What is Basal Cell Carcinoma? Basal Cell Carcinoma (BCC) is the most common type of skin cancer, making up about 80% of all skin cancer cases. It starts in the basal cells, which are located in the epidermis, the skin's outermost layer. Why should you care? Because BCC is often caused by long-term exposure to ultraviolet (UV) radiation from the sun or tanning beds, understanding it can help you take steps to protect your skin. What are the symptoms? BCC can appear as open sores, red patches, shiny bumps, or scars. Early detection and treatment are crucial to prevent it from becoming disfiguring or, in rare cases, life-threatening. How can you prevent it? Using sunscreen, wearing protective clothing, and avoiding peak sun hours can significantly lower your risk.
What is Basal Cell Carcinoma?
Basal cell carcinoma (BCC) is the most common type of skin cancer. It starts in the basal cells, which are found in the deepest part of the epidermis. Here are some key facts to understand BCC better:
- Definition: BCC begins in the basal cells of the epidermis, the skin's outermost layer.
- Prevalence: It is the most common form of skin cancer, with around 3.6 million cases diagnosed annually in the U.S.
- Risk Factors: Main risk factors include UV radiation from the sun or tanning beds, fair skin, severe sunburns, and a family history of skin cancer.
- Causes: BCC occurs due to DNA damage in basal cells, often from prolonged UV exposure.
- Symptoms: BCCs can appear as open sores, red patches, pink growths, shiny bumps, scars, or growths with rolled edges and a central indentation. They may ooze, crust, itch, or bleed.
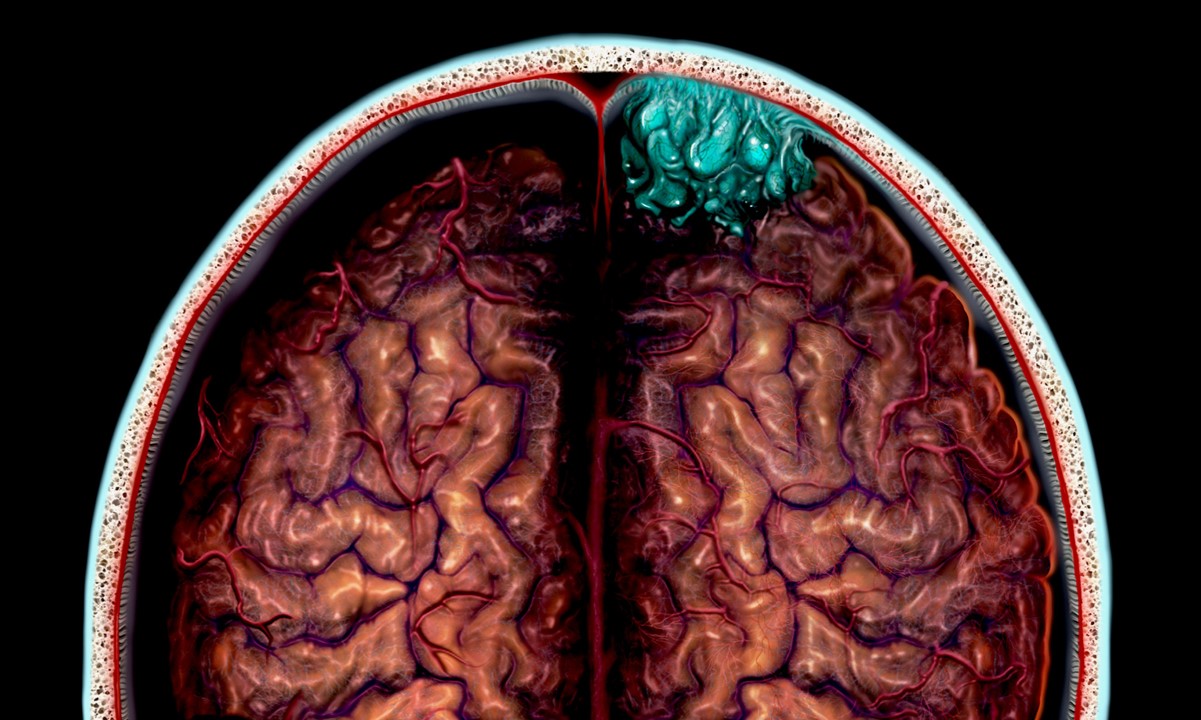
How Does Basal Cell Carcinoma Appear?
BCC can look different from person to person, making it tricky to identify without professional help. Here are some variations and warning signs:
- Appearance Variations: BCCs can resemble psoriasis or eczema, complicating early detection.
- Warning Signs: A key warning sign is a spot that doesn’t heal on its own. If a lesion persists for more than a month, see a dermatologist.
Treatment Options for Basal Cell Carcinoma
Early treatment is crucial for curing BCC. Various treatment methods are available, depending on the size, location, and depth of the tumor:
- Treatment: Most BCCs are curable with early treatment. Common treatments include surgical procedures and topical treatments.
- Surgical Excision: This involves removing the lesion along with a margin of healthy skin to ensure all cancerous cells are eliminated.
- Mohs Surgery: A specialized technique that removes the tumor layer by layer, examining each under a microscope until no cancer cells remain. It’s useful for tumors in sensitive areas.
- Topical Treatments: Imiquimod cream stimulates the immune system to fight BCC. It’s often used for superficial BCCs and can be applied at home.
- Radiation Therapy: Used in cases where surgery isn’t feasible or would cause significant disfigurement.
Risks and Complications of Basal Cell Carcinoma
While BCC rarely spreads, untreated cases can lead to severe complications. Here’s what you need to know:
- Risk of Metastasis: BCC rarely metastasizes but can grow and become dangerous if untreated.
- Local Invasion: Untreated BCCs can grow wide and deep, destroying surrounding tissues and potentially leading to disfigurement.
- Recurrence: Improperly treated BCCs can recur, sometimes repeatedly.
- Aggressive Cases: Rarely, BCC can spread to other parts of the body.
- Life-Threatening Cases: In very rare instances, untreated BCC can become life-threatening by spreading to distant organs.
Preventing Basal Cell Carcinoma
Prevention is the best way to lower your risk of developing BCC. Here are some effective strategies:
- Prevention: Shield your skin from UV radiation by using sunscreen, wearing protective clothing, and avoiding tanning salons.
- Sunscreen Use: Apply sunscreen with an SPF of at least 30 and reapply every two hours.
- Protective Clothing: Wear dark, tightly woven clothing that covers arms and legs, along with a broad-brimmed hat.
- Sunglasses: Choose sunglasses that block both UVA and UVB rays.
- Regular Skin Checks: Examine your skin often for new growths or changes in existing moles, freckles, bumps, and birthmarks.
Who is at Risk for Basal Cell Carcinoma?
Certain individuals are more prone to developing BCC due to genetic conditions, skin type, or other factors:
- Early Detection: Early detection is key. If you notice any new or changing skin lesions, see a dermatologist immediately.
- Genetic Conditions: Conditions like Gorlin syndrome can increase the risk of developing multiple BCCs.
- Photosensitivity: Conditions that increase photosensitivity can contribute to BCC development.
- Immunosuppression: People with weakened immune systems are at higher risk.
- Actinic Keratosis: This precancerous condition caused by UV exposure can increase the risk of BCC.
- Xeroderma Pigmentosum: This rare inherited condition makes individuals extremely sensitive to UV light, increasing their risk of multiple skin cancers.
- Fair Skin: People with fair skin are at higher risk due to their reduced ability to protect against UV radiation.
- Blond or Redhead: Blond or redheaded individuals are also at higher risk.
- Freckles and Sunburns: Fair skin that easily freckles or sunburns increases the risk.
- Light-Colored Eyes: People with light-colored eyes (blue or green) are at higher risk.
- Family History: A family history of skin cancer can increase an individual's risk.
- Previous Skin Cancer: Individuals previously diagnosed with skin cancer are at higher risk.
- Previous Radiation Therapy: Those who have undergone radiation therapy are at higher risk.
- Gorlin Syndrome: This rare genetic disorder can cause hundreds of BCCs over a lifetime.
- Xeroderma Pigmentosum: Mutations in DNA repair genes make individuals extremely sensitive to UV light, increasing their risk.
Understanding the Progression and Staging of Basal Cell Carcinoma
BCC is primarily staged based on its local invasion. Here’s how it progresses and how it’s staged:
- Cumulative Damage: UV damage builds up over years, starting in childhood.
- Local Tissue Invasion: Untreated BCCs can invade local tissues and bones, leading to significant damage.
- Stages of Skin Cancer: Stages are defined by the structures involved: T-stage (tumor depth), N-stage (lymph nodes), and M-stage (distant organs).
- BCC Staging: BCC is less likely to spread to lymph nodes and distant organs.
- Tumor Depth: The depth of tumor invasion is critical in staging BCC.
- Lymph Node Involvement: BCC rarely involves lymph nodes, but when it does, it’s a sign of advanced disease.
- Distant Metastasis: BCC very rarely metastasizes to distant organs.
Treatment Outcomes and Patient Education
Most BCCs are curable with early treatment. Here’s what you need to know about treatment outcomes and the importance of patient education:
- Treatment Outcomes: Most BCCs are curable with early treatment. Success depends on the size, location, and depth of the tumor.
- Recurrence Rates: If not treated properly, BCCs can recur. Recurrence rates vary depending on the initial treatment.
- Aggressive Cases Management: Aggressive cases may require more extensive treatment, including radiation therapy.
- Cosmetic Considerations: In sensitive areas, treatments like Mohs surgery are preferred to minimize scarring.
- Patient Education: Educating patients about BCC risks and symptoms is crucial for early detection and prevention.
- Research and Development: Ongoing research into the genetic and molecular mechanisms of BCC can lead to better diagnostic tools and treatments. Understanding the Hedgehog signaling pathway has led to new therapies.
Key Points to Remember
Basal cell carcinoma (BCC) stands as the most common skin cancer, with millions of cases each year. It often results from prolonged UV exposure, making sun protection crucial. BCCs can appear as shiny bumps, red patches, or scars, and they might itch, bleed, or ooze. Early detection is vital since untreated BCCs can invade local tissues and cause significant damage. Treatments range from surgical excision and Mohs surgery to topical creams and radiation therapy. Fair-skinned individuals, those with a history of severe sunburns, or a family history of skin cancer are at higher risk. Regular skin checks and protective measures like sunscreen and clothing can help prevent BCC. Though BCC rarely metastasizes, it can become life-threatening if ignored. Stay vigilant, protect your skin, and consult a dermatologist for any persistent or unusual skin changes.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.