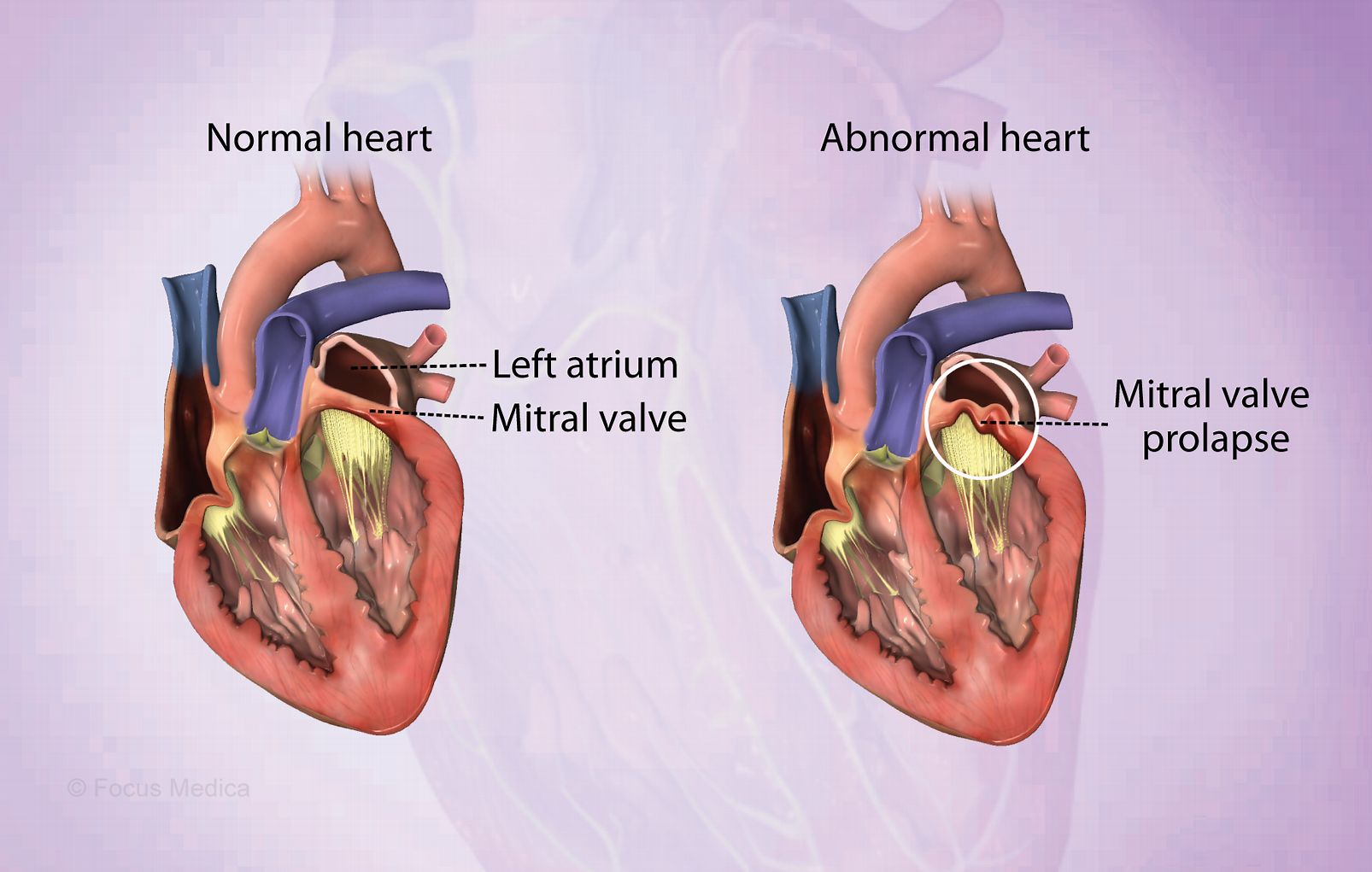
What is Mitral Valve Prolapse (MVP)? It's a heart condition where the mitral valve leaflets bulge into the left atrium during the heart's contraction. Affecting about 2-3% of the U.S. population, MVP is often benign but can lead to serious issues like mitral regurgitation, infective endocarditis, and even sudden cardiac death. Most people with MVP don't show symptoms, but some might experience chest pain, palpitations, or dizziness. Diagnosis usually involves echocardiography to visualize the prolapsing leaflets. While surgery is reserved for severe cases, less invasive procedures can improve quality of life. Understanding MVP's complexities helps in managing and treating this condition effectively.
Key Takeaways:
- Mitral Valve Prolapse (MVP) affects 2-3% of the US population and can lead to symptoms like chest pain, fast heartbeat, and dizziness. It's crucial to monitor and manage this condition to prevent long-term complications.
- MVP is diagnosed through clinical presentation and echocardiography. Lifestyle changes, regular monitoring, and an interdisciplinary approach involving healthcare professionals are essential for effective management.
What is Mitral Valve Prolapse?
Mitral Valve Prolapse (MVP) is a heart condition where the mitral valve leaflets bulge into the left atrium during systole. This can lead to various symptoms and complications. Let's dive into some essential facts about MVP.
-
Definition: MVP is defined by the systolic displacement of one or more abnormally thickened, redundant mitral leaflet(s) into the left atrium during systole.
-
Prevalence: It affects 2-3% of the population in the United States.
-
Causes: The most common cause is myxomatous degeneration of the mitral valve leaflets, leading to structural incompetence and superior displacement of the leaflets.
-
Pathophysiology: Myxomatous degeneration involves the accumulation of mucopolysaccharides and collagen in the valve tissue, causing redundancy and thickening of the leaflets.
-
Symptoms: Most people with MVP have no symptoms. However, some may experience chest pain, fast heartbeat, awareness of heartbeats, severe headaches (migraines), feeling tired and weak, dizziness, and a drop in blood pressure when standing up.
How is Mitral Valve Prolapse Diagnosed?
Identifying MVP often begins with a routine check-up. Doctors use various methods to diagnose this condition accurately.
-
Clinical Presentation: The condition is usually identified during cardiac auscultation, where a doctor hears a clicking sound while listening to the heart with a stethoscope.
-
Diagnosis: Echocardiography confirms the diagnosis by visualizing the prolapsing leaflets and assessing for mitral regurgitation.
-
Etiology: MVP often occurs as an isolated condition but can also be associated with heritable disorders of connective tissue, such as Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, and pseudoxanthoma elasticum.
-
Genetic Factors: The majority of data suggest an autosomal dominant inheritance pattern in a large proportion of individuals with MVP.
-
Risk Factors: Older age, certain infections that affect the heart, heart attack, and some types of heart disease increase the risk of mitral valve disease.
Complications of Mitral Valve Prolapse
While MVP is often benign, it can lead to serious complications. Understanding these risks is crucial for managing the condition effectively.
-
Complications: MVP can lead to serious complications such as clinically significant mitral regurgitation, infective endocarditis, sudden cardiac death, and cerebrovascular ischemic events.
-
Mitral Regurgitation: The condition often results in mitral regurgitation, where blood leaks backward from the left ventricle into the left atrium during systole.
-
Barlow Syndrome: In younger populations, MVP is characterized by gross redundancy of both the anterior and posterior leaflets and chordal apparatus, known as Barlow syndrome.
-
Fibroelastic Deficiency: In older populations, MVP is characterized by fibroelastic deficiency, sometimes with superimposed chordal rupture due to a lack of connective tissue support.
-
Malcoaptation: The anatomic abnormalities in MVP result in malcoaptation of mitral valve leaflets during systole, leading to regurgitation.
Long-term Effects and Management
Managing MVP involves monitoring and sometimes treating the condition to prevent long-term effects. Here are some key points about its management.
-
Mitral Annular Dilatation: Over time, mitral annular dilatation may develop, further progressing mitral regurgitation.
-
Congestive Heart Failure: Acute severe MR can result in congestive heart failure symptoms without left ventricular dilatation.
-
Ventricular Dysfunction: Chronic or progressively severe MR can lead to ventricular dilatation and dysfunction, neurohormonal activation, and heart failure.
-
Left Atrial Enlargement: Elevation in left atrial pressures can result in left atrial enlargement, atrial fibrillation, pulmonary congestion, and pulmonary hypertension.
-
Myxomatous Proliferation: Myxomatous proliferation is the most common pathologic basis for MVP, leading to myxomatous degeneration of the loose spongiosa and fragmentation of collagen fibrils.
Surgical and Non-Surgical Treatments
Treatment options for MVP range from medication to surgery, depending on the severity of the condition.
-
Surgical Correction: Currently, only surgical correction of MVP is curative, but it is reserved for severe cases where irreversible complications may already be established.
-
Less Invasive Procedures: Less invasive percutaneous catheter-based procedures are available for patients who are not ideal candidates for surgery and have been shown to improve quality of life, reduce rehospitalizations, and promote favorable ventricular remodeling.
-
Prevalence in Syndromes: MVP has been described in association with various genetic syndromes, including osteogenesis imperfecta, fragile X syndrome, Down syndrome, and Pseudoxanthoma elasticum.
-
Overestimation of Prevalence: Some disorders previously believed to have an increased prevalence of MVP may be overestimating the prevalence due to the lack of up-to-date diagnostic criteria.
-
Cardiovascular Morbidity: Despite its benign nature, MVP poses a significant disease burden and is a major contributor to cardiovascular morbidity and mortality.
Global Impact and Statistics
MVP affects millions worldwide. Understanding its global impact helps in recognizing its significance.
-
Global Prevalence: It is hypothesized that >7.8 million people in the United States and >176 million people worldwide are living with MVP.
-
Surgical Intervention: Approximately 0.2% to 3.5% of patients with prolapse will require surgery for their condition at some point in their lifetime, depending on their demographics.
-
Surgical Risks: Mitral valve surgery carries significant risks but is highly effective at preventing mortality in patients with severe regurgitation.
-
Non-Surgical Management: Non-surgical management options include beta-blockers to slow the heart rate and ease symptoms in symptomatic patients.
-
Interprofessional Team: An interprofessional team approach is crucial for the management of MVP, involving cardiologists, cardiac surgeons, and other healthcare professionals.
Exercise and Lifestyle Considerations
Lifestyle changes and exercise can play a role in managing MVP. Here are some recommendations.
-
Exercise Recommendations: Exercise recommendations for patients with valvular heart disease, including MVP, should be tailored to the individual's condition and risk factors.
-
Risk Factors for Complications: Certain risk factors, such as older age and underlying heart conditions, increase the likelihood of complications from MVP.
-
Infective Endocarditis: Patients with MVP are at an increased risk of developing infective endocarditis due to endothelial disruption.
-
Thromboembolic Complications: Disruption of the endothelium also predisposes patients to thromboembolic complications, such as stroke.
-
Atrial Fibrillation: Elevated left atrial pressures can lead to atrial fibrillation, further complicating the clinical course of MVP.
Potential Complications and Risks
Understanding the potential complications and risks associated with MVP is essential for effective management.
-
Pulmonary Congestion: Pulmonary congestion and pulmonary hypertension are potential complications arising from left atrial enlargement and elevated pressures.
-
Heart Failure: Chronic or severe MR can lead to heart failure, characterized by symptoms such as fatigue, shortness of breath, and swelling in the legs.
-
Ventricular Remodeling: Less invasive procedures can promote favorable ventricular remodeling, improving quality of life and reducing rehospitalizations.
-
Quality of Life: While less invasive procedures do not improve survival at 1 year, they can significantly improve quality of life for patients with MVP.
-
Rehospitalizations: These procedures have been shown to reduce rehospitalizations, which is crucial for managing chronic conditions like MVP.
Research and Studies
Research and studies provide valuable insights into MVP, helping to improve diagnosis and treatment.
-
Framingham Heart Study: The Framingham Heart Study offspring cohort disputed initial findings that MVP was associated with various diseases, arguing that many of these associations were made in hospital-based cohorts and therefore patients were sicker and more likely to have comorbid disease.
-
Community Study: A community study of asymptomatic patients with MVP reported a more heterogeneous clinical course than described in the Framingham study, highlighting the variability in patient outcomes.
-
Heterogeneous Clinical Course: The clinical course of MVP can be highly variable, ranging from asymptomatic to severe complications requiring surgical intervention.
-
Sudden Cardiac Death: Although rare, MVP can lead to sudden cardiac death, particularly in patients with severe regurgitation or underlying heart conditions.
-
Cerebrovascular Accident: The condition also increases the risk of cerebrovascular accidents, such as stroke, due to thromboembolic complications.
Preventive Measures and Guidelines
Preventive measures and guidelines help manage MVP and reduce the risk of complications.
-
Infective Endocarditis Risk: Patients with MVP are at an increased risk of developing infective endocarditis, which can be life-threatening if not promptly treated.
-
Management Guidelines: A review of clinical guidelines to allow for earlier surgical intervention may be warranted to lower cardiovascular risk in patients with MVP.
-
Interdisciplinary Care: Effective management of MVP requires an interdisciplinary approach involving cardiologists, cardiac surgeons, and other healthcare professionals to ensure comprehensive care and optimal outcomes.
-
Lifestyle Modifications: Patients with MVP should consider lifestyle modifications, such as maintaining a healthy diet, exercising regularly, and avoiding excessive caffeine and alcohol.
-
Regular Monitoring: Regular monitoring and follow-up with a healthcare provider are essential for managing MVP and preventing complications.
Understanding Mitral Valve Prolapse
Mitral Valve Prolapse (MVP) affects millions globally. While often benign, it can lead to serious complications like mitral regurgitation, heart failure, and even sudden cardiac death. Early diagnosis through echocardiography and regular monitoring is crucial. Symptoms vary widely, from none at all to chest pain and dizziness. Genetic factors play a role, and it's sometimes linked to connective tissue disorders like Marfan syndrome. Treatment ranges from lifestyle changes and medications to surgical interventions for severe cases. Less invasive procedures are also available, improving quality of life and reducing hospital visits. An interdisciplinary approach involving cardiologists and surgeons ensures comprehensive care. Understanding MVP's complexities helps in managing it effectively, highlighting the importance of early detection and appropriate treatment.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.