Glomerulosclerosis might sound like a mouthful, but understanding it is crucial for kidney health. This condition involves scarring of the tiny filters in your kidneys, known as glomeruli. Why does this matter? Because these filters play a vital role in cleaning your blood. When they get damaged, it can lead to serious health issues, including kidney failure. What causes glomerulosclerosis? Factors like diabetes, high blood pressure, and certain infections can contribute. Can it be treated? While there's no cure, treatments can manage symptoms and slow progression. Want to know more? Let's dive into 50 facts about glomerulosclerosis to help you understand this condition better.
Key Takeaways:
- Glomerulosclerosis, a kidney condition, can be caused by diabetes and high blood pressure. Early detection and management are crucial to prevent serious complications like chronic kidney disease and cardiovascular issues.
- Lifestyle changes, such as managing diabetes and controlling blood pressure, can help prevent glomerulosclerosis. Regular check-ups, a kidney-friendly diet, and staying hydrated are essential for managing the condition effectively.
What is Glomerulosclerosis?
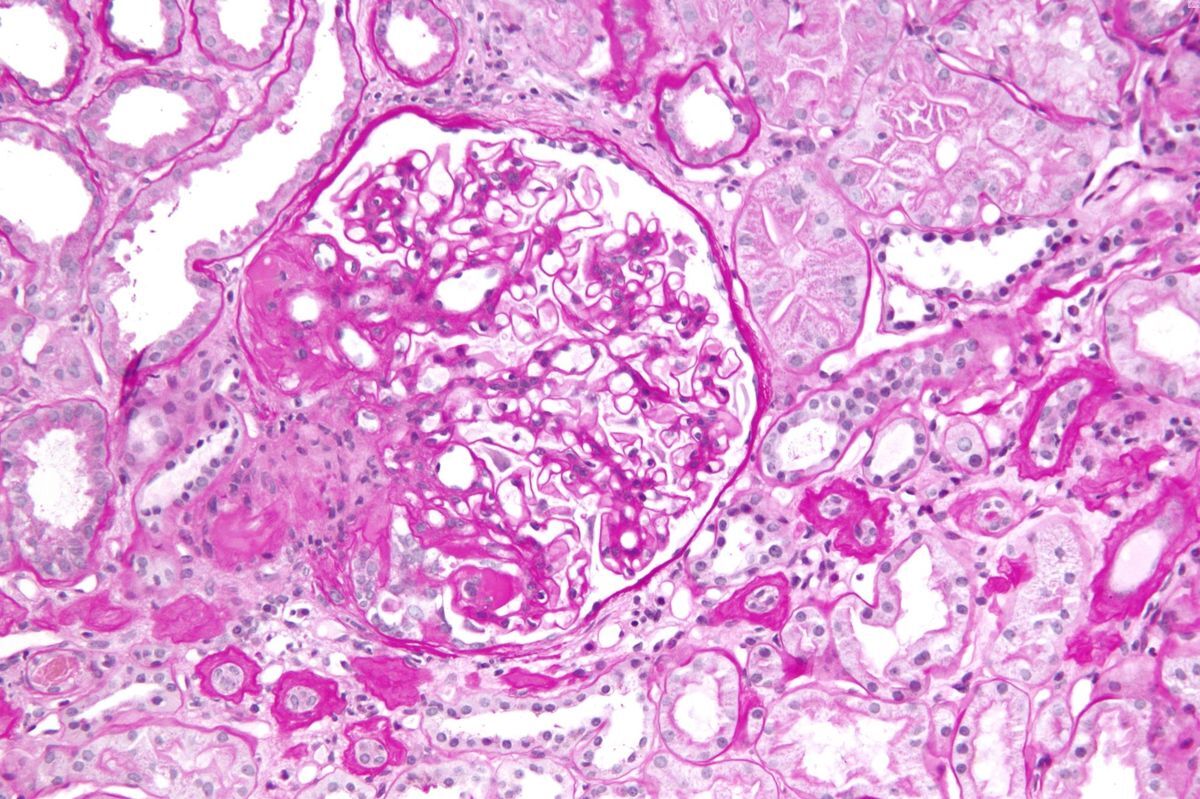
Glomerulosclerosis is a kidney condition where the tiny blood vessels in the kidneys, called glomeruli, become scarred. This scarring can affect kidney function, leading to serious health issues. Here are some key facts about this condition.
- Glomerulosclerosis can be caused by various diseases, including diabetes and high blood pressure.
- The condition can lead to chronic kidney disease (CKD) if not managed properly.
- Symptoms may include protein in the urine, swelling, and high blood pressure.
- Diagnosis often involves urine tests, blood tests, and kidney biopsies.
- Treatment focuses on controlling the underlying cause and managing symptoms.
Types of Glomerulosclerosis
There are different types of glomerulosclerosis, each with unique characteristics and causes. Understanding these types can help in managing the condition more effectively.
- Focal Segmental Glomerulosclerosis (FSGS) affects only some of the glomeruli and parts of each glomerulus.
- Diabetic Glomerulosclerosis is caused by long-term diabetes and is a leading cause of kidney failure.
- Hypertensive Glomerulosclerosis results from chronic high blood pressure damaging the kidneys.
- Idiopathic Glomerulosclerosis has no identifiable cause and is diagnosed when other causes are ruled out.
- Secondary Glomerulosclerosis occurs due to other diseases or conditions, such as lupus or HIV.
Risk Factors for Glomerulosclerosis
Certain factors can increase the risk of developing glomerulosclerosis. Awareness of these risk factors can aid in early detection and prevention.
- Diabetes is a significant risk factor due to its impact on blood vessels.
- High blood pressure can damage the kidneys over time, leading to glomerulosclerosis.
- Family history of kidney disease increases the likelihood of developing the condition.
- Obesity is linked to a higher risk of kidney problems, including glomerulosclerosis.
- Certain infections, like HIV, can lead to secondary glomerulosclerosis.
Symptoms and Signs
Recognizing the symptoms of glomerulosclerosis early can lead to better outcomes. Here are some common signs to watch for.
- Proteinuria, or protein in the urine, is a common symptom.
- Hematuria, or blood in the urine, may also occur.
- Edema, or swelling, particularly in the legs, ankles, and feet.
- High blood pressure is often a sign of kidney issues.
- Fatigue and weakness can result from decreased kidney function.
Diagnosis of Glomerulosclerosis
Accurate diagnosis is crucial for effective treatment. Various tests and procedures help in diagnosing glomerulosclerosis.
- Urine tests can detect protein and blood in the urine.
- Blood tests measure kidney function and check for underlying conditions.
- Kidney biopsy involves taking a small sample of kidney tissue for examination.
- Imaging tests, like ultrasounds, can provide a visual of the kidneys.
- Genetic testing may be used if a hereditary form of the disease is suspected.
Treatment Options
Treatment for glomerulosclerosis aims to manage symptoms and address the underlying cause. Here are some common approaches.
- Medications like ACE inhibitors and ARBs help control blood pressure.
- Diuretics can reduce swelling by helping the body remove excess fluid.
- Immunosuppressive drugs may be used in cases of immune-related glomerulosclerosis.
- Lifestyle changes, such as a low-sodium diet, can help manage symptoms.
- Dialysis or kidney transplant may be necessary in advanced cases.
Complications of Glomerulosclerosis
If left untreated, glomerulosclerosis can lead to severe complications. Understanding these risks can highlight the importance of early intervention.
- Chronic kidney disease (CKD) is a common complication.
- End-stage renal disease (ESRD) may occur, requiring dialysis or a transplant.
- Cardiovascular disease risk increases due to high blood pressure and other factors.
- Anemia can result from decreased kidney function affecting red blood cell production.
- Bone disease may develop due to imbalances in calcium and phosphorus.
Preventing Glomerulosclerosis
While not all cases can be prevented, certain measures can reduce the risk of developing glomerulosclerosis.
- Managing diabetes effectively can prevent diabetic glomerulosclerosis.
- Controlling blood pressure is crucial in reducing kidney damage.
- Maintaining a healthy weight can lower the risk of kidney disease.
- Regular exercise helps improve overall health and kidney function.
- Avoiding smoking reduces the risk of kidney and cardiovascular diseases.
Living with Glomerulosclerosis
Living with glomerulosclerosis requires ongoing management and lifestyle adjustments. Here are some tips for managing the condition.
- Regular check-ups with a healthcare provider are essential.
- Following a kidney-friendly diet can help manage symptoms.
- Staying hydrated is important, but fluid intake may need to be monitored.
- Monitoring blood pressure at home can help manage the condition.
- Joining a support group can provide emotional support and practical advice.
Research and Future Directions
Ongoing research aims to improve the understanding and treatment of glomerulosclerosis. Here are some areas of focus.
- New medications are being developed to target the underlying causes of glomerulosclerosis.
- Advances in genetic research may lead to better diagnosis and treatment options.
- Stem cell therapy is being explored as a potential treatment for kidney damage.
- Improved imaging techniques can help in early detection and monitoring of the disease.
- Patient education and awareness programs aim to improve outcomes for those with glomerulosclerosis.
Final Thoughts on Glomerulosclerosis
Glomerulosclerosis, a condition affecting the kidneys, involves scarring of the glomeruli, which are tiny filters in the kidneys. This scarring can lead to kidney dysfunction and, in severe cases, kidney failure. Understanding the causes, symptoms, and treatment options is crucial for managing this condition effectively. Early detection and intervention can slow the progression, improving the quality of life for those affected. Treatments range from medications to lifestyle changes and, in some cases, dialysis or kidney transplants. Staying informed and working closely with healthcare providers can make a significant difference. Remember, knowledge is power when it comes to managing health conditions. Stay proactive, seek regular medical advice, and don't hesitate to ask questions. Your health is worth it.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
