Pigmented Villonodular Synovitis (PVNS) is a rare joint disease that causes the lining of joints and tendons to thicken and overgrow. This condition can lead to pain, swelling, and reduced mobility. PVNS typically affects the knee or hip but can occur in any joint. The exact cause remains unknown, though some researchers believe it may be linked to genetic mutations. Treatment options include surgery, radiation, or medication to manage symptoms and prevent recurrence. Understanding PVNS is crucial for early diagnosis and effective treatment. Here are 50 facts to help you grasp the essentials of this uncommon yet impactful condition.
Key Takeaways:
- Pigmented Villonodular Synovitis (PVNS) is a rare joint disease causing pain and swelling. It can affect any joint but is most common in the knee and hip, and is more prevalent in adults aged 20 to 50.
- Early detection and personalized treatment plans are crucial for managing PVNS. Surgical removal of affected tissue, radiation therapy, and physical therapy are common approaches. Ongoing research offers hope for improved understanding and treatment.
What is Pigmented Villonodular Synovitis?
Pigmented Villonodular Synovitis (PVNS) is a rare joint disease that causes the synovium, the lining of the joints, to thicken and overgrow. This condition can lead to pain, swelling, and reduced mobility. Here are some intriguing facts about PVNS.
-
PVNS is classified as a benign tumor, meaning it is not cancerous but can still cause significant problems.
-
The disease can affect any joint but is most commonly found in the knee and hip.
-
PVNS is more prevalent in adults aged 20 to 50, though it can occur at any age.
-
The exact cause of PVNS remains unknown, but some researchers believe it may be related to inflammation or trauma.
-
There are two types of PVNS: localized and diffuse. Localized PVNS affects a small area, while diffuse PVNS involves the entire synovium.
Symptoms and Diagnosis of PVNS
Recognizing the symptoms of PVNS early can lead to better management of the condition. Here are some key symptoms and diagnostic methods.
-
Common symptoms include joint pain, swelling, and stiffness.
-
Some patients may experience a locking or catching sensation in the affected joint.
-
PVNS can lead to decreased range of motion in the affected joint.
-
In severe cases, the disease can cause joint destruction and arthritis.
-
Diagnosis typically involves imaging tests such as MRI or X-rays to visualize the affected joint.
-
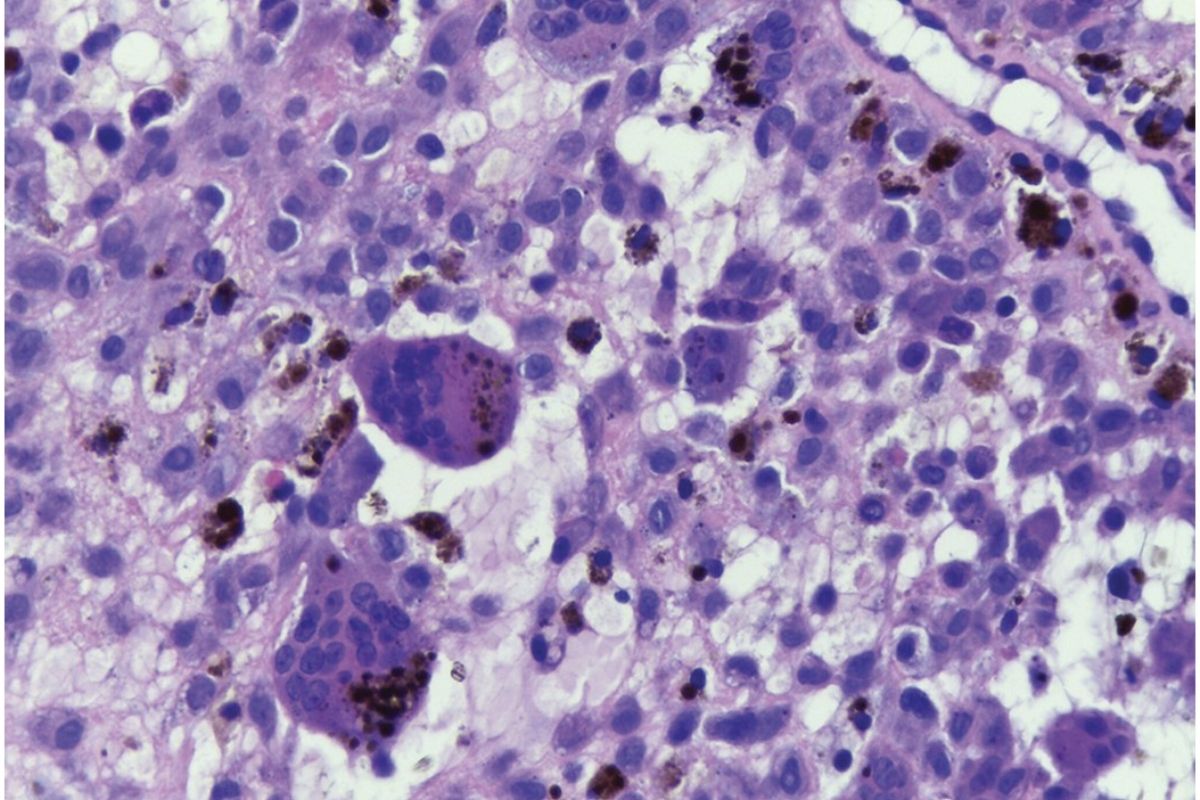
A biopsy may be performed to confirm the diagnosis by examining the synovial tissue under a microscope.
Treatment Options for PVNS
Managing PVNS often requires a combination of treatments. Here are some common approaches.
-
Surgical removal of the affected synovium is the primary treatment for PVNS.
-
Arthroscopic surgery, a minimally invasive procedure, is often used to treat localized PVNS.
-
Open surgery may be necessary for diffuse PVNS to ensure complete removal of the affected tissue.
-
Radiation therapy can be used to reduce the risk of recurrence after surgery.
-
Some patients may benefit from physical therapy to improve joint function and mobility.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage pain and inflammation.
Prognosis and Recurrence
Understanding the prognosis and potential for recurrence is crucial for PVNS patients. Here are some important facts.
-
The prognosis for PVNS is generally good with appropriate treatment.
-
Recurrence rates vary, with localized PVNS having a lower recurrence rate compared to diffuse PVNS.
-
Regular follow-up appointments are essential to monitor for signs of recurrence.
-
Early detection of recurrence can lead to more effective treatment and better outcomes.
-
In some cases, multiple surgeries may be required to manage recurrent PVNS.
Research and Future Directions
Ongoing research aims to improve the understanding and treatment of PVNS. Here are some exciting developments.
-
Researchers are investigating the genetic and molecular basis of PVNS to identify potential targets for new therapies.
-
Advances in imaging technology are helping to improve the accuracy of PVNS diagnosis.
-
Clinical trials are exploring the use of targeted therapies to treat PVNS more effectively.
-
There is growing interest in the role of inflammation in the development and progression of PVNS.
-
New surgical techniques are being developed to minimize the risk of recurrence and improve patient outcomes.
-
Patient registries and databases are being established to collect data on PVNS and facilitate research.
Living with PVNS
Living with PVNS can be challenging, but there are ways to manage the condition and maintain a good quality of life. Here are some tips.
-
Maintaining a healthy weight can reduce stress on the affected joint and alleviate symptoms.
-
Regular exercise, tailored to your abilities, can help keep joints flexible and strong.
-
Using assistive devices, such as braces or canes, can provide support and improve mobility.
-
Joining a support group can provide emotional support and practical advice from others living with PVNS.
-
Staying informed about the latest research and treatment options can empower you to make informed decisions about your care.
-
Working closely with your healthcare team can help you develop a personalized treatment plan that meets your needs.
Interesting Facts about PVNS
Here are some additional intriguing facts about PVNS that you might find interesting.
-
PVNS was first described by Dr. Jaffe in 1941.
-
The name "Pigmented Villonodular Synovitis" refers to the pigmented (colored) and villonodular (finger-like) appearance of the affected synovium.
-
PVNS is considered a rare disease, with an estimated incidence of 1.8 cases per million people per year.
-
The condition is slightly more common in women than men.
-
PVNS can sometimes be mistaken for other joint conditions, such as rheumatoid arthritis or osteoarthritis.
-
The disease can affect both large and small joints, including the fingers and toes.
-
PVNS can occur in both monoarticular (one joint) and polyarticular (multiple joints) forms.
-
Some studies suggest a possible link between PVNS and certain genetic mutations.
-
PVNS can cause significant joint damage if left untreated, highlighting the importance of early diagnosis and intervention.
-
The disease can sometimes recur many years after the initial treatment, necessitating long-term follow-up.
-
PVNS can affect both the synovium of the joint and the tendon sheaths, leading to a condition known as tenosynovial giant cell tumor.
-
The term "giant cell tumor" refers to the presence of large, multinucleated cells in the affected tissue.
-
PVNS is often classified as a type of giant cell tumor due to its histological features.
-
The disease can sometimes be associated with other conditions, such as hemophilia or metabolic disorders.
-
PVNS can cause significant pain and disability, impacting a person's ability to perform daily activities.
-
Ongoing research and advancements in treatment are providing hope for better management and outcomes for PVNS patients.
Final Thoughts on Pigmented Villonodular Synovitis
Pigmented Villonodular Synovitis (PVNS) might sound like a mouthful, but understanding it can make a big difference. This rare joint condition, often affecting knees and hips, involves the abnormal growth of joint lining. Symptoms like swelling, pain, and stiffness can disrupt daily life. Early diagnosis and treatment are crucial to managing PVNS effectively. Treatments range from medication to surgery, depending on severity. Regular check-ups and being aware of symptoms can help catch PVNS early. Remember, knowledge is power. The more you know about PVNS, the better prepared you'll be to tackle it head-on. Stay informed, stay proactive, and don't hesitate to consult healthcare professionals if you suspect something's off with your joints.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
