Autoinflammatory diseases (AIDs) are a group of rare disorders where the immune system mistakenly attacks the body, causing inflammation without an infection. These conditions are not the same as autoimmune diseases, though both involve the immune system. AIDs often result from genetic mutations, leading to symptoms like fever, rash, and joint pain. Understanding these diseases is crucial for early diagnosis and treatment, which can significantly improve quality of life. Did you know that AIDs can affect people of all ages, including children? They can be challenging to diagnose due to their rarity and overlapping symptoms with other conditions. Treatments often focus on reducing inflammation and managing symptoms. Research continues to advance, offering hope for better therapies and outcomes. Stay informed about these complex conditions to support those affected and raise awareness.
Key Takeaways:
- Autoinflammatory diseases (AIDs) are rare but serious conditions caused by genetic mutations affecting the body's innate immune system. Early diagnosis and management are crucial for preventing long-term complications.
- Treatment for AIDs focuses on managing symptoms and preventing complications. Lifestyle adjustments, support groups, and ongoing research offer hope for improved quality of life and future treatments.
Understanding Autoinflammatory Diseases
Autoinflammatory diseases (AIDs) are a group of disorders characterized by unprovoked inflammation due to a malfunction in the innate immune system. These conditions are distinct from autoimmune diseases, which involve the adaptive immune system. Let's explore some intriguing facts about these rare but impactful conditions.
-
Innate Immune System Malfunction
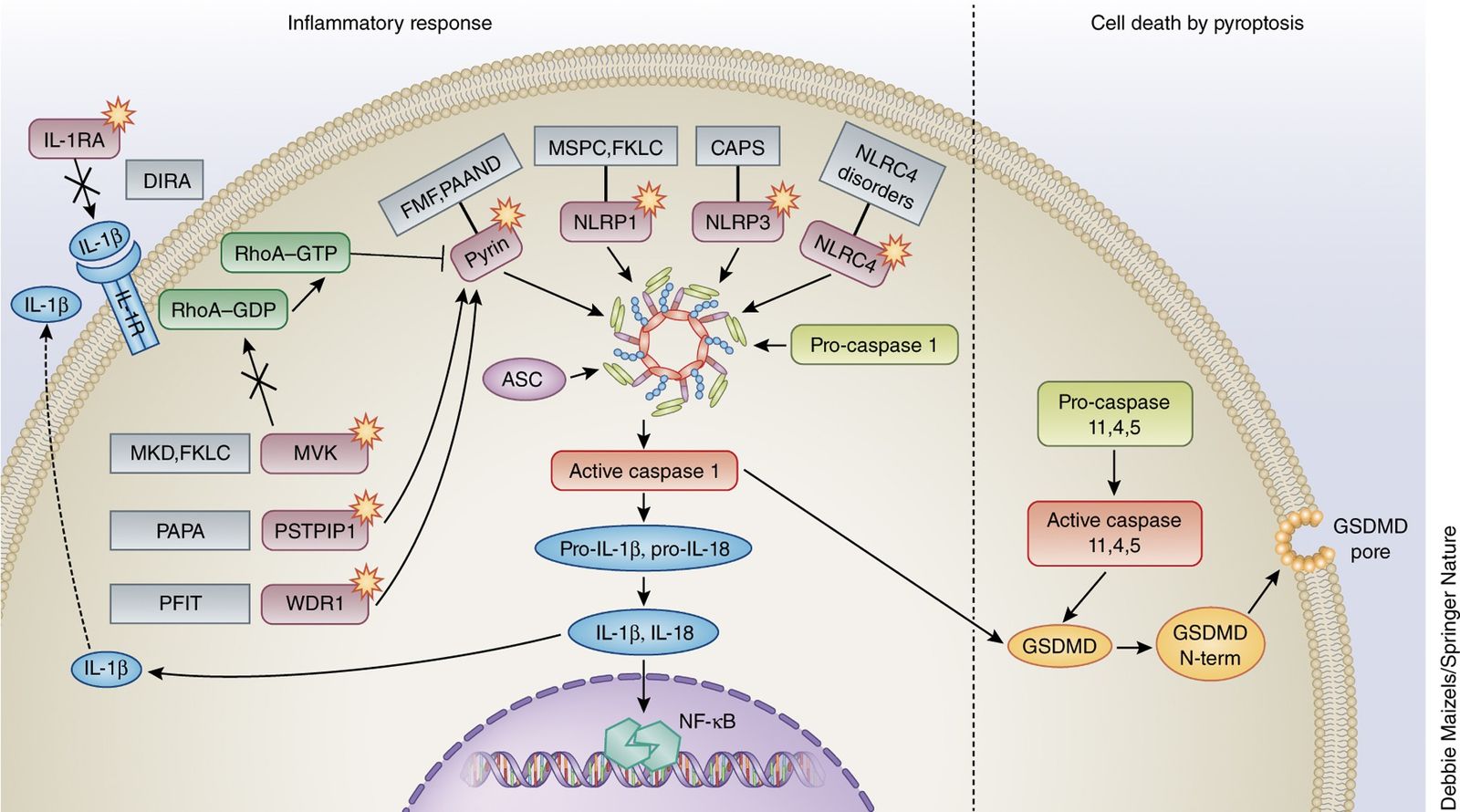
AIDs result from issues in the innate immune system, the body's first line of defense. Unlike autoimmune diseases, which involve antibodies, AIDs are caused by genetic mutations affecting proteins that regulate inflammation. -
Genetic Roots
Most AIDs are hereditary, passed down through families. Mutations in specific genes, like MEFV, NLRP3, and TNFRSF1A, are often responsible for these conditions. -
Periodic Fever Syndromes
Many AIDs are known as periodic fever syndromes. These include Familial Mediterranean Fever (FMF) and Hyper-IgD Syndrome (HIDS), characterized by recurrent fevers and inflammation. -
Rare but Serious
Though rare, AIDs can lead to severe complications if untreated. Chronic inflammation can damage organs and tissues, leading to long-term health issues. -
Early Onset
Symptoms often appear in childhood, sometimes within the first few months of life. Early diagnosis is crucial for managing symptoms and preventing complications.
Symptoms and Diagnosis
Recognizing the signs of AIDs can be challenging due to their rarity and overlap with other conditions. However, understanding common symptoms and diagnostic methods can aid in early detection.
-
Fever and Rash
Recurrent fevers and skin rashes are common symptoms. These can vary in severity and duration, often appearing without any apparent cause. -
Joint Pain and Swelling
Many individuals experience joint pain and swelling, similar to arthritis. This can lead to reduced mobility and discomfort. -
Abdominal Pain
Abdominal pain is another frequent symptom, often mistaken for other gastrointestinal issues. This pain can be severe and debilitating. -
Blood Tests for Inflammation
Doctors use blood tests to measure inflammation markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Elevated levels can indicate an inflammatory process. -
Genetic Testing
Genetic testing can confirm a diagnosis by identifying mutations associated with AIDs. This is especially useful for conditions with known genetic links.
Treatment and Management
While there's no cure for AIDs, treatments focus on managing symptoms and preventing complications. Understanding available therapies can improve quality of life for those affected.
-
Anti-inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. These are often the first line of treatment. -
Colchicine for FMF
Colchicine is a medication specifically effective for FMF. It helps prevent attacks and reduce inflammation. -
Biologic Therapies
Biologic drugs target specific components of the immune system. Medications like anakinra and canakinumab are used to treat certain AIDs. -
Corticosteroids
Corticosteroids can quickly reduce inflammation but are typically used short-term due to side effects. -
Lifestyle Adjustments
Diet, exercise, and stress management can play a role in managing symptoms. A healthy lifestyle supports overall well-being.
Living with Autoinflammatory Diseases
Living with AIDs requires ongoing management and support. Awareness and education can empower individuals and families affected by these conditions.
-
Support Groups
Connecting with others who have AIDs can provide emotional support and practical advice. Support groups offer a sense of community and understanding. -
Regular Medical Check-ups
Frequent visits to healthcare providers help monitor disease progression and adjust treatments as needed. -
Patient Education
Understanding one's condition is vital. Educated patients can better manage symptoms and advocate for their health needs. -
Family Planning Considerations
Genetic counseling can help families understand the risks of passing AIDs to children. This information is crucial for informed family planning. -
Research and Clinical Trials
Ongoing research aims to improve treatments and find cures. Participation in clinical trials can provide access to new therapies.
The Future of Autoinflammatory Disease Research
Research into AIDs is continually evolving, offering hope for better treatments and understanding of these complex conditions.
-
Gene Therapy Potential
Gene therapy holds promise for correcting genetic mutations causing AIDs. This approach could offer long-term solutions for some patients. -
New Drug Developments
Scientists are developing new drugs targeting specific inflammatory pathways. These could offer more effective and targeted treatments. -
Improved Diagnostic Tools
Advancements in genetic testing and biomarkers may lead to earlier and more accurate diagnoses. -
Understanding Disease Mechanisms
Research into the underlying mechanisms of AIDs is expanding. This knowledge could lead to breakthroughs in treatment and prevention. -
Global Collaboration
International research collaborations are crucial for advancing knowledge and treatment of rare diseases like AIDs. Sharing data and resources accelerates progress.
Final Thoughts on Autoinflammatory Diseases
Autoinflammatory diseases, often misunderstood, are crucial to recognize for their unique characteristics. These conditions, unlike autoimmune diseases, arise from innate immune system malfunctions, leading to unprovoked inflammation. Understanding these diseases helps in early diagnosis and effective management, improving patients' quality of life. Recent research and advancements in genetic testing have paved the way for better treatments, offering hope to those affected. It's vital for both patients and healthcare providers to stay informed about the latest developments in this field. Raising awareness can lead to more research funding and support for those living with these conditions. By fostering a supportive community, we can ensure that individuals with autoinflammatory diseases receive the care and understanding they deserve. Keep learning and advocating for those impacted by these complex conditions, as knowledge and empathy are powerful tools in the fight against them.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
