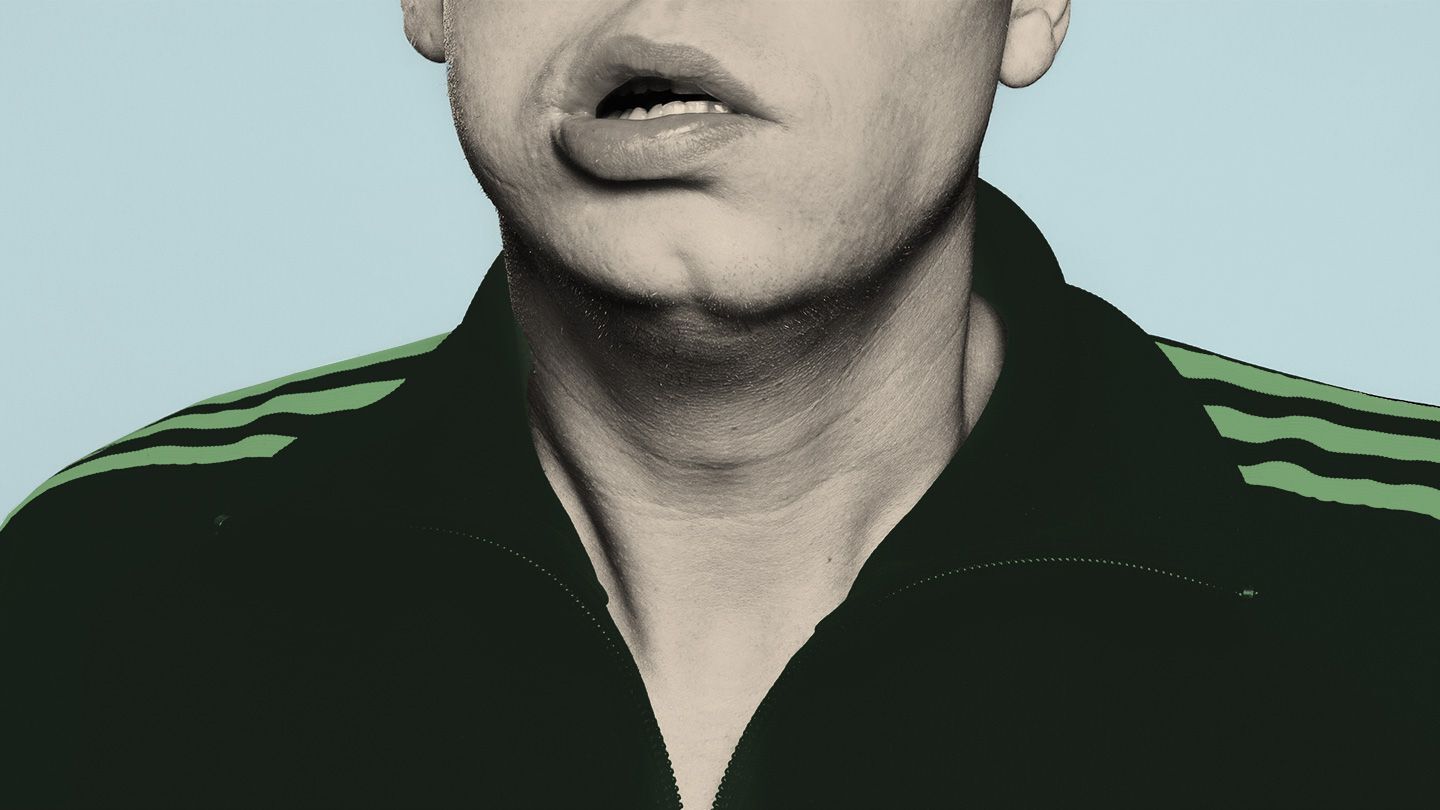
Oral Facial Dyskinesia is a condition that affects the muscles of the face, mouth, and jaw, causing involuntary movements. These movements can include grimacing, lip smacking, and rapid blinking. What causes Oral Facial Dyskinesia? Often, it results from long-term use of certain medications, especially antipsychotics. However, it can also be linked to neurological disorders or aging. This condition can impact daily activities like eating, speaking, and even social interactions. Understanding the symptoms, causes, and treatments is crucial for managing this disorder effectively. Let's dive into 25 key facts about Oral Facial Dyskinesia to help you grasp this complex condition better.
Key Takeaways:
- Oral Facial Dyskinesia (OFD) causes involuntary facial movements and speech difficulties, often due to long-term medication use. Treatment options include medication adjustment, Botox injections, and support groups for emotional and practical support.
- Living with OFD can impact social interactions, mental health, and work performance. Ongoing research aims to understand genetic factors, develop new medications, and improve early detection and intervention.
What is Oral Facial Dyskinesia?
Oral Facial Dyskinesia (OFD) is a movement disorder that affects the muscles of the face, mouth, and sometimes the jaw. This condition can cause involuntary movements, making everyday tasks challenging. Let's dive into some fascinating facts about OFD.
-
Involuntary Movements: OFD causes involuntary, repetitive movements of the facial muscles. These movements can include grimacing, lip smacking, and tongue protrusion.
-
Medication Side Effect: One of the primary causes of OFD is long-term use of certain medications, especially antipsychotics. These drugs can alter brain chemistry, leading to movement disorders.
-
Tardive Dyskinesia: OFD is often a symptom of Tardive Dyskinesia, a condition resulting from prolonged use of dopamine-blocking drugs. This highlights the importance of monitoring medication side effects.
-
Age Factor: Older adults are more susceptible to developing OFD, particularly those who have been on antipsychotic medications for extended periods.
-
Gender Differences: Women are more likely to develop OFD than men. Hormonal differences might play a role in this increased susceptibility.
Symptoms and Diagnosis
Recognizing the symptoms of OFD is crucial for early intervention. Diagnosis often involves a thorough medical history and physical examination.
-
Facial Tics: Common symptoms include facial tics, such as rapid blinking or eyebrow raising. These tics can be mild or severe, affecting daily life.
-
Speech Difficulties: OFD can cause speech difficulties due to involuntary movements of the tongue and lips. This can make communication challenging.
-
Chewing Problems: Involuntary jaw movements can lead to problems with chewing and swallowing, increasing the risk of choking.
-
Dental Issues: Constant movements can wear down teeth and cause other dental problems, necessitating frequent dental visits.
-
Neurological Exam: A neurologist may perform a detailed examination to assess the severity and impact of the movements on the patient's life.
Treatment Options
While there is no cure for OFD, various treatments can help manage the symptoms and improve quality of life.
-
Medication Adjustment: Reducing or changing the medication causing OFD can sometimes alleviate symptoms. This requires careful monitoring by a healthcare professional.
-
Botox Injections: Botox injections can help relax the facial muscles, reducing the severity of involuntary movements.
-
Speech Therapy: Speech therapy can assist individuals in improving their communication skills despite the challenges posed by OFD.
-
Occupational Therapy: Occupational therapists can provide strategies to manage daily tasks and improve overall functioning.
-
Support Groups: Joining support groups can offer emotional support and practical advice from others experiencing similar challenges.
Impact on Daily Life
Living with OFD can be challenging, but understanding its impact can help in finding ways to cope.
-
Social Interaction: Involuntary facial movements can affect social interactions, leading to embarrassment or social withdrawal.
-
Mental Health: The condition can take a toll on mental health, causing anxiety or depression. Seeking mental health support is essential.
-
Workplace Challenges: OFD can impact job performance, especially in roles requiring clear communication or fine motor skills.
-
Eating Habits: Difficulty in chewing and swallowing can lead to changes in eating habits and nutritional deficiencies.
-
Self-Esteem: The visible nature of the disorder can affect self-esteem and body image, making psychological support crucial.
Research and Future Directions
Ongoing research aims to better understand OFD and develop more effective treatments.
-
Genetic Factors: Researchers are exploring genetic factors that might predispose individuals to OFD, which could lead to targeted therapies.
-
New Medications: Development of new medications with fewer side effects could reduce the incidence of OFD in patients requiring long-term treatment.
-
Brain Stimulation: Techniques like deep brain stimulation are being investigated as potential treatments for severe cases of OFD.
-
Early Detection: Improved methods for early detection and intervention could prevent the progression of OFD.
-
Patient Education: Educating patients and healthcare providers about the risks and management of OFD is vital for improving outcomes.
Final Thoughts on Oral Facial Dyskinesia
Oral Facial Dyskinesia is a complex condition affecting many people. Understanding its causes, symptoms, and treatments can help those affected manage their condition better. From involuntary muscle movements to the impact on daily life, knowing these facts can make a big difference. Early diagnosis and proper medical care are crucial for improving quality of life. While there’s no cure, treatments like medication, therapy, and lifestyle changes can help manage symptoms. Staying informed and seeking professional advice are key steps in dealing with this condition. Remember, knowledge is power. By learning more about Oral Facial Dyskinesia, you’re taking an important step toward better health and well-being. Keep these facts in mind, and don’t hesitate to reach out to healthcare providers for support.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
