Pelizaeus–Merzbacher Disease (PMD) is a rare genetic disorder affecting the central nervous system. Caused by mutations in the PLP1 gene, this disease disrupts the formation of myelin, the protective covering of nerve fibers. Symptoms often appear in infancy or early childhood and can include developmental delays, muscle stiffness, and difficulty with coordination. PMD primarily affects males due to its X-linked recessive inheritance pattern. There is currently no cure, but treatments focus on managing symptoms and improving quality of life. Understanding PMD is crucial for early diagnosis and intervention, which can significantly impact the progression and management of the disease.
Key Takeaways:
- Pelizaeus–Merzbacher Disease (PMD) is a rare genetic disorder affecting the brain's white matter, leading to symptoms like delayed motor development and cognitive impairment in children, with ongoing research offering hope for future breakthroughs.
- Families affected by PMD can find support through resources like support groups, educational materials, and advocacy organizations, while genetic counseling provides essential information for family planning and risk assessment.
What is Pelizaeus–Merzbacher Disease?
Pelizaeus–Merzbacher Disease (PMD) is a rare genetic disorder that affects the central nervous system. It primarily impacts the brain's white matter, leading to various neurological symptoms.
- PMD is caused by mutations in the PLP1 gene.
- This disease is part of a group known as leukodystrophies.
- It mainly affects males due to its X-linked recessive inheritance pattern.
- Symptoms often appear in infancy or early childhood.
- PMD can lead to delayed motor development and coordination issues.
Symptoms of Pelizaeus–Merzbacher Disease
Understanding the symptoms can help in early diagnosis and management of PMD. These symptoms vary in severity and can affect different aspects of a child's development.
- Nystagmus, or involuntary eye movement, is a common early sign.
- Children may experience hypotonia, or reduced muscle tone.
- Spasticity can develop, causing stiff and rigid muscles.
- Ataxia, or lack of muscle coordination, is often present.
- Cognitive impairment can range from mild to severe.
Diagnosis of Pelizaeus–Merzbacher Disease
Accurate diagnosis is crucial for managing PMD. Various tests and evaluations are used to confirm the presence of this genetic disorder.
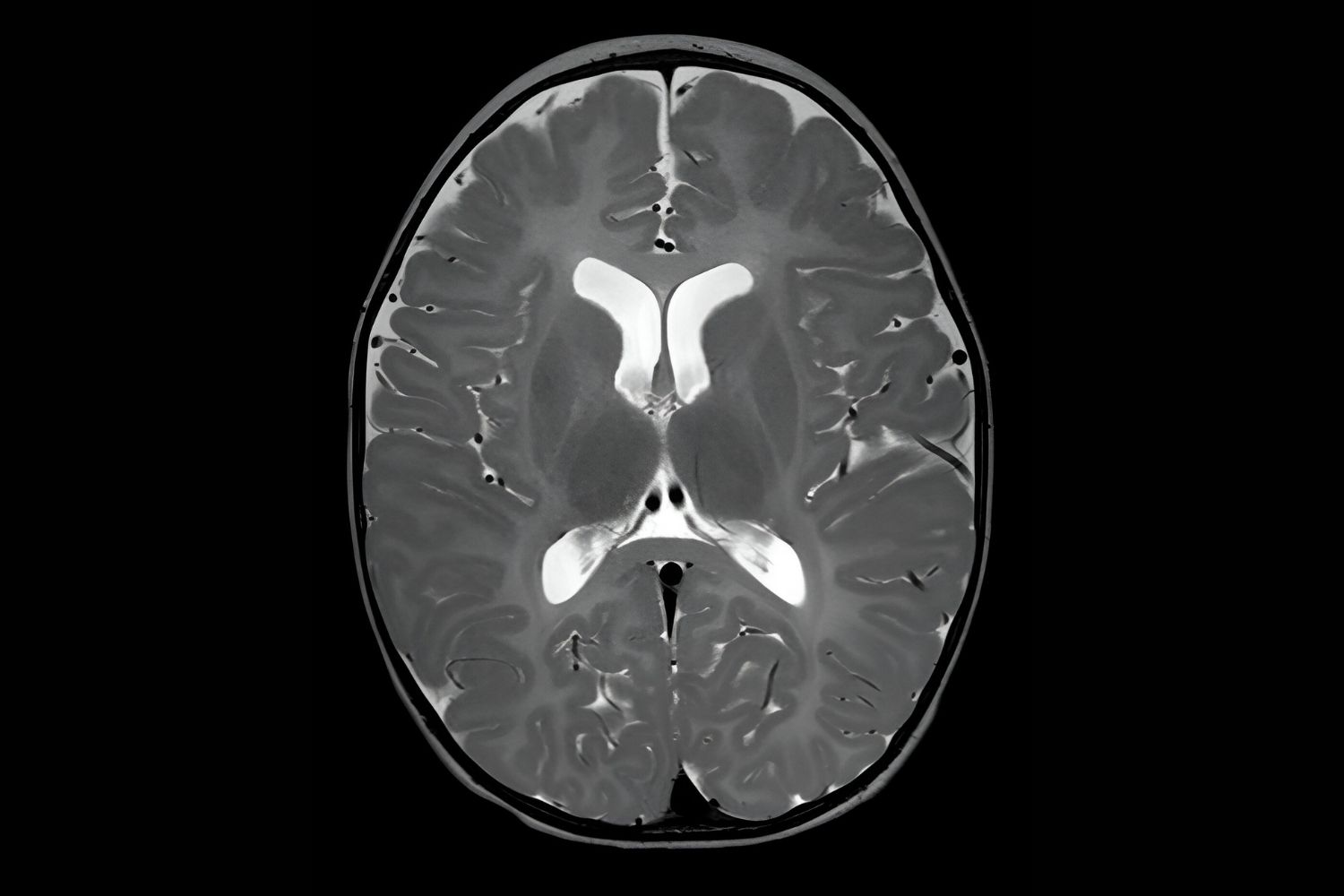
- MRI scans can reveal abnormalities in brain white matter.
- Genetic testing identifies mutations in the PLP1 gene.
- Clinical evaluations assess physical and neurological symptoms.
- Family history can provide clues, as PMD is inherited.
- Electroencephalograms (EEGs) may be used to monitor brain activity.
Treatment and Management
While there is no cure for PMD, various treatments can help manage symptoms and improve quality of life.
- Physical therapy aids in maintaining mobility and muscle strength.
- Occupational therapy helps with daily activities and fine motor skills.
- Speech therapy can address communication difficulties.
- Medications may be prescribed to manage spasticity and seizures.
- Supportive care includes nutritional support and respiratory assistance.
Research and Future Directions
Ongoing research aims to better understand PMD and develop new treatments. Advances in genetics and neurology offer hope for future breakthroughs.
- Stem cell research is being explored as a potential treatment.
- Gene therapy holds promise for correcting genetic mutations.
- Clinical trials are testing new medications and therapies.
- Animal models help researchers study the disease's progression.
- Patient registries collect data to improve understanding and care.
Living with Pelizaeus–Merzbacher Disease
Families and individuals affected by PMD face unique challenges. Support networks and resources can make a significant difference.
- Support groups provide emotional and practical assistance.
- Educational resources help families understand the disease.
- Advocacy organizations work to raise awareness and funding.
- Assistive devices can improve mobility and independence.
- Respite care offers temporary relief for caregivers.
Genetic Counseling and Family Planning
Genetic counseling is essential for families affected by PMD. It provides information on inheritance patterns and risks for future children.
- Carrier testing can identify potential carriers of the PLP1 mutation.
- Prenatal testing is available for at-risk pregnancies.
- Preimplantation genetic diagnosis (PGD) can be used with IVF to select embryos without the mutation.
- Genetic counselors offer guidance on family planning options.
- Educational sessions help families understand genetic risks.
Historical Background of Pelizaeus–Merzbacher Disease
PMD has a rich history of discovery and research. Understanding its origins can provide context for current knowledge and treatment approaches.
- Friedrich Pelizaeus first described the disease in 1885.
- Ludwig Merzbacher further characterized it in 1910.
- The PLP1 gene was identified as the cause in the 1980s.
- Early research focused on clinical observations and family studies.
- Advances in molecular genetics have revolutionized understanding of PMD.
Impact on Quality of Life
PMD significantly affects the quality of life for those diagnosed and their families. Addressing these impacts is a key part of comprehensive care.
- Mobility issues can limit independence and daily activities.
- Communication difficulties may affect social interactions.
- Chronic health problems require ongoing medical care.
- Emotional and psychological support is crucial for families.
- Access to specialized care can improve outcomes and quality of life.
The Final Word on Pelizaeus–Merzbacher Disease
Pelizaeus–Merzbacher Disease (PMD) is a rare, inherited disorder affecting the central nervous system. It primarily impacts the myelin sheath, which insulates nerve fibers, leading to severe neurological symptoms. PMD manifests in early childhood with symptoms like involuntary eye movements, muscle stiffness, and developmental delays. While there's no cure, treatments focus on managing symptoms and improving quality of life. Genetic counseling is crucial for families affected by PMD, as it helps understand the inheritance pattern and risks for future children. Research continues to explore potential therapies, offering hope for better management in the future. Awareness and support for those living with PMD can make a significant difference. Understanding this disease helps in advocating for more research and resources, ultimately aiming for a brighter future for those affected.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
