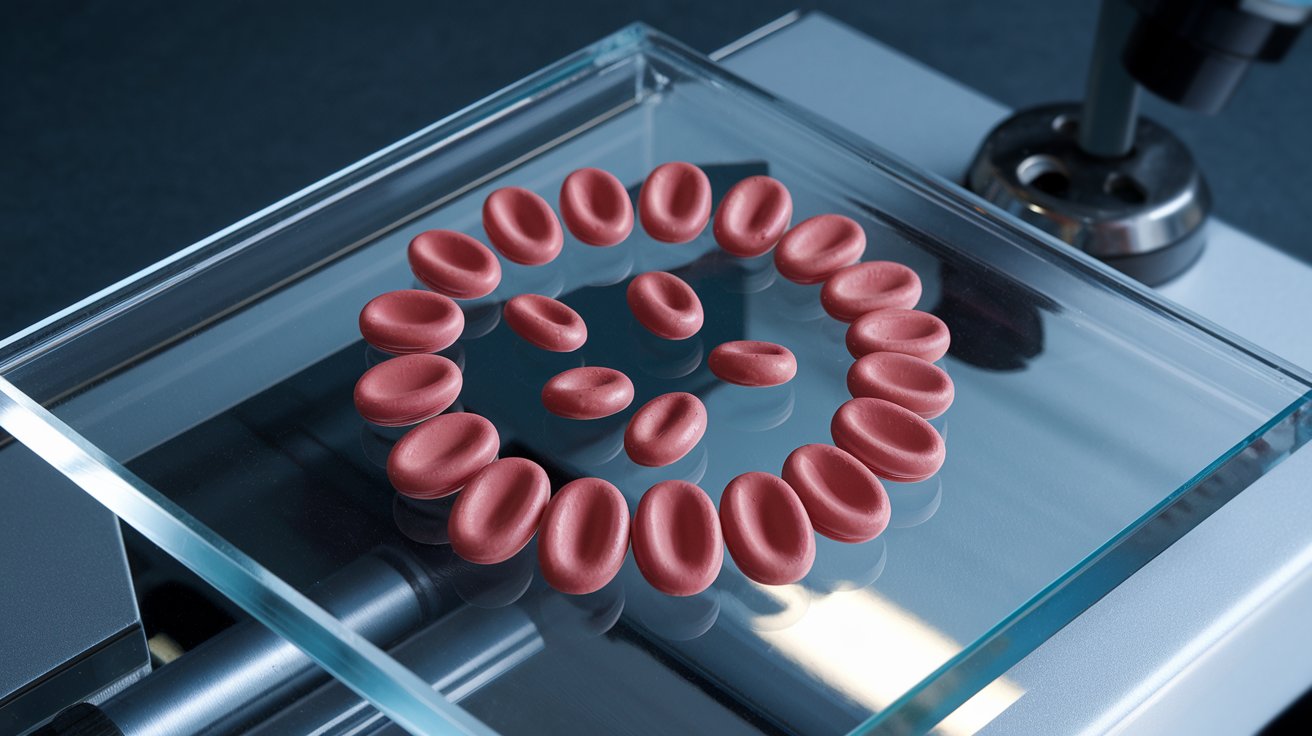
What is HLA antigen? Human Leukocyte Antigen (HLA) is a protein found on the surface of most cells in your body. Why is it important? It plays a crucial role in the immune system by helping the body distinguish between its own cells and foreign invaders like bacteria or viruses. How does it work? HLA molecules present pieces of proteins (antigens) to immune cells, which then decide if these pieces are harmful. Why should you care? Understanding HLA is vital for organ transplants, as matching HLA types between donors and recipients can prevent rejection. In essence, HLA antigens are like the body's ID cards, ensuring the immune system functions correctly.
Key Takeaways:
- HLA antigens help the immune system recognize friend from foe. They play a crucial role in organ transplants and disease associations, making them essential for personalized medicine and pregnancy outcomes.
- HLA typing informs personalized treatments and can predict adverse reactions to certain drugs. It also influences pregnancy outcomes, making it a key player in personalized medicine and reproductive health.
What is HLA Antigen?
Human Leukocyte Antigen (HLA) is a protein found on the surface of white blood cells. These proteins play a crucial role in the immune system by helping the body distinguish between its own cells and foreign invaders.
-
HLA stands for Human Leukocyte Antigen. This name reflects its primary location on white blood cells (leukocytes).
-
HLA proteins are encoded by genes located on chromosome 6. This specific region is known as the Major Histocompatibility Complex (MHC).
-
There are three main classes of HLA: Class I, Class II, and Class III. Each class has different functions and locations within the body.
-
HLA Class I molecules are found on almost all nucleated cells. They present peptides from inside the cell to the immune system.
-
HLA Class II molecules are primarily on antigen-presenting cells. These include macrophages, dendritic cells, and B cells.
Importance of HLA in Transplantation
HLA matching is critical in organ and bone marrow transplants. A close match between donor and recipient HLA types can reduce the risk of transplant rejection.
-
HLA typing is used to match organ donors with recipients. This process helps ensure compatibility and reduces the likelihood of rejection.
-
A perfect HLA match is rare. Even siblings have only a 25% chance of being a perfect match.
-
HLA mismatches can lead to graft-versus-host disease (GVHD). This condition occurs when the donor's immune cells attack the recipient's body.
-
HLA antibodies can develop after a transplant. These antibodies can attack the transplanted organ, leading to rejection.
-
Cross-matching tests are performed before transplantation. These tests check for pre-existing antibodies against the donor's HLA.
HLA and Disease Association
Certain HLA types are associated with an increased risk of specific diseases. Understanding these associations can help in disease prediction and management.
-
HLA-B27 is linked to ankylosing spondylitis. This autoimmune disease affects the spine and large joints.
-
HLA-DR4 is associated with rheumatoid arthritis. This condition causes inflammation in the joints.
-
HLA-DQ2 and HLA-DQ8 are linked to celiac disease. People with these HLA types are more likely to develop this gluten intolerance.
-
HLA-A3 is associated with hemochromatosis. This genetic disorder causes the body to absorb too much iron.
-
HLA-DR3 is linked to type 1 diabetes. This autoimmune disease destroys insulin-producing cells in the pancreas.
HLA and Immune Response
HLA molecules are essential for the immune system's ability to recognize and respond to pathogens. They present peptide fragments to T cells, triggering an immune response.
-
HLA Class I molecules present endogenous antigens. These are peptides from within the cell, such as viral proteins.
-
HLA Class II molecules present exogenous antigens. These are peptides from outside the cell, such as bacterial proteins.
-
T cells recognize antigens presented by HLA molecules. This recognition is crucial for initiating an immune response.
-
CD8+ T cells interact with HLA Class I molecules. These T cells are involved in killing infected or cancerous cells.
-
CD4+ T cells interact with HLA Class II molecules. These T cells help coordinate the immune response by activating other immune cells.
HLA Diversity and Evolution
HLA genes are highly polymorphic, meaning there is a lot of variation in the population. This diversity is beneficial for the survival of the species.
-
There are thousands of different HLA alleles. This genetic diversity helps the immune system recognize a wide range of pathogens.
-
HLA diversity is greater in populations with a long history of exposure to various pathogens. This suggests that pathogen pressure drives HLA diversity.
-
HLA alleles can be inherited in a co-dominant manner. This means both maternal and paternal alleles are expressed.
-
Certain HLA types are more common in specific ethnic groups. This reflects the evolutionary history and migration patterns of human populations.
-
HLA diversity can affect vaccine efficacy. Different HLA types may present vaccine antigens differently, influencing the immune response.
HLA Typing Methods
HLA typing is a laboratory procedure used to identify the specific HLA alleles a person has. This information is crucial for transplantation and disease association studies.
-
Serological typing was the first method used for HLA typing. This method uses antibodies to detect HLA antigens on the cell surface.
-
Molecular typing methods are now more common. These methods include PCR and sequencing techniques.
-
Next-generation sequencing (NGS) provides high-resolution HLA typing. NGS can identify even minor differences between HLA alleles.
-
HLA typing can be performed on various sample types. These include blood, saliva, and buccal swabs.
-
High-resolution HLA typing is essential for bone marrow transplantation. It ensures the best possible match between donor and recipient.
HLA and Personalized Medicine
HLA typing can inform personalized medical treatments, including drug therapy and disease management.
-
HLA-B*57:01 is associated with hypersensitivity to abacavir. This antiretroviral drug can cause severe allergic reactions in people with this HLA type.
-
HLA typing can predict response to certain cancer immunotherapies. Some HLA types are better at presenting tumor antigens to the immune system.
-
Pharmacogenomics uses HLA typing to guide drug therapy. This approach aims to reduce adverse drug reactions and improve treatment efficacy.
-
HLA typing can help identify individuals at risk for autoimmune diseases. Early identification can lead to preventive measures and early treatment.
-
Personalized vaccines may be developed based on HLA typing. These vaccines could be more effective by targeting specific HLA types.
HLA and Pregnancy
HLA compatibility between mother and fetus can influence pregnancy outcomes. Certain HLA mismatches can lead to complications.
-
HLA-G plays a role in maternal-fetal tolerance. This molecule helps prevent the mother's immune system from attacking the fetus.
-
HLA mismatches can lead to recurrent miscarriages. Some studies suggest that certain HLA combinations between partners increase miscarriage risk.
-
HLA-C is involved in placental development. Proper HLA-C expression is crucial for a healthy pregnancy.
-
HLA typing can be used in reproductive medicine. It helps identify potential issues related to HLA compatibility.
-
Certain HLA types are associated with preeclampsia. This pregnancy complication involves high blood pressure and can be life-threatening for both mother and baby.
Final Thoughts on HLA Antigens
HLA antigens play a crucial role in the immune system, helping the body distinguish between its own cells and foreign invaders. Understanding these proteins can aid in organ transplants, disease research, and personalized medicine. They’re like the body's ID cards, ensuring that immune responses are accurate and effective.
Knowing your HLA type can be vital for matching organ donors and recipients, reducing the risk of transplant rejection. It also helps in diagnosing autoimmune diseases and tailoring treatments to individual genetic profiles.
Research continues to uncover more about how these antigens influence health and disease. Staying informed about HLA antigens can empower you to make better health decisions and understand your body's unique characteristics.
So, next time you hear about HLA antigens, remember their importance in keeping your immune system in check and advancing medical science.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
