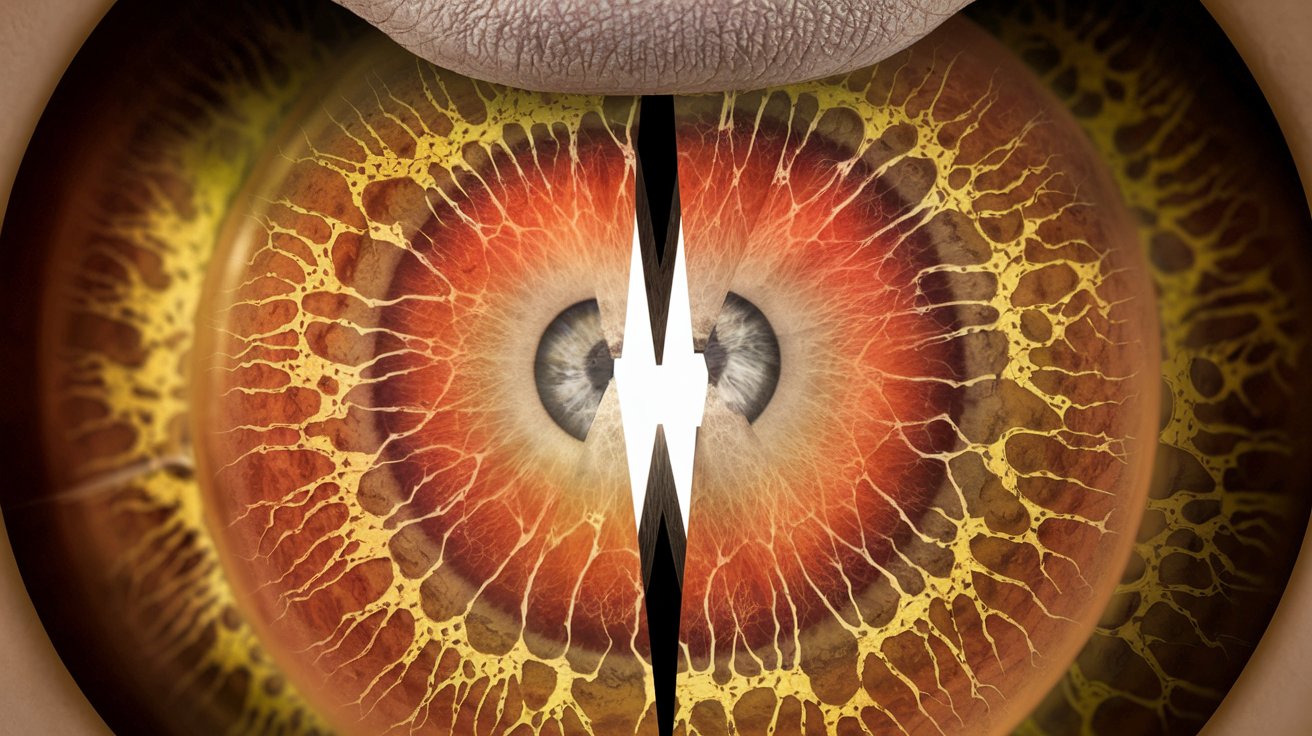
Retinoschisis is a rare eye condition that affects the retina, causing it to split into two layers. This can lead to vision problems, including blurred vision and difficulty seeing in low light. Retinoschisis can be inherited or acquired, with the inherited form often appearing in childhood and the acquired form typically developing in older adults. Understanding this condition is crucial for early detection and management. In this blog post, we will explore 50 fascinating facts about Retinoschisis, shedding light on its causes, symptoms, treatments, and much more. Whether you're a patient, a caregiver, or simply curious, you'll find valuable information to help you navigate this complex condition.
Key Takeaways:
- Retinoschisis is a rare eye condition where the retina splits, causing vision problems. Early diagnosis and regular eye exams are crucial for managing the symptoms and seeking support when needed.
- Understanding the causes and risk factors of retinoschisis can help identify those at risk and take preventive measures. Genetic mutations, aging, and high myopia are significant risk factors.
What is Retinoschisis?
Retinoschisis is a rare eye condition where the retina splits into two layers. This can lead to vision problems and, in severe cases, blindness. Understanding this condition can help in managing it better.
- Retinoschisis is derived from Greek words meaning "split retina."
- It primarily affects the peripheral retina, the part responsible for side vision.
- The condition can be congenital (present at birth) or acquired later in life.
- Juvenile retinoschisis is the most common form, affecting young boys.
- Adult-onset retinoschisis usually occurs in people over 50.
Symptoms of Retinoschisis
Recognizing the symptoms early can lead to better management and treatment options. Here are some common signs to watch for.
- Vision loss, particularly in the peripheral vision.
- Floaters, which are small shapes that drift across your field of vision.
- Flashing lights, often seen in the peripheral vision.
- Difficulty seeing in low light conditions.
- A sensation of a "curtain" over part of the visual field.
Causes and Risk Factors
Understanding what causes retinoschisis can help in identifying those at risk and taking preventive measures.
- Genetic mutations are a primary cause, especially in juvenile retinoschisis.
- X-linked inheritance means the condition is passed from mother to son.
- Aging is a significant risk factor for adult-onset retinoschisis.
- High myopia (nearsightedness) increases the risk.
- Trauma to the eye can also lead to retinoschisis.
Diagnosis of Retinoschisis
Early diagnosis is crucial for managing retinoschisis effectively. Here are some methods used by eye specialists.
- Ophthalmoscopy allows doctors to examine the retina directly.
- Optical coherence tomography (OCT) provides detailed images of the retina.
- Visual field tests measure peripheral vision loss.
- Electroretinography (ERG) assesses the electrical activity of the retina.
- Genetic testing can confirm juvenile retinoschisis.
Treatment Options
While there's no cure for retinoschisis, various treatments can help manage the symptoms and slow progression.
- Regular eye exams are essential for monitoring the condition.
- Laser therapy can seal retinal tears and prevent further splitting.
- Vitrectomy surgery removes the vitreous gel to relieve traction on the retina.
- Scleral buckling surgery helps reattach the retina.
- Low vision aids, like magnifying glasses, can improve quality of life.
Living with Retinoschisis
Managing daily life with retinoschisis involves adapting to vision changes and seeking support when needed.
- Using bright lighting can help with low light vision difficulties.
- Large-print books and digital devices with adjustable text sizes are beneficial.
- Mobility training can help navigate safely with peripheral vision loss.
- Support groups provide emotional and practical support.
- Regular follow-ups with an eye specialist are crucial.
Research and Future Directions
Ongoing research aims to find better treatments and possibly a cure for retinoschisis. Here are some promising areas.
- Gene therapy is being explored to correct genetic mutations.
- Stem cell therapy could potentially regenerate damaged retinal cells.
- New imaging techniques are improving early diagnosis.
- Clinical trials are testing new medications to slow disease progression.
- Advances in surgical techniques are reducing complications.
Interesting Facts about Retinoschisis
Here are some lesser-known but fascinating facts about this eye condition.
- Retinoschisis was first described in medical literature in the 19th century.
- It affects approximately 1 in 5,000 to 1 in 25,000 people.
- The condition is more common in males due to its X-linked inheritance.
- Some people with retinoschisis may never experience significant vision loss.
- Early intervention can significantly improve outcomes.
Preventive Measures
While not all cases of retinoschisis can be prevented, certain measures can reduce the risk or delay onset.
- Regular eye exams can catch early signs before symptoms appear.
- Protecting eyes from trauma can prevent acquired retinoschisis.
- Managing high myopia with corrective lenses or surgery can reduce risk.
- Genetic counseling can help families understand their risk.
- Maintaining overall eye health with a balanced diet and avoiding smoking is beneficial.
Myths and Misconceptions
Clearing up common myths can help people better understand and manage retinoschisis.
- Retinoschisis is not the same as retinal detachment, though they can occur together.
- It is not caused by poor eye hygiene or excessive screen time.
- Wearing glasses or contact lenses does not cause retinoschisis.
- The condition is not contagious and cannot be spread from person to person.
- Early diagnosis and treatment can significantly improve quality of life, contrary to the belief that nothing can be done.
Final Thoughts on Retinoschisis
Retinoschisis, a condition affecting the retina, can lead to vision problems if not monitored. Knowing the symptoms like blurred vision or floaters helps in early detection. Regular eye exams are crucial for those at risk, especially if there's a family history. Treatments range from observation to surgery, depending on severity. Advances in medical research offer hope for better management and potential cures. Staying informed about retinoschisis empowers patients and caregivers to make educated decisions. Remember, early intervention can make a significant difference. If you suspect any issues with your vision, consult an eye specialist promptly. Taking proactive steps ensures better eye health and quality of life. Keep learning and stay vigilant about your eye health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
