Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare autoimmune disorder where the body's immune system mistakenly attacks the myelin sheath, a protective covering around nerves. This leads to progressive weakness and sensory loss in the limbs. CIDP can be tricky to diagnose due to its varied symptoms and the need for specialized tests like electromyography (EMG) and nerve conduction studies (NCS). Treatment often involves immunomodulatory therapies such as plasma exchange, intravenous immunoglobulin (IVIG), and corticosteroids. Early diagnosis and treatment are crucial to prevent irreversible nerve damage and improve quality of life. Understanding CIDP is essential for managing this challenging condition effectively.
Key Takeaways:
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare autoimmune disorder affecting the nerves, causing weakness and sensory loss, often starting in the legs and requiring early diagnosis for effective treatment.
- CIDP can present in various clinical patterns, such as ataxic, pure motor, and pure sensory, making diagnosis and treatment complex. It requires ongoing management and coordination among healthcare professionals for effective care.
What is Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)?
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare neurological disorder that affects the peripheral nerves. It is characterized by progressive weakness and impaired sensory function in the limbs. Let's dive into some key facts about this condition.
-
CIDP is an acquired autoimmune disease of the peripheral nervous system. The immune system mistakenly attacks the myelin sheath, leading to progressive weakness and sensory loss.
-
Symptoms typically start in the legs. Patients often report difficulty getting out of a chair, walking, climbing stairs, and falling.
-
Upper limb involvement can cause problems with gripping objects. Tasks like tying shoelaces and using utensils become challenging.
Clinical Characteristics and Symptoms
Understanding the clinical characteristics and symptoms of CIDP is crucial for early diagnosis and treatment.
-
Proximal limb weakness is a fundamental clinical characteristic. This distinguishes CIDP from most distal polyneuropathies.
-
Sensory involvement includes proprioception impairment. Patients may experience distal paresthesias, loss of feeling, and poor balance.
-
Only a small percentage of cases involve neuropathic pain. Most patients experience motor and sensory impairments without significant pain.
-
Fatigue is common in CIDP patients. It is unclear how much this is due to primary effects or secondary effects of the disease.
Variations in Clinical Patterns
CIDP can present in various clinical patterns, making diagnosis and treatment more complex.
-
CIDP can present in ataxic, pure motor, and pure sensory patterns. Multifocal patterns also exist, where specific nerve territories experience weakness and sensory loss.
-
Ataxic patterns involve coordination and balance issues. Patients may have difficulty walking, standing, and performing fine motor tasks.
-
Pure motor patterns involve only motor symptoms. There is no sensory involvement, leading to significant limb weakness.
-
Pure sensory patterns involve only sensory symptoms. There is no motor weakness, but significant sensory disturbances.
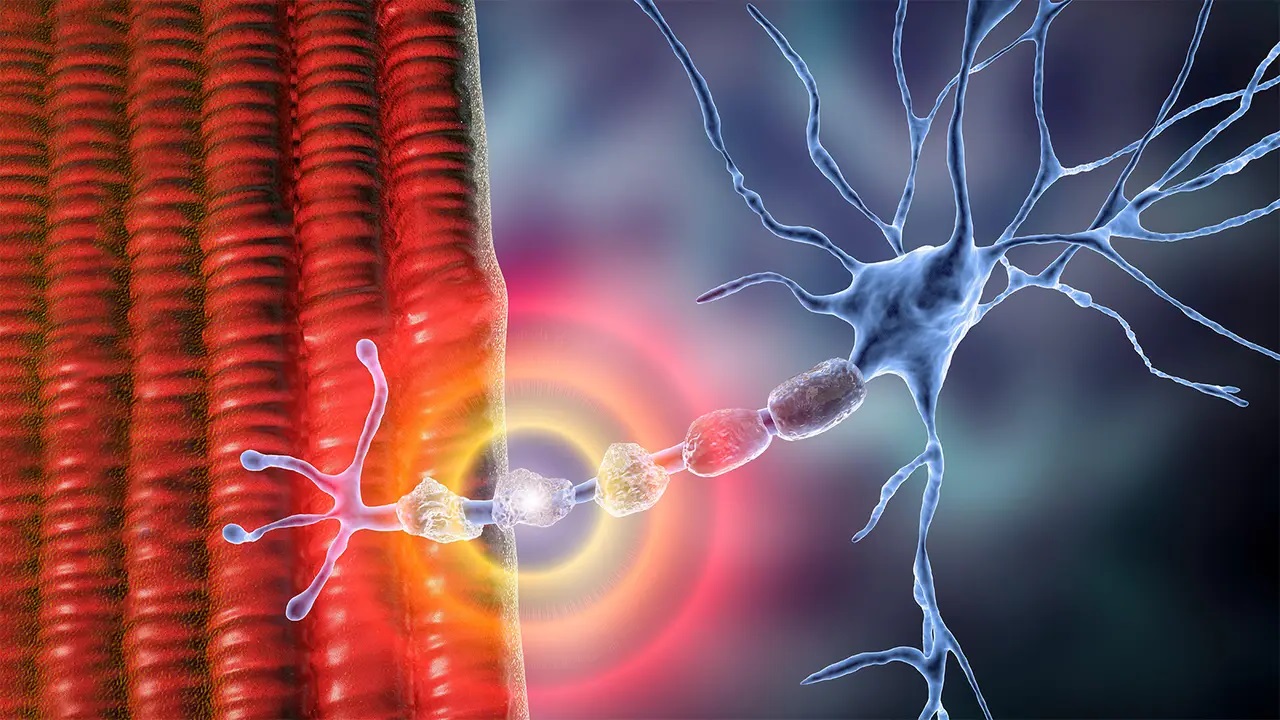
Autoimmune Nature and Myelin Sheath Destruction
The autoimmune nature of CIDP leads to the destruction of the myelin sheath, affecting nerve signal transmission.
-
CIDP is considered an autoimmune disorder. The immune system attacks the myelin sheath, leading to demyelination and remyelination.
-
The myelin sheath is crucial for rapid nerve signal transmission. Loss or damage to the myelin sheath can cause slowing or blockage of nerve signals.
-
Motor impairments typically affect both sides of the body symmetrically. This causes weakness and paralysis.
-
Sensory disturbances may also be present. Vibration and position sense are more affected than pain and temperature sense.
Diagnostic Challenges and Tools
Diagnosing CIDP can be challenging due to its heterogeneous presentation and the limitations of diagnostic criteria.
-
CIDP is characterized by ongoing symptoms for over 8 weeks. This distinguishes it from acute inflammatory demyelinating polyneuropathy (AIDP).
-
Diagnosing CIDP can be challenging. Early diagnosis and treatment are crucial to prevent irreversible axonal loss.
-
Electrodiagnostic studies are essential in confirming the diagnosis. These include electromyography (EMG) and nerve conduction studies (NCS).
-
Cerebrospinal fluid analysis can help in diagnosis. Increased protein content in the CSF is often observed in CIDP patients.
Treatment Options
Various treatment options are available for CIDP, focusing on immunomodulatory therapies.
-
Treatment options for CIDP include plasma exchange, intravenous immunoglobulin (IVIG), and corticosteroids. The choice of treatment depends on the severity and progression of the disease.
-
Plasma exchange involves removing plasma from the blood. It is replaced with a substitute solution to reduce autoantibodies attacking the myelin sheath.
-
IVIG involves administering antibodies. These antibodies help modulate the immune response and reduce inflammation.
-
Corticosteroids, such as prednisone, are often used. They reduce inflammation and suppress the immune system but may have significant side effects.
Long-term Management and Interprofessional Team Coordination
Effective management of CIDP requires long-term strategies and coordination among healthcare professionals.
-
Long-term management involves maintenance therapies to prevent relapses. This may include ongoing immunomodulatory treatments and regular monitoring.
-
Effective management requires coordination among an interprofessional team. This includes neurologists, physical therapists, and other healthcare professionals.
-
Regular follow-up appointments are crucial. They help adjust treatment plans as needed and monitor for potential side effects.
Epidemiology and Risk Factors
CIDP is a rare disorder with specific risk factors and epidemiological characteristics.
-
CIDP is estimated to affect approximately 1 in 100,000 people worldwide. Its exact prevalence is difficult to determine due to under-recognition and under-treatment.
-
HIV infection is a known risk factor for CIDP. Distinct patterns of CIDP have been noted at every stage of HIV infection.
-
Pregnancy has been linked to a significantly greater risk of relapse. Hormonal changes or other factors associated with pregnancy may contribute to this risk.
-
In some cases, CIDP may be triggered by infections or vaccinations. A study found that 32% of CIDP patients had a history of vaccination or infection within 6 weeks of the onset of symptoms.
Genetic Predisposition and Disease Progression
Understanding the genetic predisposition and progression of CIDP can help in managing the condition.
-
There is no known genetic predisposition to CIDP. The condition is considered an acquired autoimmune disorder.
-
The progression of CIDP can vary significantly from person to person. Some individuals may follow a slow steady pattern, while others may experience symptoms that stabilize and then relapse.
-
Multifocal patterns involve specific nerve territories experiencing weakness and sensory loss. This can lead to a more complex clinical presentation.
Diagnostic Criteria and Awareness
The lack of standardized diagnostic criteria often leads to missed diagnoses and untreated patients.
-
There are no generally agreed-upon clinical diagnostic criteria for CIDP. This lack of standardization often delays diagnosis and treatment.
-
Early diagnosis and treatment are crucial. They prevent irreversible axonal loss and improve functional recovery.
-
There is a lack of awareness and treatment of CIDP. This contributes to the under-recognition and under-treatment of the condition.
Research and Economic Impact
Research and the economic impact of CIDP are important considerations for improving patient outcomes.
-
Stringent research criteria are applied to select patients for clinical trials. More robust diagnostic criteria and better awareness are needed.
-
CIDP has a significant economic impact. Prolonged morbidity and the need for long-term treatments contribute to healthcare costs.
-
Advancements in treatment options are ongoing. New immunomodulatory therapies and targeted treatments are being explored.
Quality of Life and Interdisciplinary Care
CIDP significantly affects the quality of life, requiring interdisciplinary care and patient education.
-
CIDP significantly affects the quality of life for patients. The progressive nature of the disease leads to significant disability and emotional distress.
-
Interdisciplinary care is essential for managing CIDP. This includes coordination among neurologists, physical therapists, and occupational therapists.
-
Patient education is critical in managing CIDP. Educating patients about their condition and treatment options helps them manage symptoms better.
-
Support groups can provide emotional support and practical advice. These groups help patients connect with others experiencing similar challenges.
Special Cases: HIV-CIDP, Pregnancy, and Vaccination
Certain conditions like HIV, pregnancy, and vaccination can influence the onset and progression of CIDP.
-
HIV-CIDP is a distinct form of CIDP. It occurs in individuals with HIV infection and is characterized by distinct patterns of demyelination and axonal loss.
-
Pregnancy can trigger or exacerbate CIDP symptoms. Hormonal changes and other factors associated with pregnancy may contribute to this risk.
-
In some cases, CIDP may be triggered by vaccinations. A study found that 32% of CIDP patients had a history of vaccination within 6 weeks of the onset of symptoms.
-
Non-specific upper respiratory tract or gastrointestinal infections can trigger CIDP. These infections often occur within 6 weeks of the onset of symptoms.
Diagnostic Tools and Treatment Monitoring
Various diagnostic tools and regular monitoring are essential for managing CIDP effectively.
-
Diagnostic tools for CIDP include electrodiagnostic studies, cerebrospinal fluid analysis, and imaging studies. These tools help confirm the diagnosis and assess nerve damage.
-
Regular monitoring of treatment efficacy is crucial. Follow-up appointments help adjust treatment plans and monitor for side effects.
-
Lifestyle modifications, such as regular exercise and physical therapy, can help improve functional recovery. These modifications should be tailored to the individual's specific needs and abilities.
Key Points on CIDP
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a rare, autoimmune disorder affecting the peripheral nervous system. It causes progressive weakness and sensory loss, typically starting in the legs. Early diagnosis and treatment are crucial to prevent irreversible damage. Treatment options include plasma exchange, intravenous immunoglobulin (IVIG), and corticosteroids. CIDP can present in various patterns, including ataxic, pure motor, and pure sensory. Fatigue, areflexia, and proximal limb weakness are common symptoms. The disease can be triggered by infections or vaccinations, and pregnancy may increase the risk of relapse. Effective management requires an interprofessional team approach, regular monitoring, and patient education. Support groups and psychological support can significantly improve the quality of life for those affected. Ongoing research aims to develop better diagnostic criteria and treatments, offering hope for improved outcomes in the future.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


