Multiple acyl-CoA deficiency is a rare metabolic disorder that affects the body's ability to break down fats and proteins for energy. This condition is caused by mutations in genes responsible for producing enzymes needed in the fatty acid oxidation process. Symptoms can range from mild to severe and may include muscle weakness, low blood sugar, and developmental delays. Early diagnosis and treatment are crucial for managing the condition and improving quality of life. In this post, we'll explore 30 intriguing facts about multiple acyl-CoA deficiency, shedding light on its causes, symptoms, and management strategies. Get ready to dive into the world of metabolic disorders!
Key Takeaways:
- Multiple Acyl-CoA Deficiency is a rare genetic disorder affecting fat and protein breakdown, leading to muscle weakness and metabolic crises. Early diagnosis and dietary management are crucial for symptom control and prevention of complications.
- Ongoing research for Multiple Acyl-CoA Deficiency explores gene therapy, enzyme replacement, and antioxidants to improve patient care. Collaboration between researchers, clinicians, and patient communities is essential for advancing knowledge and treatment options.
What is Multiple Acyl-CoA Deficiency?
Multiple acyl-CoA deficiency, also known as glutaric acidemia type II, is a rare metabolic disorder. It affects the body's ability to break down fats and proteins for energy. This condition can lead to a variety of health issues.
- Multiple acyl-CoA deficiency is a genetic disorder caused by mutations in the ETFA, ETFB, or ETFDH genes.
- These genes are responsible for producing enzymes that help break down fats and proteins.
- Symptoms can appear in infancy, childhood, or adulthood, making diagnosis challenging.
- Common symptoms include muscle weakness, low blood sugar, and a distinctive body odor.
- Some individuals may experience severe metabolic crises, which can be life-threatening.
How is Multiple Acyl-CoA Deficiency Diagnosed?
Diagnosing this condition involves a combination of clinical evaluation, laboratory tests, and genetic testing. Early diagnosis is crucial for managing symptoms and preventing complications.
- Blood and urine tests can detect abnormal levels of organic acids and acylcarnitines.
- Genetic testing can confirm mutations in the ETFA, ETFB, or ETFDH genes.
- Newborn screening programs in some countries can identify the disorder early.
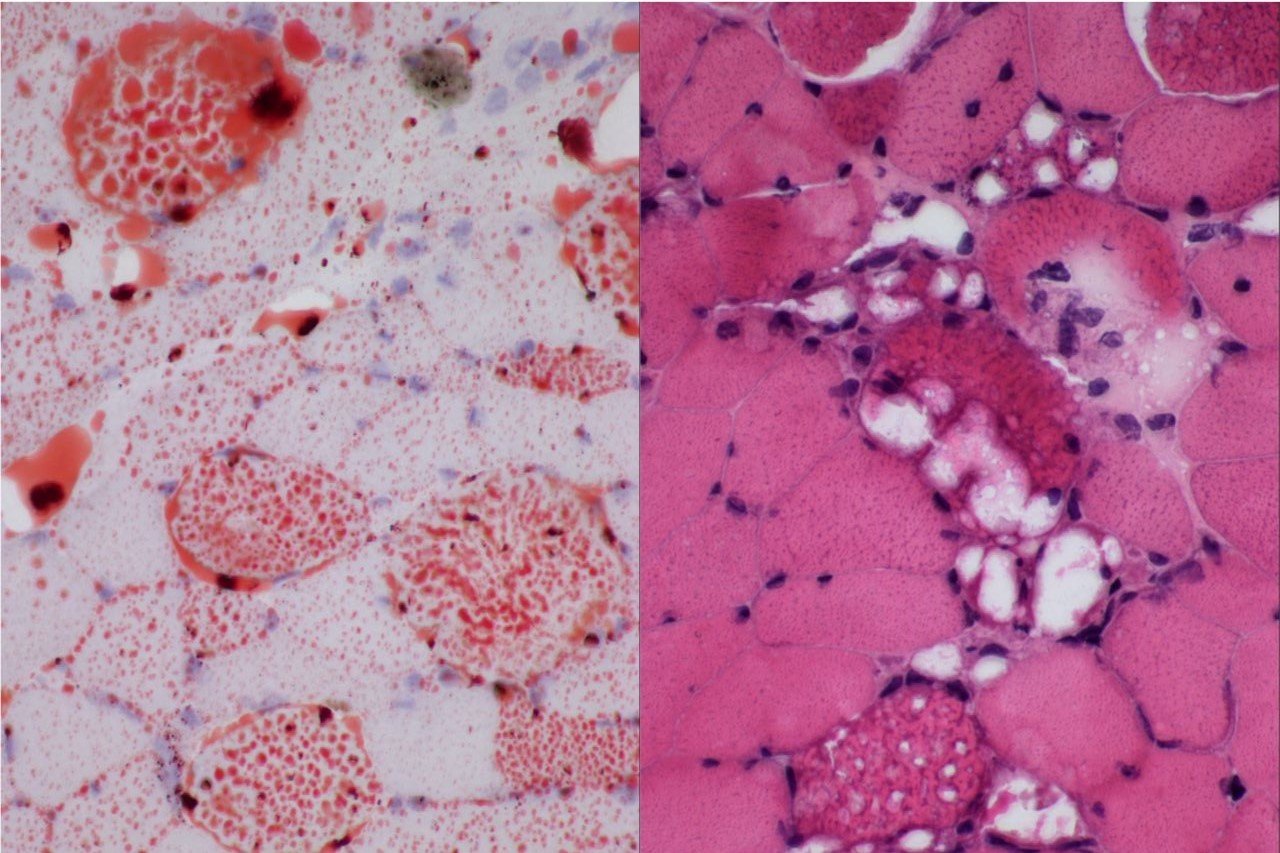
- Muscle biopsy may be performed to assess enzyme activity.
- Prenatal testing is available for families with a history of the disorder.
Treatment Options for Multiple Acyl-CoA Deficiency
While there is no cure for multiple acyl-CoA deficiency, treatment focuses on managing symptoms and preventing metabolic crises. A multidisciplinary approach is often required.
- Dietary management is crucial, with a focus on low-fat, high-carbohydrate diets.
- Medium-chain triglyceride (MCT) oil may be used as an alternative energy source.
- Riboflavin (vitamin B2) supplements can help improve enzyme function in some patients.
- Carnitine supplements may be prescribed to help transport fatty acids into cells.
- Emergency treatment during metabolic crises includes intravenous glucose and lipids.
Complications Associated with Multiple Acyl-CoA Deficiency
If not properly managed, multiple acyl-CoA deficiency can lead to serious health complications. Understanding these risks can help in early intervention and treatment.
- Recurrent metabolic crises can cause permanent organ damage.
- Hypoglycemia (low blood sugar) can lead to seizures and brain damage.
- Cardiomyopathy, a condition affecting the heart muscle, is a potential complication.
- Liver dysfunction and fatty liver disease may occur in some patients.
- Developmental delays and intellectual disabilities are possible in severe cases.
Living with Multiple Acyl-CoA Deficiency
Managing this condition requires ongoing medical care and lifestyle adjustments. Support from healthcare professionals and patient communities can make a significant difference.
- Regular follow-up with a metabolic specialist is essential for monitoring health.
- Patients should carry an emergency letter outlining their condition and treatment plan.
- Genetic counseling can provide valuable information for affected families.
- Support groups and online communities offer emotional support and practical advice.
- Advances in research may lead to new treatments and improved outcomes in the future.
Research and Future Directions
Ongoing research aims to better understand multiple acyl-CoA deficiency and develop new treatments. Scientists are exploring various approaches to improve patient care.
- Gene therapy holds promise for correcting the underlying genetic mutations.
- Enzyme replacement therapy is being investigated as a potential treatment.
- Researchers are studying the role of antioxidants in reducing oxidative stress.
- Clinical trials are testing new medications to enhance enzyme function.
- Collaboration between researchers, clinicians, and patient organizations is key to advancing knowledge and treatment options.
Final Thoughts on Multiple Acyl-CoA Deficiency
Multiple acyl-CoA deficiency, also known as MADD, is a rare metabolic disorder affecting the body's ability to break down fats and proteins. This condition can lead to a range of symptoms, from muscle weakness to severe metabolic crises. Early diagnosis and treatment are crucial for managing the disease and improving quality of life. Treatments often include dietary changes, supplements like riboflavin, and sometimes medications to manage symptoms. Genetic counseling can also be beneficial for families affected by MADD. Understanding the complexities of this disorder helps in providing better care and support for those living with it. Stay informed, consult healthcare professionals, and consider genetic testing if there's a family history of metabolic disorders. Knowledge and proactive management can make a significant difference.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
