What is Chronic Demyelinating Neuropathy with IgM Monoclonal? It's a rare neurological disorder where the immune system produces an abnormal IgM monoclonal protein, damaging the myelin sheath that protects nerve fibers. This leads to symptoms like weakness, numbness, and tingling in the limbs. Often seen in patients with lymphoproliferative disorders, it disrupts nerve conduction, causing significant discomfort and disability. Diagnosing this condition involves clinical evaluations, lab tests, and electrophysiological studies. Treatment focuses on symptom management and addressing the underlying cause, often involving plasma exchange, immunosuppressive medications, and rituximab. Understanding this condition is crucial for effective management and improving patient outcomes.
Key Takeaways:
- Chronic Demyelinating Neuropathy with IgM Monoclonal is a rare condition causing nerve damage. It's diagnosed through lab tests and treated with therapies like plasma exchange and immunosuppressive medications.
- Research and patient support are essential for improving Chronic Demyelinating Neuropathy with IgM Monoclonal management. Clinical trials and support groups offer hope for better treatments and emotional support.
Understanding Chronic Demyelinating Neuropathy with IgM Monoclonal
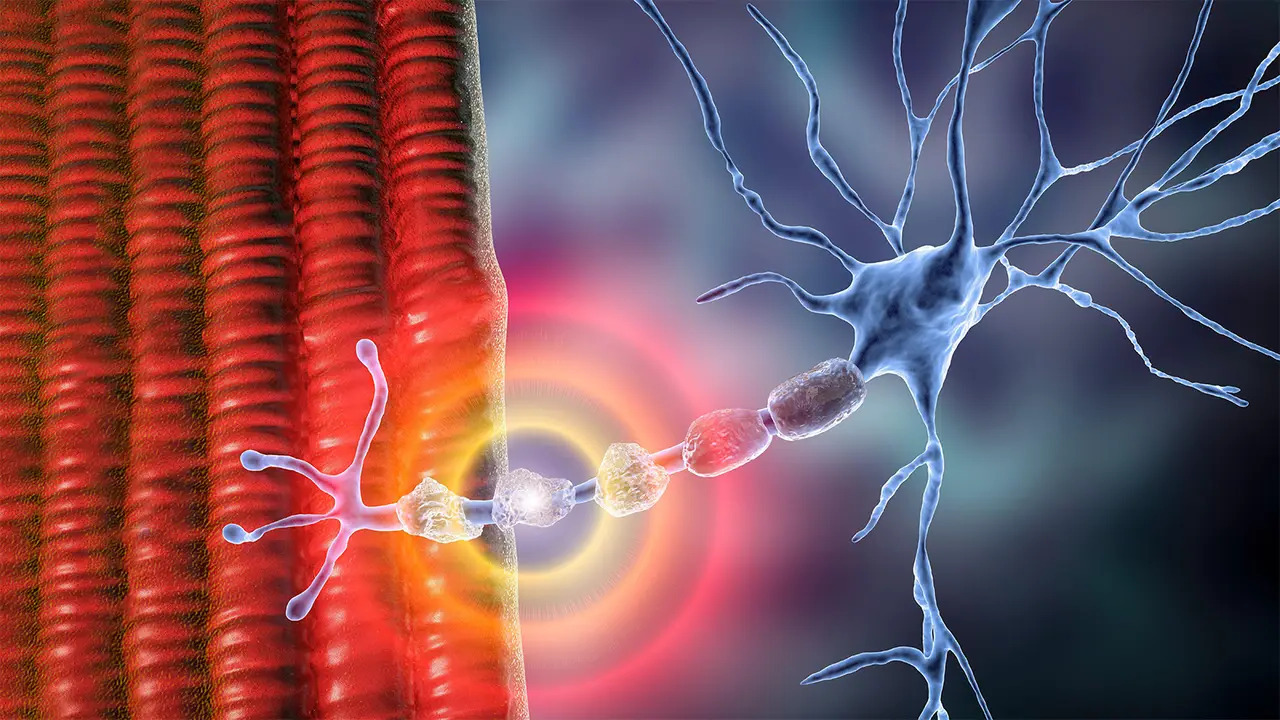
Chronic demyelinating neuropathy with IgM monoclonal (CDMN) is a rare neurological disorder. It involves the immune system producing an abnormal IgM monoclonal protein, which damages the myelin sheath around nerve fibers. Let's dive into some essential facts about this condition.
-
Definition: CDMN is a type of peripheral neuropathy where the immune system creates an abnormal IgM monoclonal protein, leading to chronic demyelination of nerve fibers.
-
Incidence: This condition is relatively rare. It's often seen in patients with lymphoproliferative disorders like lymphoma or chronic lymphocytic leukemia (CLL).
-
Symptoms: Symptoms vary but typically include progressive weakness, numbness, and tingling in limbs, especially hands and feet. Muscle atrophy, loss of reflexes, and autonomic dysfunction are also common.
Pathophysiology and Diagnosis
Understanding how CDMN affects the body and how it's diagnosed is crucial for managing the condition effectively.
-
Pathophysiology: The abnormal IgM monoclonal protein targets and damages the myelin sheath, disrupting nerve conduction and causing neuropathy symptoms.
-
Diagnostic Criteria: Diagnosis is based on clinical presentation, lab findings showing IgM monoclonal protein, and electrophysiological studies demonstrating demyelination.
-
Electrophysiological Studies: Electromyography (EMG) and nerve conduction studies (NCS) are key diagnostic tools. They reveal demyelination signs like prolonged distal latencies and conduction block.
-
Imaging Studies: MRI and CT scans aren't specific for diagnosing CDMN but help rule out other conditions with similar symptoms.
-
Laboratory Tests: Important tests include serum protein electrophoresis (SPEP) to detect monoclonal proteins, immunofixation electrophoresis (IFE) to identify specific monoclonal proteins, and serum immunoglobulin levels.
Key Laboratory Tests
Laboratory tests play a significant role in diagnosing CDMN. They help identify the presence and type of abnormal proteins in the blood.
-
Serum Protein Electrophoresis (SPEP): SPEP separates serum proteins by size and charge, identifying abnormal proteins like monoclonal immunoglobulins.
-
Immunofixation Electrophoresis (IFE): IFE is more sensitive than SPEP and can specifically identify the type of monoclonal protein in the serum.
-
Serum Immunoglobulin Levels: Elevated IgM levels are often seen in CDMN patients.
-
Bone Marrow Biopsy: Sometimes, a bone marrow biopsy is performed to check for underlying lymphoproliferative disorders.
Treatment Options
Treating CDMN focuses on managing symptoms and addressing the underlying cause. Various therapeutic options are available.
-
Plasma Exchange: This procedure removes plasma from the blood to reduce monoclonal protein levels and temporarily alleviate symptoms.
-
Immunosuppressive Medications: Drugs like cyclophosphamide, cyclosporine, and prednisone suppress the immune system, reducing abnormal protein production.
-
Rituximab: Rituximab is a monoclonal antibody targeting CD20-positive B cells, helping reduce IgM monoclonal protein production.
-
Symptomatic Management: Includes physical therapy to maintain muscle strength, pain management strategies, and supportive care for autonomic dysfunction.
Prognosis and Complications
The prognosis for CDMN varies widely. Understanding potential complications helps in managing the condition better.
-
Prognosis: Prognosis depends on the underlying cause and response to treatment. Some patients improve significantly with therapy, while others may worsen despite treatment.
-
Complications: Untreated or inadequately treated CDMN can lead to severe disability due to progressive muscle weakness, autonomic dysfunction, and increased infection risk from immunosuppression.
Differential Diagnosis and Factors
Differentiating CDMN from other conditions and understanding genetic and environmental factors is essential for accurate diagnosis and treatment.
-
Differential Diagnosis: Includes other peripheral neuropathies like chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), Guillain-Barré syndrome, and hereditary neuropathies like Charcot-Marie-Tooth disease.
-
Genetic Factors: While genetic factors aren't directly implicated in CDMN, some patients may have genetic predispositions contributing to lymphoproliferative disorders.
-
Environmental Factors: No known environmental factors directly cause CDMN. However, exposure to certain chemicals or infections might trigger an immune response in susceptible individuals.
Research and Support
Ongoing research and patient support are crucial for improving CDMN management and patient outcomes.
-
Clinical Trials: Limited clinical trials specifically target CDMN due to its rarity. Research into treatments for related conditions like CIDP provides valuable insights.
-
Patient Support Groups: These groups offer emotional support and connect patients with similar conditions. They facilitate sharing experiences, managing symptoms, and accessing resources.
-
Future Research Directions: Future research aims to develop more targeted therapies for reducing monoclonal protein production and improving patient quality of life. Better understanding of CDMN's pathophysiology could lead to more effective diagnostic tools and treatments.
-
Continued Research: Ongoing studies are essential for uncovering new treatment strategies and improving outcomes for patients with this rare disorder.
Final Thoughts on Chronic Demyelinating Neuropathy with IgM Monoclonal
Chronic demyelinating neuropathy with IgM monoclonal is a rare, complex condition that affects the nervous system. It involves an abnormal IgM monoclonal protein attacking the myelin sheath, leading to symptoms like weakness, numbness, and tingling in the limbs. Diagnosis relies on clinical presentation, lab tests, and electrophysiological studies. Treatment focuses on managing symptoms and addressing underlying causes, often involving plasma exchange, immunosuppressive meds, and rituximab. Prognosis varies widely, with some patients improving significantly while others face progressive worsening. Complications can include severe disability and increased infection risk. Understanding and managing this condition requires a comprehensive approach, combining symptom relief with targeted therapies. Ongoing research and patient support groups play crucial roles in improving outcomes and quality of life for those affected.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


