Coarctation of the Aorta (CoA) is a congenital heart defect where the aorta, the main artery carrying blood from the heart, narrows. This condition affects 4-6% of all congenital heart defects, with an incidence of 3-4 cases per 10,000 live births. Symptoms can range from difficulty breathing and feeding in infants to high blood pressure, chest pain, and leg cramps in older children and adults. Diagnosis often involves physical exams, echocardiograms, and imaging tests like MRI or CT scans. Treatment options include surgical repair, balloon angioplasty, and stent implantation. Early diagnosis and lifelong care are crucial for managing this condition effectively.
Key Takeaways:
- Coarctation of the aorta is a narrowing of the heart's main blood vessel. It can cause serious symptoms and requires lifelong care to manage potential complications and improve patient outcomes.
- Early diagnosis and proper treatment are crucial for managing coarctation of the aorta. Lifelong cardiovascular care and monitoring are essential for patients, and genetic associations and natural disease progression should be considered.
Understanding Coarctation of the Aorta
Coarctation of the aorta (CoA) is a congenital heart defect that can have serious implications if not properly managed. Let's dive into some essential facts about this condition.
-
Definition and Prevalence
Coarctation of the aorta is a congenital narrowing of the aorta. It accounts for 4-6% of all congenital heart defects, with an incidence of 3-4 cases per 10,000 live births. -
Causes
The exact cause remains unclear, but it likely results from errors in cell migration, differentiation, and programmed cell death during embryonic development. Genetic factors also play a role, as CoA is more common in males.
Symptoms of Coarctation of the Aorta
Symptoms can vary widely depending on the severity of the narrowing. Here are some common signs to watch for.
-
Infant Symptoms
Infants may experience difficulty breathing, feeding issues, heavy sweating, irritability, and changes in skin color. -
Older Children and Adults
In older children and adults, symptoms may include chest pain, high blood pressure, headaches, muscle weakness, leg cramps, and cold feet.
Diagnosing Coarctation of the Aorta
Early and accurate diagnosis is crucial for effective treatment. Here are some methods used to diagnose CoA.
-
Physical Examination
A doctor may find higher blood pressures in the arms compared to the legs, a heart murmur, and weak or hard-to-feel pulses in the groin area. -
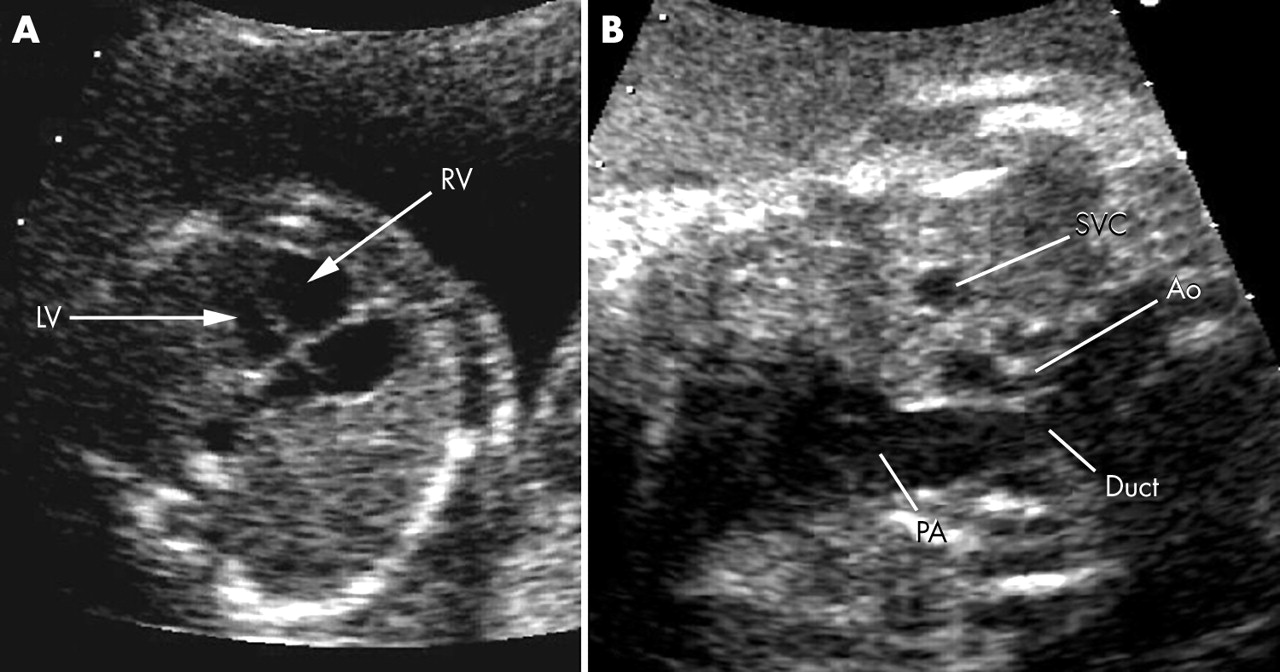
Echocardiograms
Echocardiograms use sound waves to create images of the heart, helping to visualize the narrowing. -
Chest X-rays
Chest X-rays can show an enlarged heart or rib notching, which are indicative of CoA. -
MRI and CT Scans
Magnetic resonance imaging (MRI) and computerized tomography (CT) scans provide detailed images of the heart and aorta.
Treatment Options for Coarctation of the Aorta
Treatment usually involves surgical or minimally invasive procedures to correct the narrowing. Here are some common methods.
-
Surgical Repair
Surgical repair involves removing the narrowed section of the aorta and reconnecting the two ends. This is typically done in infancy or early childhood. -
Balloon Angioplasty
A minimally invasive procedure where a balloon is inserted and inflated to widen the narrowed area. -
Stent Implantation
Stents are small, mesh-like devices inserted into the aorta to keep it open after balloon angioplasty. -
Endovascular Technology
Advances in endovascular technology have made nonsurgical approaches possible for older children and adults.
Long-term Management and Complications
Managing CoA doesn't end with treatment. Long-term care is essential to monitor and manage potential complications.
-
High Blood Pressure
High blood pressure is common in CoA patients, even after treatment, and requires ongoing management. -
Cardiovascular Complications
CoA increases the risk of cardiovascular issues like persistent hypertension, vascular dysfunction, and coronary disease. -
Regular Monitoring
Regular blood pressure checks and periodic reassessment with echocardiography and three-dimensional imaging are crucial. -
Genetic Associations
CoA is often associated with other congenital heart defects and genetic conditions like Turner syndrome. -
Aortopathy
Abnormalities of the aorta can lead to dilation and aneurysm formation, requiring close monitoring.
Special Considerations
Certain factors can complicate the management of CoA. Here are some special considerations to keep in mind.
-
Natural Disease Progression
As patients age, complications from the disease and its treatment become more apparent. -
Prenatal Detection
Improved prenatal detection has significantly improved treatment outcomes. -
Neurodevelopmental Concerns
CoA can be associated with neurodevelopmental issues, requiring early detection and management. -
Pregnancy-Related Issues
Pregnancy can exacerbate CoA, necessitating close monitoring by a cardiologist. -
Optimizing Health
Optimizing arterial, endothelial, and fluid mechanics is essential to reduce the incidence of recurrence and other complications.
Lifelong Care and Prognosis
Lifelong care is essential for managing CoA and improving patient outcomes.
-
Lifelong Cardiovascular Care
All CoA patients benefit from lifelong care by a cardiologist familiar with the disease. -
Reduced Life Expectancy
Patients with CoA have a reduced life expectancy and increased risk of cardiovascular complications. -
Increased Risk of Coronary Disease
Persistent hypertension and vascular dysfunction can lead to an increased risk of coronary disease, the greatest cause of long-term mortality in CoA patients.
Key Takeaways on Coarctation of the Aorta
Coarctation of the aorta (CoA) is a serious congenital heart defect that requires early diagnosis and lifelong management. This condition, marked by the narrowing of the aorta, can lead to high blood pressure, cardiovascular complications, and reduced life expectancy if not treated properly. Surgical repair, balloon angioplasty, and stent implantation are common treatments that have significantly improved outcomes. Regular checkups and monitoring are essential for managing long-term risks, including hypertension and coronary disease. Advances in prenatal detection and endovascular technology have also enhanced treatment options, making early intervention more effective. Understanding the genetic associations and potential complications helps in providing comprehensive care. Lifelong cardiovascular care by a knowledgeable cardiologist is crucial for anyone with CoA. Early diagnosis and proper management can greatly improve quality of life and reduce the risk of severe complications.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.