Pelizaeus-Merzbacher Disease (PMD) is a rare genetic disorder affecting the central nervous system. Caused by mutations in the PLP1 gene, it primarily impacts the production of myelin, the protective covering of nerve fibers. This disease manifests in early childhood, leading to symptoms like involuntary eye movements, muscle stiffness, and delayed development. PMD is part of a group of disorders known as leukodystrophies, which involve the white matter of the brain. Understanding this condition can be challenging due to its rarity and complexity. However, knowing the facts about Pelizaeus-Merzbacher Disease can help in recognizing symptoms, seeking appropriate care, and supporting affected individuals and their families.
Key Takeaways:
- Pelizaeus-Merzbacher Disease is a rare genetic disorder affecting the brain's white matter, causing symptoms like muscle stiffness and developmental delays. Research and support are crucial for improving outcomes.
- Myelin, a fatty substance that insulates nerve fibers, plays a crucial role in PMD. Understanding its role and promoting myelin repair hold promise for improving outcomes in individuals with PMD.
What is Pelizaeus-Merzbacher Disease?
Pelizaeus-Merzbacher Disease (PMD) is a rare genetic disorder affecting the central nervous system. It primarily impacts the brain's white matter, leading to various neurological symptoms. Here are some intriguing facts about this condition.
-
PMD is a type of leukodystrophy, a group of disorders characterized by the abnormal development or destruction of the white matter in the brain.
-
The disease is named after Friedrich Pelizaeus and Ludwig Merzbacher, who first described it in the late 19th and early 20th centuries.
-
PMD is caused by mutations in the PLP1 gene, which provides instructions for making a protein essential for the formation of myelin, the protective covering of nerve fibers.
-
The condition is inherited in an X-linked recessive pattern, meaning it primarily affects males, while females can be carriers.
-
Symptoms of PMD usually appear in infancy or early childhood and can include developmental delays, muscle stiffness, and involuntary eye movements.
Symptoms and Diagnosis
Understanding the symptoms and how PMD is diagnosed can help in managing the condition more effectively.
-
Early signs of PMD include hypotonia (reduced muscle tone), nystagmus (rapid, involuntary eye movements), and delayed motor skills.
-
As the disease progresses, affected individuals may develop spasticity (muscle stiffness), ataxia (lack of muscle coordination), and cognitive impairments.
-
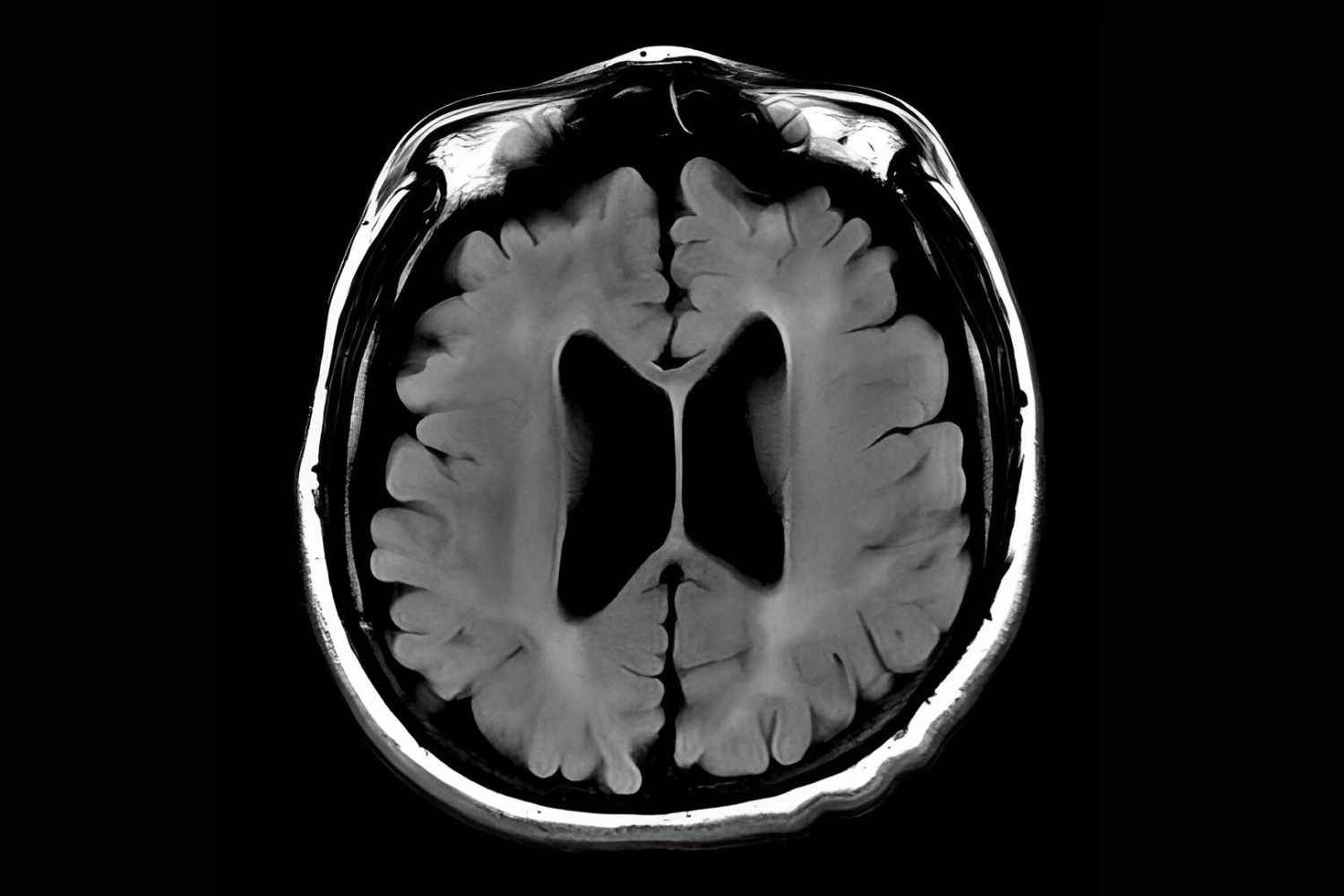
Diagnosis often involves a combination of clinical evaluation, magnetic resonance imaging (MRI) to detect abnormalities in the brain's white matter, and genetic testing to identify mutations in the PLP1 gene.
-
MRI scans of individuals with PMD typically show a lack of myelin in the brain, which appears as white patches.
-
Genetic testing can confirm the diagnosis by identifying mutations in the PLP1 gene, helping to distinguish PMD from other leukodystrophies.
Types of Pelizaeus-Merzbacher Disease
PMD can be classified into different types based on the severity and progression of symptoms.
-
Classic PMD is the most common form, characterized by early onset and a gradual progression of symptoms.
-
Connatal PMD is a more severe form that presents at birth or shortly after, with rapid progression and significant neurological impairment.
-
Transitional PMD falls between classic and connatal forms, with symptoms appearing in early childhood and progressing at a moderate rate.
-
Adult-onset PMD is rare, with symptoms appearing later in life and progressing more slowly than other forms.
-
The severity of PMD can vary widely even among individuals with the same type, influenced by the specific mutation in the PLP1 gene.
Treatment and Management
While there is no cure for PMD, various treatments and management strategies can help improve the quality of life for those affected.
-
Physical therapy can help maintain muscle strength and flexibility, improving mobility and reducing spasticity.
-
Occupational therapy can assist individuals in developing skills for daily living and enhancing their independence.
-
Speech therapy may be beneficial for those with speech and swallowing difficulties.
-
Medications such as muscle relaxants and anticonvulsants can help manage symptoms like spasticity and seizures.
-
Regular follow-up with a multidisciplinary team of healthcare professionals is essential for monitoring the progression of the disease and adjusting treatment plans as needed.
Research and Future Directions
Ongoing research aims to better understand PMD and develop new treatments.
-
Scientists are exploring gene therapy as a potential treatment for PMD, aiming to correct the underlying genetic mutation.
-
Stem cell therapy is another area of research, with the goal of replacing damaged myelin-producing cells in the brain.
-
Advances in imaging techniques are helping researchers study the progression of PMD and evaluate the effectiveness of new treatments.
-
Clinical trials are underway to test the safety and efficacy of various experimental therapies for PMD.
-
Increased awareness and funding for PMD research can accelerate the development of new treatments and improve outcomes for those affected.
Living with Pelizaeus-Merzbacher Disease
Living with PMD presents unique challenges, but support and resources are available to help individuals and their families.
-
Support groups and online communities can provide valuable information and emotional support for families affected by PMD.
-
Educational resources and advocacy organizations can help raise awareness about PMD and promote research funding.
-
Assistive devices such as wheelchairs, communication aids, and adaptive equipment can enhance mobility and independence.
-
Early intervention programs can provide specialized services to support the development of children with PMD.
-
Palliative care and hospice services can offer comfort and support for individuals with advanced PMD and their families.
Genetic Counseling and Family Planning
Genetic counseling can provide important information for families affected by PMD.
-
Genetic counselors can help families understand the inheritance pattern of PMD and the risks of passing the condition to future children.
-
Carrier testing can identify female carriers of the PLP1 mutation, providing information for family planning decisions.
-
Prenatal testing and preimplantation genetic diagnosis (PGD) are options for families who wish to avoid passing PMD to their children.
-
Genetic counseling can also provide emotional support and resources for families coping with a PMD diagnosis.
-
Families can benefit from connecting with other families affected by PMD to share experiences and support each other.
The Role of Myelin in PMD
Myelin plays a crucial role in the development and progression of PMD.
-
Myelin is a fatty substance that surrounds and insulates nerve fibers, allowing for the rapid transmission of electrical signals in the brain.
-
In PMD, mutations in the PLP1 gene disrupt the production of myelin, leading to the degeneration of white matter in the brain.
-
The loss of myelin results in the neurological symptoms seen in PMD, such as motor and cognitive impairments.
-
Research into myelin biology is helping scientists understand the mechanisms underlying PMD and develop potential treatments.
-
Therapies aimed at promoting myelin repair and regeneration hold promise for improving outcomes in individuals with PMD.
Support and Advocacy
Support and advocacy efforts are crucial for improving the lives of those affected by PMD.
-
Organizations such as the Pelizaeus-Merzbacher Disease Foundation provide resources, support, and advocacy for individuals and families affected by PMD.
-
Fundraising events and awareness campaigns can help raise money for PMD research and support services.
-
Advocacy efforts can promote policies that improve access to healthcare and support services for individuals with PMD.
-
Collaboration between researchers, healthcare providers, and advocacy organizations can accelerate the development of new treatments and improve outcomes for those affected by PMD.
-
Increased awareness and understanding of PMD can help reduce stigma and improve the quality of life for individuals and families affected by the condition.
Final Thoughts on Pelizaeus-Merzbacher Disease
Pelizaeus-Merzbacher Disease (PMD) is a rare genetic disorder that affects the central nervous system. Understanding PMD is crucial for those affected and their families. This disease, caused by mutations in the PLP1 gene, leads to a range of symptoms, including motor skill difficulties, muscle stiffness, and developmental delays. Early diagnosis and intervention can significantly improve quality of life. While there's no cure yet, ongoing research offers hope for future treatments. Raising awareness about PMD helps drive support for research and resources for affected individuals. By sharing knowledge and supporting each other, we can make a difference in the lives of those living with PMD. Stay informed, stay supportive, and let's continue to push for advancements in understanding and treating this challenging condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
