What is Coccidioidomycosis? Coccidioidomycosis, often called Valley fever, is a fungal infection caused by Coccidioides immitis and Coccidioides posadasii. This disease primarily affects the lungs but can spread to other parts of the body. Found in the soil of the southwestern United States and parts of Mexico, the fungi become airborne when the soil is disturbed. People inhale the spores, leading to infection. Symptoms range from mild, flu-like signs to severe, life-threatening conditions. While many infected individuals show no symptoms, others may experience fever, cough, and fatigue. High-risk groups include immunocompromised individuals and pregnant women. Understanding this disease is crucial for those living in or traveling to endemic areas.
Key Takeaways:
- Coccidioidomycosis, also known as Valley fever, is a fungal infection prevalent in specific regions. It can range from mild to severe, with symptoms including tiredness, fever, cough, and joint pain.
- The disease is endemic to the western hemisphere, mainly in the southwestern United States and northern Mexico. High-risk groups include immunocompromised individuals, pregnant women, and those with occupational exposure to potentially infected dust.
What is Coccidioidomycosis?
Coccidioidomycosis, also known as Valley fever, is a fungal infection caused by Coccidioides immitis and Coccidioides posadasii. This disease is prevalent in certain regions and can range from mild to severe. Let's dive into some key facts about this infection.
- Definition: Coccidioidomycosis is a mammalian fungal disease caused by Coccidioides immitis or Coccidioides posadasii.
- Common Names: The disease is also known as cocci, Valley fever, California fever, desert rheumatism, or San Joaquin Valley fever.
- History: The first reported case was in an Argentinian soldier in 1892, who had skin lesions for four years. Initially, the organism was thought to be a protozoan.
Symptoms and Clinical Presentation
Understanding the symptoms and how the disease presents itself is crucial for early diagnosis and treatment.
- Clinical Presentation: The disease can range from asymptomatic to severe, with the primary infection often resembling bronchitis or pneumonia.
- Symptoms: Common symptoms include tiredness, loss of smell and taste, fever, cough, headaches, rash, muscle pain, and joint pain.
- Asymptomatic Infection: About 60% of people infected show minimal to no symptoms but may still develop delayed hypersensitivity to a coccidioidal skin test.
- Types of Infection: The spectrum includes asymptomatic infection, uncomplicated primary infection, fibro-cavitary pulmonary infection, and extra-thoracic dissemination.
Geographic Distribution and Incidence
Coccidioidomycosis is more common in specific regions. Knowing where it is prevalent can help in understanding the risk factors.
- Incidence: The disease is endemic to the western hemisphere between 40°N and 40°S, mainly in the southwestern United States and northern Mexico.
- Ecological Niche: The fungi thrive in alkaline sandy soil, typically 10–30 cm below the surface, with incidence increasing after periods of dryness following rain.
- Transmission: Infection is typically acquired by inhaling airborne arthroconidia, which are single-cell fragments of mycelia that become airborne after soil disruption.
Risk Factors and Occupational Exposure
Certain groups and occupations are at higher risk of contracting coccidioidomycosis.
- Risk Factors: Immunocompromised individuals and pregnant women are at higher risk of severe and disseminated infections.
- Occupational Exposure: High exposure to potentially infected dust is a risk for certain occupations, like archaeological site workers.
- Geographic Distribution: Endemic in Arizona, California, Nevada, New Mexico, Texas, Utah, and northern Mexico, with cases also occurring in non-endemic areas due to travel.
Clinical Forms and Chronic Infection
The disease can manifest in various forms, from acute to chronic infections.
- Annual Cases: An estimated 150,000 infections occur annually in the U.S., with about 0.5% resulting in dissemination.
- Underreporting: Epidemiological models suggest that reported infections underestimate actual cases by 6- to 14-fold.
- Clinical Forms: The disease can manifest as acute, chronic, and disseminated infections, with chronic fibrocavitary disease characterized by cough, fevers, night sweats, and weight loss.
- Chronic Infection: A minority (3–5%) of infected individuals develop chronic infection, which can be a chronic lung infection or widespread disseminated infection.
Severe and Disseminated Infections
Severe cases can lead to more serious health issues, including dissemination to other parts of the body.
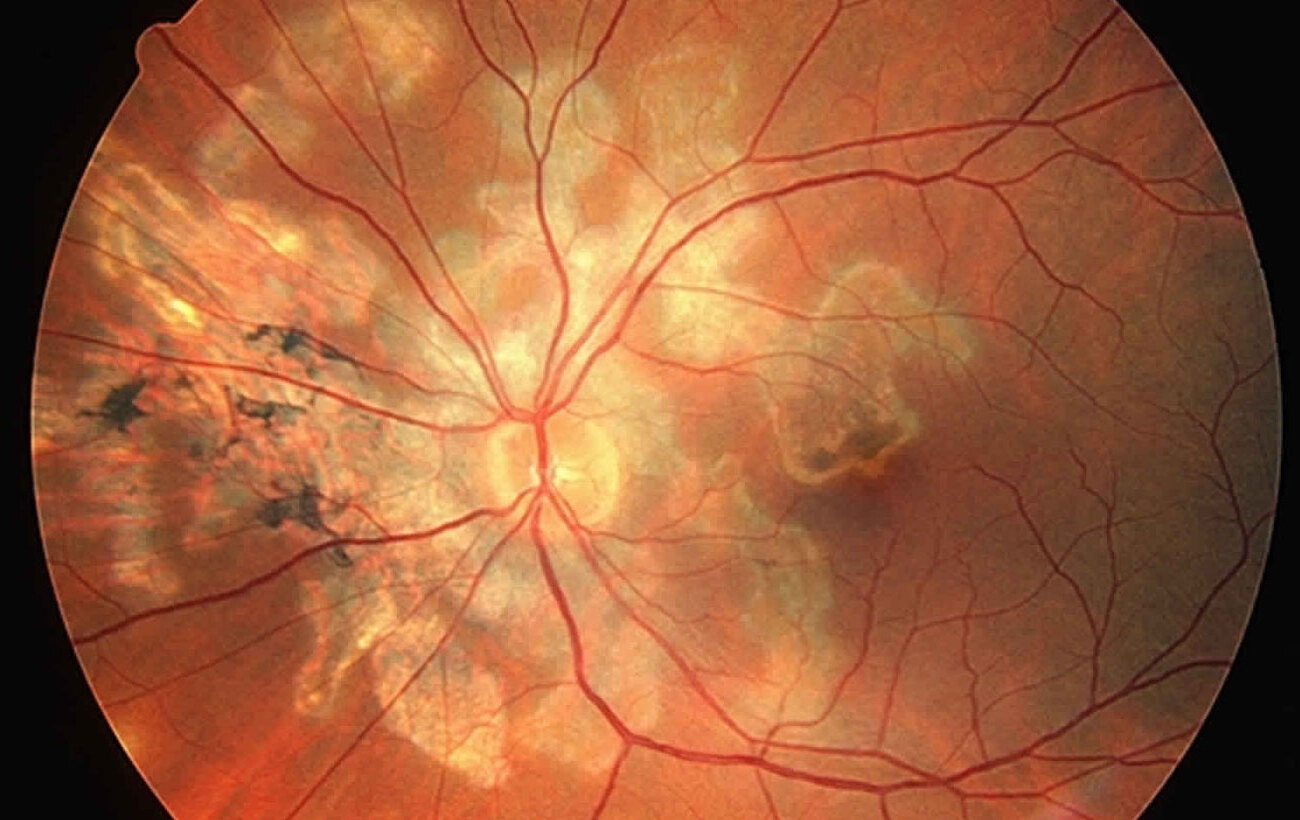
- Disseminated Infection: Disseminated coccidioidomycosis (DCM) is a severe spread of infection beyond the lungs, affecting tissues lining the brain, soft tissues, joints, and bone.
- Osteomyelitis: Osteomyelitis, including spinal involvement, and meningitis may occur months to years after initial infection.
- Vaccine Development: Researchers are working on developing an effective vaccine, though challenges include the complex immune response and need for a multi-valent vaccine.
Treatment and Historical Perspectives
Treatment options and historical insights provide a deeper understanding of how the disease has been managed over time.
- Treatment: Primary treatment involves antifungal medication like Amphotericin B, itraconazole, and fluconazole, depending on the severity and type of infection.
- Historical Perspectives: The first two U.S. cases were reported in 1902, with marked differences in clinical presentation.
- Fungal Nature: The fungal nature of the organism was identified four years after the initial cases by Ophuls and Moffitt.
Laboratory Insights and Public Health
Laboratory research and public health measures are essential in managing and preventing coccidioidomycosis.
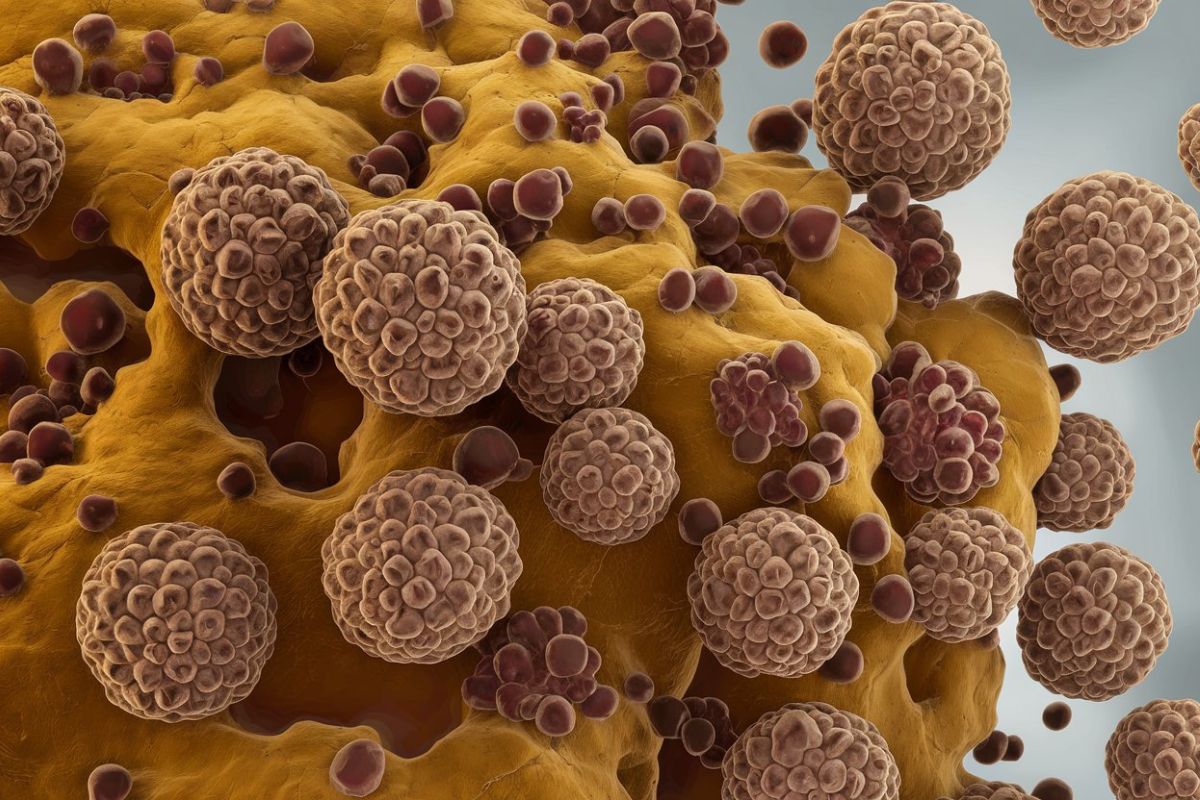
- Dimorphic Fungi: Coccidioides is a dimorphic fungus, changing from a mold to the “protozoan” phase in tissue and sprouting hyphae in a coverslip preparation.
- Laboratory Accidents: A lab accident provided insight into milder forms of infection when a medical student accidentally inhaled spores.
- Public Health Importance: Preventing coccidioidomycosis is challenging, but understanding its public health impact is essential in endemic areas.
Epidemiological Models and Risk Factors
Epidemiological models help in understanding the true extent of the disease and identifying high-risk groups.
- Epidemiological Models: Models suggest actual cases are significantly higher than reported due to mild or asymptomatic infections.
- Risk Factors for Severe Disease: Immunocompromised individuals and pregnant women are at higher risk of severe infections, as are those treated with tumor necrosis factor alpha antagonists.
- Occupational Exposure in Archaeological Sites: Workers at archaeological sites, like Dinosaur National Monument in Utah, have been exposed due to soil disturbance.
Travel-Related Cases and Clinical Spectrum
Travel-related cases and the wide clinical spectrum of the disease highlight its complexity.
- Travel-Related Cases: Cases outside endemic areas are generally visitors who contracted the infection and returned home before becoming symptomatic.
- Clinical Spectrum: The clinical spectrum includes asymptomatic infection, uncomplicated primary infection, fibro-cavitary pulmonary infection, and extra-thoracic dissemination.
Histopathological Changes and Research Efforts
Histopathological changes and ongoing research efforts are crucial for better understanding and managing the disease.
- Histopathological Changes: Lung infections show large fibrocaseous nodules, characteristic of chronic fibrocavitary disease.
- NIH-Mycoses Study Group: This group has conducted studies on antifungal drugs to treat disseminated coccidioidomycosis, providing valuable insights into treatment options.
Molecular and Phenotypic Description
Molecular and phenotypic descriptions help distinguish between different species of the fungus.
- Molecular and Phenotypic Description: Coccidioides posadasii was previously recognized as the non-California population of Coccidioides immitis.
- Risk Factors in Select Racial and Ethnic Groups: Research is ongoing to identify host factors in select racial and ethnic groups that increase the risk of developing coccidioidomycosis.
Climate Change and Environmental Detection
Climate change and improved environmental detection methods play a role in understanding and managing the disease.
- Climate Change Impact: Warmer temperatures and altered precipitation patterns may affect the growth and dispersal of the fungus, potentially increasing the incidence of the disease.
- Improved Environmental Detection Methods: Researchers are working to develop better methods for detecting Coccidioides in the environment.
Treatment Regimens and Transmission
Establishing optimal treatment regimens and understanding transmission methods are key to managing the disease.
- Optimal Treatment Regimen: Research aims to identify the most effective antifungal medications and treatment durations for primary pulmonary infections.
- Fomite-Transmitted Infection: Fomite-transmitted coccidioidomycosis has been reported in immunocompromised children, highlighting the potential for secondary transmission.
Organ Transplant and HIV-Related Cases
Special cases involving organ transplants and HIV-infected individuals require careful management.
- Donor-Derived Organ Transplant Transmission: Documented cases emphasize the need for thorough screening of organ donors to prevent fungal infection transmission.
- Coccidioidomycosis in HIV-Infected Persons: The disease can progress to severe lung disease in HIV-infected individuals, highlighting the need for early diagnosis and treatment.
Pregnancy and Solid Organ Transplantation
Pregnancy and solid organ transplantation present unique challenges in managing coccidioidomycosis.
- Coccidioidomycosis during Pregnancy: Pregnant women have a higher risk of disseminated infection, requiring antifungal therapy and close monitoring.
- Coccidioidomycosis in Solid Organ Transplantation: The immunosuppressed state of these patients increases their susceptibility to severe forms of the disease.
TNF-Alpha Antagonists and Cutaneous Infections
Certain medications and rare forms of the disease present additional challenges.
- Increased Risk with TNF-Alpha Antagonists: Patients treated with these antagonists are at increased risk, necessitating careful monitoring and preventive measures.
- Primary Cutaneous Coccidioidomycosis: This rare form presents as skin lesions and can be associated with systemic infections in immunocompromised individuals.
Genetic Determinants and Non-Endemic Areas
Genetic factors and cases in non-endemic areas provide further insights into the disease.
- Genetic and Other Determinants for Severity: Polymorphisms identified in patients with disseminated coccidioidomycosis help understand disease patterns.
- Coccidioidomycosis in Non-Endemic Areas: Cases have been reported in individuals who traveled to endemic regions and returned with the infection.
Fungal Ecology and Public Health Response
Understanding the fungus's ecology and enhancing public health awareness are crucial for managing the disease.
- Fungal Ecology: Coccidioides resides in hot, sandy soil with alkaline properties, typically 10–30 cm below the surface.
- Public Health Response: Educating healthcare providers, public health professionals, and the general public about the disease is essential in endemic regions.
Ongoing Research and Surveillance
Ongoing research aims to improve surveillance, testing, and treatment of coccidioidomycosis.
- Ongoing Research: Efforts include identifying risk factors, developing effective vaccines, and improving environmental detection methods to better manage the disease.
Key Takeaways on Coccidioidomycosis
Coccidioidomycosis, or Valley fever, is a fungal infection caused by Coccidioides immitis and Coccidioides posadasii. Found mainly in the southwestern U.S. and northern Mexico, it often presents with flu-like symptoms but can be severe, especially in immunocompromised individuals. Most infections are mild or asymptomatic, but some can lead to chronic or disseminated disease. Risk factors include exposure to contaminated soil, certain occupations, and weakened immune systems. Treatment typically involves antifungal medications like Amphotericin B, itraconazole, and fluconazole. Researchers are working on vaccines and better detection methods. Understanding this disease's impact is crucial for those living in or traveling to endemic areas. Public health awareness and ongoing research are key to managing and preventing coccidioidomycosis effectively.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.