placenta.
Antenatal Infections
Antenatal infections are infections that occur during pregnancy. They can have serious implications for both the mother and the baby.
-
Common antenatal infections include TORCH. TORCH stands for Toxoplasmosis, Other (syphilis, varicella-zoster, parvovirus B19), Rubella, Cytomegalovirus, and Herpes simplex virus.
-
Infections can lead to congenital anomalies. These are structural or functional anomalies that occur during intrauterine life.
-
Some infections can cause preterm labor. This can lead to complications for the newborn.
-
Screening is essential. Early detection and treatment can prevent many complications.
-
Vaccination can prevent some infections. For example, the rubella vaccine can prevent congenital rubella syndrome.
Warfarin and Antenatal Infections
Combining the topics of warfarin and antenatal infections reveals some unique challenges and considerations.
-
Warfarin can complicate infection treatment. Its anticoagulant properties can make managing infections more difficult.
-
Infections can alter warfarin metabolism. This can affect how the drug works and its dosage requirements.
-
Pregnant women on warfarin need close monitoring. Both the infection and the medication require careful management.
-
Antibiotics can interact with warfarin. Some antibiotics can increase or decrease warfarin's effectiveness.
-
Infection-induced inflammation can affect INR levels. This makes it harder to maintain the correct warfarin dose.
Managing Risks
Managing the risks associated with warfarin and antenatal infections involves a multidisciplinary approach.
-
Regular check-ups are crucial. Frequent visits to healthcare providers help monitor both the mother and the baby.
-
Patient education is key. Understanding the risks and how to manage them can improve outcomes.
-
Alternative medications may be necessary. In some cases, switching from warfarin to another anticoagulant is the best option.
-
Close collaboration between specialists. Obstetricians, hematologists, and infectious disease specialists often work together.
-
Personalized care plans. Each patient's situation is unique, requiring tailored treatment plans.
Final Thoughts on Warfarin Antenatal Infection
Warfarin, a common anticoagulant, has significant implications during pregnancy. Understanding its effects on antenatal infection is crucial for both expectant mothers and healthcare providers. Warfarin can cross the placenta, potentially leading to complications such as fetal bleeding, congenital abnormalities, and even miscarriage. Close monitoring and alternative treatments might be necessary to ensure the safety of both mother and baby.
Pregnant women on warfarin should work closely with their healthcare team to manage their condition effectively. Regular check-ups, blood tests, and possibly switching to safer anticoagulants like heparin during pregnancy can help mitigate risks. Awareness and proactive management are key to navigating the challenges associated with warfarin use during pregnancy.
By staying informed and vigilant, expectant mothers can better protect their health and the health of their unborn child, ensuring a safer pregnancy journey.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.