Microphthalmia-Dermal Aplasia-Sclerocornea Syndrome (MLS), also known as MIDAS syndrome, is a rare genetic disorder that primarily affects females. This condition is characterized by microphthalmia (small or underdeveloped eyes), linear skin defects, and sclerocornea (opaque corneas). Caused by mutations in the HCCS gene, MLS syndrome follows an X-linked dominant inheritance pattern, meaning a single copy of the mutated gene can cause the disorder. Males with the mutation are typically not viable in utero. The syndrome's manifestations can vary widely, including congenital heart defects, brain abnormalities, and microcephaly. Understanding MLS syndrome's genetic basis, clinical features, and management strategies is crucial for providing comprehensive care to affected individuals and their families.
What is Microphthalmia-Dermal Aplasia-Sclerocornea Syndrome?
Microphthalmia-Dermal Aplasia-Sclerocornea Syndrome, also known as MLS or MIDAS syndrome, is a rare genetic disorder. It primarily affects females and is characterized by unique eye and skin abnormalities. Let's dive into the details.
-
Definition and Classification: MLS syndrome is an X-linked dominant condition. This means a single copy of the mutated gene on the X chromosome can cause the disorder.
-
Ocular Defects: The main eye issue is microphthalmia, where one or both eyes are underdeveloped or small. This can range from mild to severe, with some cases resulting in anophthalmia, where the eye is completely absent.
-
Linear Skin Defects: Affected individuals often have linear skin defects that follow the lines of Blaschko. These lesions, usually on the face and neck, may turn into hyperpigmented areas over time.
-
Sclerocornea: Sclerocornea is when the cornea, normally clear, becomes opaque. This condition is common in MLS syndrome and can further complicate vision.
Genetic Basis and Inheritance
Understanding the genetic roots of MLS syndrome helps in diagnosing and managing the condition. Here's what you need to know.
-
Genetic Basis: MLS syndrome is mainly caused by mutations in the HCCS gene. This gene is crucial for mitochondrial function, and its mutation leads to the syndrome's symptoms.
-
X-Chromosome Inactivation: Females with MLS often show skewed X-chromosome inactivation. This means one X chromosome is inactivated more than the other, leading to a mix of cells with and without the mutation.
-
Male Lethality: Males with the mutation usually do not survive in utero due to the lack of a second X chromosome to compensate. This makes MLS an X-linked dominant condition with male lethality.
-
Inheritance Pattern: MLS syndrome follows an X-linked dominant inheritance pattern. Females with one mutated HCCS gene can pass it to their offspring, who will be affected if they inherit the gene.
Clinical Manifestations
MLS syndrome presents a wide range of symptoms, affecting various parts of the body. Here are the key clinical features.
-
Clinical Spectrum: The symptoms of MLS syndrome vary widely. Common issues include microphthalmia, sclerocornea, linear skin defects, and systemic abnormalities like heart defects and brain issues.
-
Additional Ocular Anomalies: Other eye problems may include iris coloboma, corneal clouding, and chorioretinal abnormalities, which can further impact vision.
-
Cardiac Defects: Congenital heart defects are common in MLS syndrome. These can range from mild to severe, including atrial septal defects (ASD) and ventricular septal defects (VSD).
-
Brain Imaging Abnormalities: Brain scans may show issues like agenesis of the corpus callosum and hydrocephalus, affecting cognitive and motor development.
-
Microcephaly: Some individuals have microcephaly, or a small head size, which can be linked to intellectual disability and developmental delays.
-
Intellectual Disability: Intellectual disability can vary from mild to severe in MLS syndrome, often associated with other systemic abnormalities.
-
Nail Dystrophy: Nail dystrophy, or abnormal fingernails and toenails, is another feature. This can show up as nail hypoplasia or other nail issues.
-
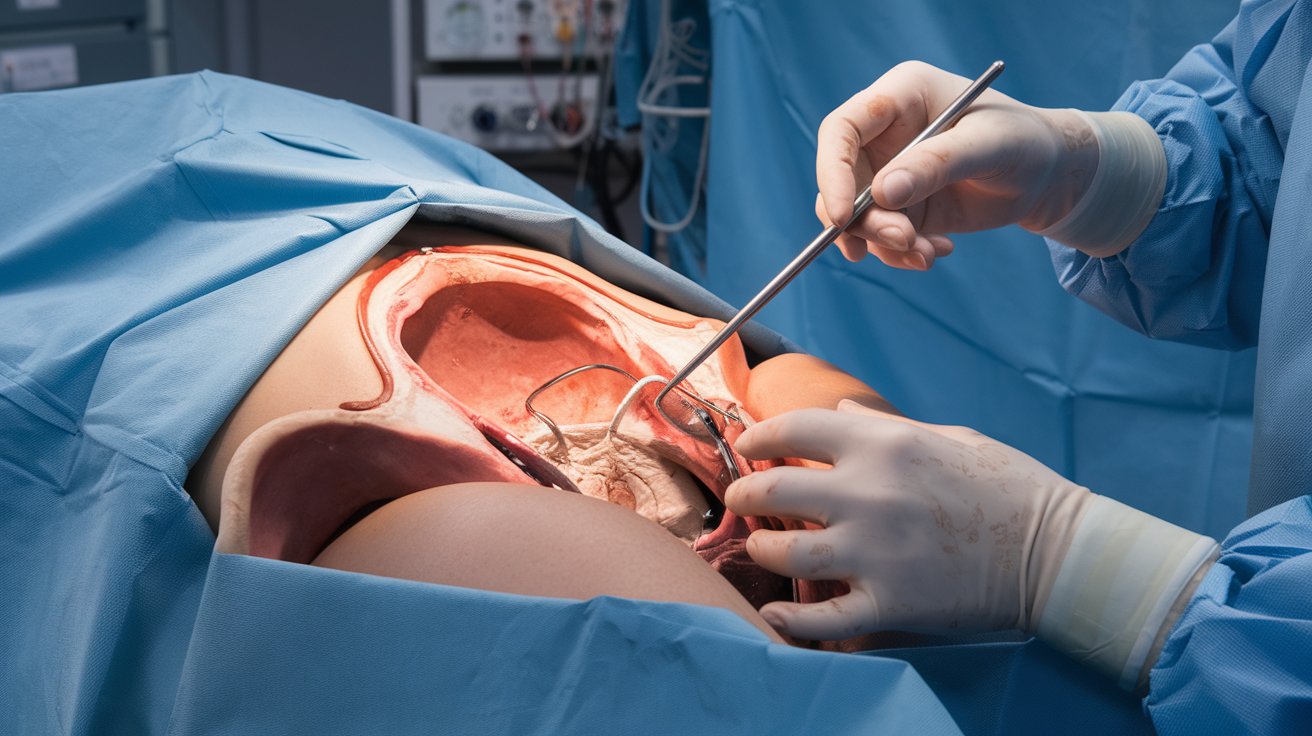
Diaphragmatic Hernia: A diaphragmatic hernia, where the diaphragm doesn't form properly, can occur, leading to respiratory and gastrointestinal problems.
Diagnosis and Management
Diagnosing and managing MLS syndrome involves a combination of clinical examination and genetic testing. Here's how it's done.
-
Prevalence: MLS syndrome is rare, with over 50 identified cases. This rarity underscores the importance of genetic counseling and diagnosis.
-
Diagnostic Criteria: Diagnosis relies on clinical examination and genetic testing. Techniques like cytogenetic analysis, FISH, sequencing, and PCR help identify the HCCS mutation.
-
Genetic Testing: Genetic testing is key for confirming the diagnosis. It involves analyzing the HCCS gene for mutations. In some cases, other genes like COX7B may also be involved.
-
Management and Treatment: There's no specific treatment for MLS syndrome. Management focuses on addressing systemic complications and improving quality of life, including surgical interventions and supportive care.
-
Prognosis: The prognosis varies widely. Those with severe systemic complications may have a poorer outlook compared to those with milder symptoms.
Support and Future Directions
Support and ongoing research are crucial for families affected by MLS syndrome. Here's what the future holds.
-
Family Counseling: Given the inheritance pattern, family counseling is essential. Females who are carriers need to understand the risks for their offspring. Prenatal testing can help determine if a fetus is affected.
-
Research and Advances: Ongoing research aims to understand the molecular mechanisms of MLS syndrome better. This includes studies on mitochondrial function and the role of HCCS in oxidative phosphorylation.
-
Support and Resources: Support groups and resources are vital for affected families. Organizations like Orphanet and MedlinePlus offer valuable information and support.
-
Future Directions: Future research may lead to targeted therapies to improve mitochondrial function. Advances in genetic engineering and gene therapy could offer new treatment avenues. Continued research will help develop better management strategies.
Understanding MLS Syndrome
Microphthalmia-Dermal Aplasia-Sclerocornea Syndrome, or MLS, is a rare genetic disorder affecting mainly females. It involves underdeveloped eyes, linear skin defects, and opaque corneas. Caused by mutations in the HCCS gene, MLS leads to various systemic issues like heart defects and brain abnormalities. Diagnosis relies on clinical examination and genetic testing. Management focuses on treating symptoms and improving quality of life. Genetic counseling is crucial for families due to the X-linked dominant inheritance pattern. Research continues to explore better treatments and understanding of the syndrome. Support groups and resources play a vital role in helping affected families navigate this challenging condition. Understanding MLS syndrome's complexities can lead to better care and support for those affected.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.