What is Orbital Apex Syndrome? Orbital Apex Syndrome (OAS), also known as Jacod syndrome, is a complex neurological disorder that affects the area where the eye socket meets the brain. This condition involves multiple cranial nerves, leading to symptoms like ophthalmoplegia (eye muscle weakness), proptosis (bulging eye), ptosis (drooping eyelid), and visual loss. Various causes, including tumors, infections, inflammation, trauma, and vascular issues, can trigger OAS. Diagnosing and managing OAS requires a team of specialists, including ophthalmologists, neurologists, and radiologists. Early recognition and prompt treatment are crucial for improving outcomes and preventing permanent damage.
Key Takeaways:
- Orbital Apex Syndrome (OAS) is a complex neurological disorder affecting the orbital apex, causing symptoms like eye muscle paralysis and visual loss. It can be caused by tumors, infections, inflammation, trauma, or vascular anomalies.
- Early recognition and a multidisciplinary approach involving ophthalmologists, neurologists, and radiologists are crucial for diagnosing and managing Orbital Apex Syndrome effectively. Timely treatment tailored to individual patient needs can significantly impact outcomes.
What is Orbital Apex Syndrome?
Orbital Apex Syndrome (OAS), also known as Jacod syndrome, is a complex neurological disorder. It involves multiple cranial nerves and affects the orbital apex, a critical area connecting the orbit and cranial cavity.
-
Definition and Classification: OAS is one of three main disorders affecting the orbital apex, alongside superior orbital fissure syndrome and cavernous sinus syndrome.
-
Clinical Features: Symptoms include ophthalmoplegia (eye muscle paralysis), proptosis (bulging eye), ptosis (drooping eyelid), hypoesthesia (reduced sensation), and visual loss.
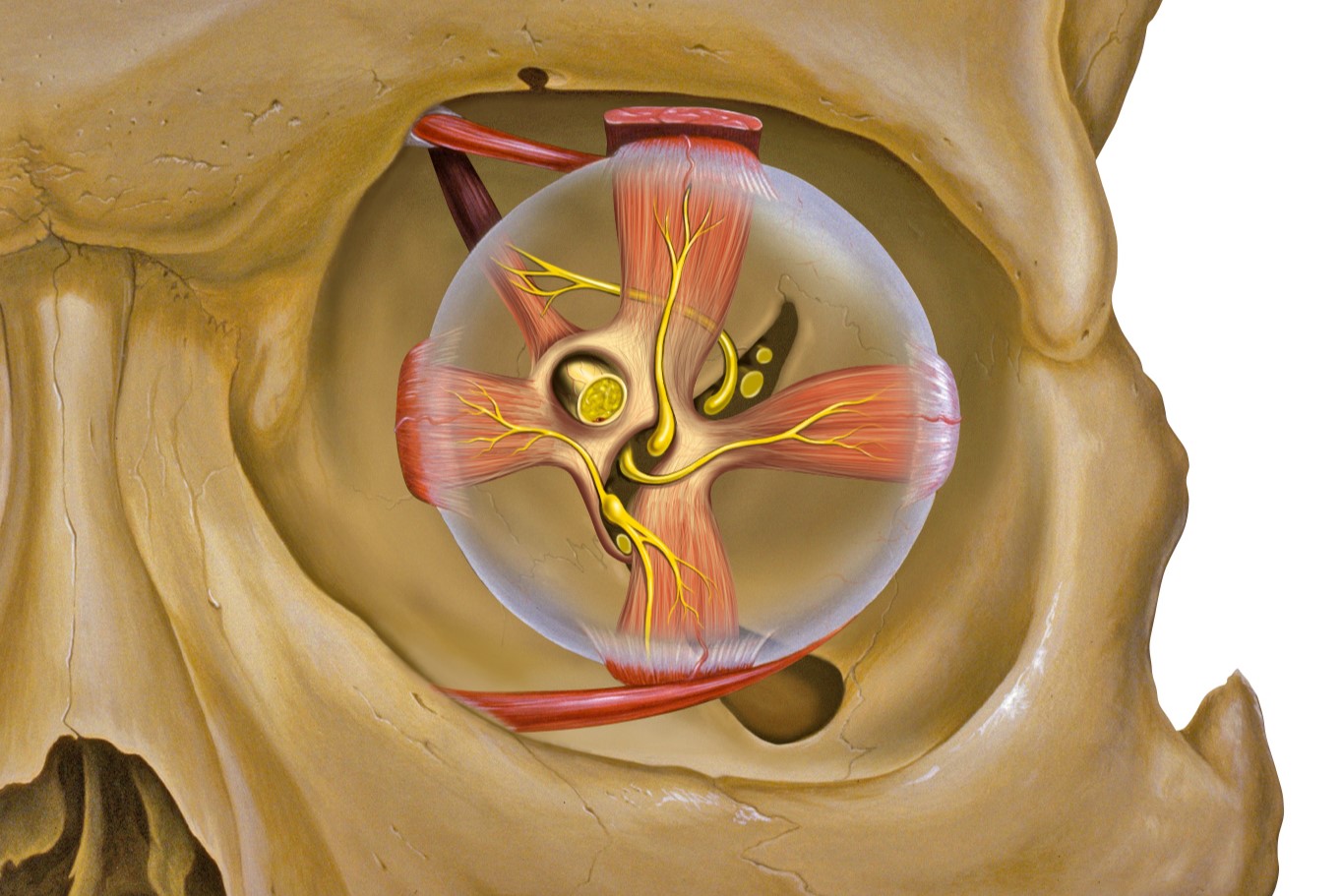
Anatomy of the Orbital Apex
Understanding the anatomy of the orbital apex helps in diagnosing and treating OAS effectively.
-
Orbital Apex Structure: The orbital apex connects the orbit and cranial cavity, housing the optic nerve, ophthalmic artery, and cranial nerves III, IV, and VI.
-
Bony Components: The roof is formed by the lesser wing of the sphenoid, the lateral wall by the greater wing of the sphenoid, the medial wall by the ethmoidal sinus, and the floor by the orbital plate of the palatine bone.
-
Optic Canal: Contains the optic nerve, ophthalmic artery, and postganglionic sympathetic fibers from the carotid plexus.
Causes of Orbital Apex Syndrome
Various factors can lead to the development of OAS, ranging from infections to trauma.
-
Neoplastic Causes: Tumors in the head and neck, hematologic cancers, and metastases can spread to the orbital apex.
-
Infectious Causes: Bacterial or fungal sinusitis can extend to the orbital apex, causing OAS.
-
Inflammatory Causes: Conditions like Tolosa-Hunt syndrome involve inflammation that can affect the orbital apex.
-
Traumatic Causes: Cranio-maxillo-facial fractures can damage structures within the orbital apex.
-
Vascular Causes: Carotid-cavernous fistula, a vascular anomaly, can cause pulsatile proptosis and other OAS symptoms.
Diagnosing Orbital Apex Syndrome
A multidisciplinary approach is crucial for accurate diagnosis.
-
Clinical Examination: Assess symptoms like ophthalmoplegia, proptosis, and visual loss.
-
Imaging Studies: MRI and CT scans visualize the orbital apex and its contents.
-
Electrophysiological Tests: Visual evoked potentials (VEPs) and electro-oculography (EOG) assess optic nerve and muscle function.
Managing Orbital Apex Syndrome
Treatment varies based on the underlying cause.
-
Surgical Intervention: Necessary for tumor removal or vascular anomaly repair.
-
Medical Therapy: Antibiotics or antifungal medications treat infectious causes.
-
Steroid Therapy: Reduces inflammation in inflammatory causes.
-
Radiation Therapy: Used for treating neoplastic causes.
-
Pain Management: Crucial for inflammatory or vascular causes.
Risk Factors for Orbital Apex Syndrome
Certain conditions and histories increase the risk of developing OAS.
-
Immunocompromise: Individuals with weakened immune systems are more susceptible to infections.
-
History of Malignancy: Increases the risk of neoplastic causes.
-
History of Sinusitis: Recurrent or untreated sinusitis can lead to infections spreading to the orbital apex.
-
Trauma: Cranio-maxillo-facial trauma can damage orbital apex structures.
Clinical Signs of Orbital Apex Syndrome
Recognizing the clinical signs is essential for early diagnosis.
-
Proptosis: Bulging of the eyeball.
-
Ophthalmoplegia: Weakness or paralysis of the eye muscles.
-
Ptosis: Drooping of the eyelid.
-
Hypoesthesia: Reduced sensation in the forehead and upper eyelid.
-
Visual Loss: Reduced or complete loss of vision.
-
Relative Afferent Pupillary Defect (RAPD): Indicates optic nerve involvement.
-
Optic Disc Edema or Pallor: Changes in the optic disc indicating optic nerve pathology.
-
Pulsatile Proptosis: Bulging of the eyeball with a pulsatile nature indicating vascular anomalies.
Differential Diagnosis
Differentiating OAS from other conditions is crucial for appropriate treatment.
-
Superior Orbital Fissure Syndrome (SOFS): Similar to OAS but without optic nerve impairment.
-
Cavernous Sinus Syndrome (CSS): Includes hypoesthesia of the cheek and lower eyelid along with OAS features.
Treatment Outcomes and Prognosis
The effectiveness of treatment and prognosis depends on various factors.
-
Early Recognition: Critical for improving treatment outcomes.
-
Treatment Outcomes: Depend on the underlying cause and promptness of treatment.
-
Prognosis: Varies widely; prompt and appropriate management can improve outcomes.
Multidisciplinary Approach
A collaborative effort ensures comprehensive evaluation and management.
-
Ophthalmologists: Essential for eye-related symptoms and treatments.
-
Neurologists: Address neurological aspects of OAS.
-
Radiologists: Provide detailed imaging for accurate diagnosis.
-
Other Specialists: May include infectious disease experts, oncologists, and surgeons.
Role of Imaging and Electrophysiological Tests
These tools are vital for diagnosing and managing OAS.
-
MRI and CT Scans: Provide detailed visualization of the orbital apex.
-
Visual Evoked Potentials (VEPs): Assess optic nerve function.
-
Electro-oculography (EOG): Evaluates extraocular muscle function.
Importance of Early Recognition and Treatment
Timely diagnosis and management can significantly impact outcomes.
-
Early Diagnosis: Reduces associated comorbidities and improves visual outcomes.
-
Prompt Treatment: Essential for preventing permanent damage.
-
Comprehensive Management: Tailored to individual patient needs for the best outcomes.
Final Thoughts on Orbital Apex Syndrome
Orbital Apex Syndrome (OAS) is a complex condition involving multiple cranial nerves. It presents with symptoms like ophthalmoplegia, proptosis, ptosis, hypoesthesia, and visual loss. The orbital apex is a critical area connecting the orbit and cranial cavity, housing vital structures such as the optic nerve and ophthalmic artery. Causes range from neoplastic and infectious to inflammatory and traumatic origins. Diagnosis involves clinical exams, imaging studies, and electrophysiological tests. Treatment varies based on the underlying cause, including surgical intervention, medical therapy, steroids, and radiation. Early recognition and a multidisciplinary approach are crucial for better outcomes. Understanding the risk factors and clinical signs can aid in prompt diagnosis and effective management, ultimately improving patient prognosis.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


