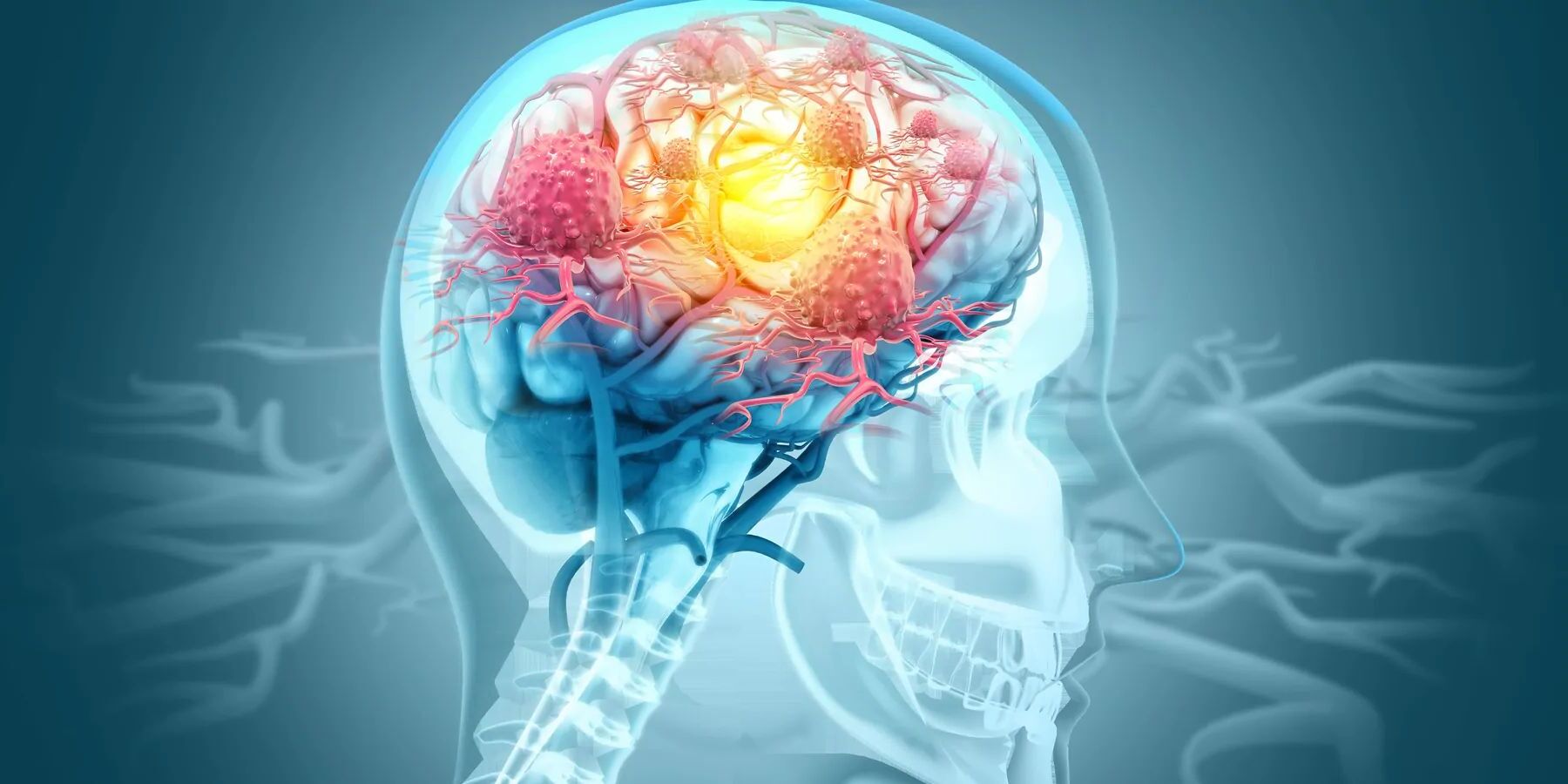
What exactly is a choroid plexus cyst? These small, fluid-filled sacs form in the brain's choroid plexus, a spongy tissue that produces cerebrospinal fluid. Found in about 1 out of every 50 to 100 pregnancies, these cysts are usually harmless and often disappear on their own. Detected during the second trimester via ultrasound, they can vary in size and shape. While their presence might raise concerns about genetic conditions like Trisomy 18, the actual risk remains low. Understanding choroid plexus cysts can help expectant parents and healthcare providers manage any potential concerns effectively. Let's dive into 50 key facts about these intriguing cysts.
Key Takeaways:
- Choroid plexus cysts are common, harmless fluid-filled sacs in a fetus's brain, usually resolving on their own. They raise a small concern for genetic conditions, but proper evaluation and surveillance are essential for reassurance.
- Most choroid plexus cysts are harmless and resolve on their own during pregnancy. While they may raise a small concern for genetic conditions, proper evaluation and surveillance ensure appropriate management and follow-up care.
What is a Choroid Plexus Cyst?
Choroid plexus cysts (CPCs) are small, fluid-filled sacs that can appear in a fetus's brain during pregnancy. They are generally harmless but can sometimes raise concerns. Let's dive into some key facts about these cysts.
-
Definition: A choroid plexus cyst is a fluid-filled sac in the choroid plexus, a part of the brain that produces cerebrospinal fluid (CSF).
-
Prevalence: CPCs are relatively common, appearing in about 1 out of every 50 to 100 pregnancies.
-
Location: These cysts can be found on one or both sides of the brain, usually near the lateral ventricles.
-
Size and Shape: CPCs vary in size and shape, ranging from a few millimeters to 1-2 cm in diameter.
-
Formation: They form when a small amount of CSF gets trapped in the choroid plexus as the brain develops.
How Are Choroid Plexus Cysts Detected?
Detection usually happens during routine prenatal check-ups. Here's how they are typically found.
-
Detection: CPCs are usually detected during the second trimester of pregnancy through ultrasound.
-
Ultrasound Appearance: On ultrasound, they appear as sonolucent cysts near the lateral ventricles, with echogenic walls due to the surrounding choroid plexus.
-
Risk of Aneuploidy: The presence of isolated CPCs raises a small concern for genetic conditions like Trisomy 18, but the risk is less than 1% if only a CPC is found.
-
Trisomy 18 Association: CPCs are weakly linked to Trisomy 18, but this association is not strong enough to significantly increase the risk.
-
Down Syndrome: CPCs do not increase the risk of Down syndrome.
What Happens After Detection?
Once detected, further steps are taken to ensure the health of the fetus.
-
Maternal Age: The risk of associated abnormalities with CPCs increases with maternal age, especially if maternal serum screening results are abnormal.
-
Prenatal Testing: Some pregnant individuals undergo prenatal testing early in pregnancy to evaluate the risk for Trisomy 18 and other chromosome conditions.
-
Genetic Counselor: Consulting a genetic counselor is advisable if CPCs are detected. They can review risk factors and help decide if prenatal testing is right for you.
-
Ultrasound Follow-Up: A more detailed ultrasound may be necessary to check for other concerns related to Trisomy 18 or other structural abnormalities.
-
Resolution: CPCs usually resolve on their own during pregnancy, typically by week 32.
Are Choroid Plexus Cysts Harmful?
Most CPCs are harmless, but understanding their nature is crucial.
-
Asymptomatic Incidence: Most fetuses with a CPC are normal, and the cysts are often asymptomatic incidental findings.
-
Incidence in Newborns: CPCs are present in less than 1 in 3,000 newborns.
-
Pathology: The cysts have no epithelial lining; they are spaces within the choroid plexus filled with clear fluid (CSF) and cellular debris.
-
Symptomatic CPCs: Symptomatic CPCs are rare and usually exceptionally large (2-8 cm). They can cause symptoms like headache and vomiting due to obstruction of CSF flow.
-
Treatment of Symptomatic CPCs: Symptomatic CPCs may require surgical intervention, such as endoscopic removal or excision through a craniotomy.
What Are the Complications?
While rare, complications can occur, especially with larger cysts.
-
Endoscopic Removal: Endoscopic techniques offer a minimally invasive option for treating symptomatic CPCs, often avoiding further treatment.
-
Complications: Large CPCs can cause obstructive hydrocephalus, a rare but serious condition where fluid accumulates in the brain, potentially leading to increased intracranial pressure.
-
Differential Diagnosis: CPCs should not be confused with other types of cysts, such as subacute in-utero intraventricular hemorrhage or choroid plexus xanthogranulomas.
-
Clinical Manifestations: Symptoms of large CPCs can include increased pressure, epilepsy, and intermittent worsening of symptoms due to a mobile cyst with a ball-and-chain configuration.
-
Asymmetrical Dilatation: Patients with unilateral lesions above the third ventricle can present with asymmetrical dilatation of the lateral ventricle.
How Are CPCs Managed?
Management involves careful monitoring and, in rare cases, surgical intervention.
-
Histological Examination: The histological examination of the cyst wall is consistent with choroid epithelium, confirming the nature of the cyst.
-
Postoperative Complications: Postoperative complications such as intraventricular hemorrhage and catheter infection can occur but are generally manageable with appropriate medical care.
-
Resolution in Infancy: Most CPCs spontaneously resolve by birth or early infancy, with very few reports of persistence into adulthood.
-
Incidental Findings: CPCs are often discovered incidentally in older patients, usually in the trigone of the lateral ventricle, and are typically small and asymptomatic.
-
Autopsy Series: CPCs are the most common neuroepithelial cysts, occurring in more than 50% of some autopsy series.
Are There Any Long-Term Effects?
Long-term effects are rare, but understanding potential outcomes is important.
-
Pediatric Prevalence: These cysts are more frequently found in children, with a preponderance for the male sex, and account for approximately 3% of all pediatric cerebral pathological entities.
-
Ventricular Cavity: CPCs can occur in any ventricular cavity and may be uni- or bilateral, single or multiple.
-
Trigone Congregation: In the lateral ventricle, they usually congregate at and around the trigone.
-
Prenatal Screening: The presence of CPC on prenatal screening has been associated with trisomy 18 and possibly trisomy 21, but most cysts are asymptomatic incidental findings.
-
Spontaneous Resolution: Most of these cysts spontaneously resolve by birth or early infancy, with very few reports of persistence into adulthood.
What Should Parents Know?
Parents should be informed and reassured about the nature of CPCs.
-
Obstruction of CSF Flow: Symptoms of large CPCs are secondary to the obstruction of CSF flow, particularly at the foramen of Monro.
-
Imaging Findings: Imaging of symptomatic patients usually reveals dilated ventricles. Patients with unilateral lesions above the third ventricle can present with asymmetrical dilatation of the lateral ventricle.
-
Clinical Manifestations: Other possible clinical manifestations of large cysts may range from increased pressure to epilepsy.
-
Diagnostic Evaluation: A detailed evaluation of detected cysts and other structural brain abnormalities is essential. Prenatal magnetic resonance scans can clearly decrease the need for risky procedures, such as an amniocentesis, in the evaluation of antenatal CPCs.
-
Risk of Aneuploidy: The size and number of cysts are thought to affect the risk of aneuploidy by some authors. However, the risk remains low if no other abnormalities are present.
What Are the Diagnostic Criteria?
Accurate diagnosis is crucial for proper management.
-
Ultrasound Criteria: Some studies suggest that the cysts should be at least 2.5 mm during the screening period of 13-21 weeks gestation and at least 2 mm from 22-38 weeks gestation for accurate diagnosis.
-
Avoiding Misdiagnosis: The size and number of cysts should be carefully evaluated to avoid confusing the surrounding choroid plexus heterogeneity as cysts.
-
Treatment Prognosis: Generally, CPCs are of no significance in most cases and typically resolve by the third trimester. However, if one is seen in antenatal imaging, careful surveillance of the rest of the fetus is warranted due to weak associations with karyotypic abnormalities.
-
Amniocentesis: Amniocentesis is suggested when there are other abnormalities or when there is a high risk for trisomy 18. The cysts themselves resolve in the third trimester and are generally not associated with abnormal CNS development.
What Are the Associated Conditions?
Understanding associated conditions helps in managing CPCs effectively.
-
Associated Conditions: It is usually the associated conditions that are of concern, not the cysts themselves. CPCs are of concern if the cysts are large (>1 cm), bilateral, multiple, and associated with structural abnormalities, especially in pregnancies with maternal age ≥32 years or abnormal maternal serum screening results.
-
Complications Overview: While rare, complications such as obstructive hydrocephalus can occur if the cyst is large. Other possible complications include postoperative intraventricular hemorrhage and catheter infection.
-
Differential Diagnosis Considerations: CPCs should not be confused with other types of cysts or conditions, such as subacute in-utero intraventricular hemorrhage or choroid plexus xanthogranulomas.
-
Clinical Management: The clinical management of CPCs involves careful surveillance and monitoring. If symptoms arise, further diagnostic evaluation and potential surgical intervention may be necessary.
-
Educational Importance: Understanding CPCs is crucial for both medical professionals and expectant parents. It helps alleviate anxiety and ensures appropriate management and follow-up care.
-
Conclusion: Choroid plexus cysts are common benign findings during pregnancy that typically resolve on their own. While they raise a small concern for genetic conditions like Trisomy 18, the risk remains low. Proper evaluation and surveillance are essential to ensure that any associated conditions are addressed promptly. With advancements in prenatal imaging and diagnostic techniques, the management of CPCs continues to improve, providing reassurance to expectant parents and healthcare providers alike.
Understanding Choroid Plexus Cysts
Choroid plexus cysts (CPCs) are common, benign findings during pregnancy. They usually resolve on their own by the third trimester. These fluid-filled structures in the brain's choroid plexus often cause no symptoms and are typically discovered during routine ultrasounds. While CPCs can be linked to genetic conditions like Trisomy 18, the risk remains low if no other abnormalities are present. Most fetuses with CPCs are perfectly healthy. If a CPC is detected, further evaluation and monitoring might be recommended to rule out any associated conditions. Consulting a genetic counselor can provide additional guidance. Advances in prenatal imaging have improved the management of CPCs, offering reassurance to expectant parents. Understanding these cysts helps alleviate anxiety and ensures appropriate care. So, while CPCs might sound alarming, they are usually just a small bump on the road to a healthy baby.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.