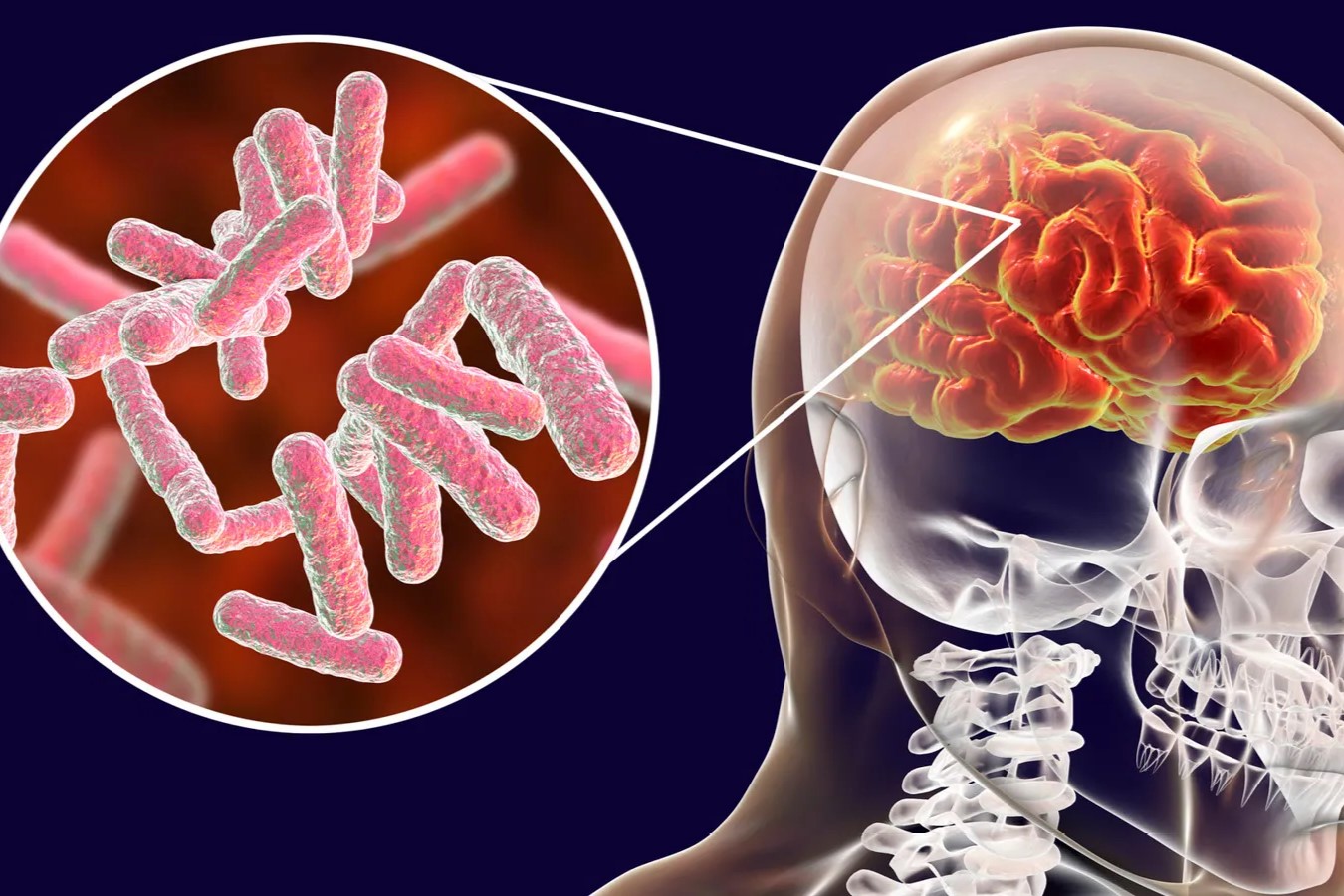
Tuberculous meningitis is a severe infection caused by Mycobacterium tuberculosis, the same bacteria responsible for tuberculosis. This condition affects the protective membranes covering the brain and spinal cord, leading to inflammation and potentially life-threatening complications. Early symptoms often mimic those of other illnesses, making diagnosis tricky. Common signs include persistent headaches, fever, neck stiffness, and confusion. Without prompt treatment, it can result in severe neurological damage or death. Risk factors include a weakened immune system, HIV infection, and living in areas with high tuberculosis prevalence. Treatment typically involves a lengthy course of antibiotics and supportive care. Understanding the facts about tuberculous meningitis can help in recognizing symptoms early and seeking timely medical intervention.
Key Takeaways:
- Tuberculous Meningitis is a severe form of tuberculosis that affects the brain and spinal cord, causing symptoms like severe headache, fever, and neck stiffness. Early diagnosis and treatment are crucial for better outcomes.
- Preventing Tuberculous Meningitis involves strategies like vaccination, prompt treatment of active tuberculosis, and improving living conditions to reduce the spread of the disease. Public health education and awareness campaigns play a vital role in controlling tuberculosis.
What is Tuberculous Meningitis?
Tuberculous meningitis (TBM) is a severe form of tuberculosis that affects the membranes covering the brain and spinal cord. It is a life-threatening condition requiring prompt diagnosis and treatment. Here are some crucial facts about TBM:
- TBM is caused by Mycobacterium tuberculosis, the same bacteria responsible for pulmonary tuberculosis.
- It primarily affects the meninges, the protective membranes surrounding the brain and spinal cord.
- TBM is more common in developing countries with high rates of tuberculosis.
- It can occur at any age but is more prevalent in children and immunocompromised individuals.
- Symptoms often include severe headache, fever, neck stiffness, and altered mental status.
How is Tuberculous Meningitis Diagnosed?
Diagnosing TBM can be challenging due to its non-specific symptoms. Various tests and procedures help in confirming the diagnosis:
- A lumbar puncture (spinal tap) is often performed to collect cerebrospinal fluid (CSF) for analysis.
- CSF analysis typically shows elevated protein levels, low glucose levels, and increased white blood cells.
- Acid-fast bacilli (AFB) staining and culture of CSF can identify Mycobacterium tuberculosis.
- Polymerase chain reaction (PCR) tests can detect bacterial DNA in CSF, providing a quicker diagnosis.
- Imaging studies like MRI and CT scans can reveal abnormalities in the brain and spinal cord.
Treatment Options for Tuberculous Meningitis
Effective treatment of TBM requires a combination of antibiotics and supportive care. Here are some key points about TBM treatment:
- The standard treatment regimen includes a combination of four antibiotics: isoniazid, rifampicin, pyrazinamide, and ethambutol.
- Treatment duration is typically 9-12 months, longer than for pulmonary tuberculosis.
- Corticosteroids like dexamethasone are often prescribed to reduce inflammation and prevent complications.
- Early initiation of treatment is crucial for better outcomes and reducing the risk of long-term neurological damage.
- Regular monitoring and follow-up are essential to assess treatment response and manage side effects.
Complications Associated with Tuberculous Meningitis
TBM can lead to various complications, some of which can be life-threatening or cause permanent damage:
- Hydrocephalus, an accumulation of fluid in the brain, is a common complication requiring surgical intervention.
- Stroke can occur due to inflammation and blockage of blood vessels in the brain.
- Seizures are frequent in TBM patients and may require long-term anticonvulsant therapy.
- Cranial nerve palsies can result in vision and hearing problems.
- Long-term neurological deficits, including cognitive impairment and motor dysfunction, are possible.
Risk Factors for Developing Tuberculous Meningitis
Certain factors increase the risk of developing TBM. Understanding these can help in early detection and prevention:
- HIV infection significantly raises the risk due to weakened immune systems.
- Malnutrition and poor living conditions contribute to higher susceptibility.
- Close contact with individuals having active tuberculosis increases the likelihood of infection.
- Young children and the elderly are more vulnerable due to weaker immune defenses.
- Pre-existing medical conditions like diabetes and chronic kidney disease can also elevate the risk.
Preventing Tuberculous Meningitis
Prevention strategies focus on reducing the spread of tuberculosis and protecting high-risk individuals:
- Bacillus Calmette-Guérin (BCG) vaccination provides some protection against severe forms of tuberculosis, including TBM.
- Prompt diagnosis and treatment of active tuberculosis cases help prevent transmission.
- Regular screening and prophylactic treatment for high-risk groups can reduce the incidence of TBM.
- Improving living conditions and nutrition can strengthen immune systems and lower susceptibility.
- Public health education and awareness campaigns are vital in controlling the spread of tuberculosis.
Global Impact of Tuberculous Meningitis
TBM remains a significant public health challenge worldwide, particularly in regions with high tuberculosis prevalence:
- Approximately 1-2% of all tuberculosis cases progress to TBM.
- TBM accounts for a substantial proportion of tuberculosis-related deaths, especially in children.
- The World Health Organization (WHO) emphasizes the need for early diagnosis and treatment to reduce TBM mortality.
- Multidrug-resistant tuberculosis (MDR-TB) complicates TBM treatment and requires specialized care.
- International collaboration and funding are essential to combat TBM and improve outcomes.
Research and Future Directions
Ongoing research aims to improve TBM diagnosis, treatment, and prevention. Here are some recent advancements and future directions:
- New diagnostic tools, including advanced molecular techniques, are being developed for quicker and more accurate TBM detection.
- Research on shorter and more effective treatment regimens is underway to improve patient compliance and outcomes.
- Studies are exploring the role of adjunctive therapies, such as immunomodulators, in enhancing TBM treatment.
- Vaccine development efforts focus on creating more effective vaccines against tuberculosis, including TBM.
- Global health initiatives and partnerships continue to prioritize TBM research and resource allocation to combat this deadly disease.
Final Thoughts on Tuberculous Meningitis
Tuberculous meningitis is a serious condition that requires prompt medical attention. Understanding its symptoms, causes, and treatments can make a significant difference in outcomes. Early diagnosis and treatment are crucial to prevent severe complications. Remember, this disease primarily affects the brain and spinal cord, leading to potentially life-threatening situations if not addressed quickly.
Awareness and education about tuberculous meningitis can help in early detection and treatment. If you or someone you know exhibits symptoms like persistent headaches, fever, or neck stiffness, seek medical advice immediately. Knowledge is power, and staying informed about such conditions can save lives.
Stay vigilant, prioritize health, and spread awareness about tuberculous meningitis. Your proactive approach can make a difference in combating this serious illness.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
