What is HELLP syndrome? HELLP syndrome is a serious condition affecting pregnant women, marked by hemolysis (breakdown of red blood cells), elevated liver enzymes, and low platelet count. This condition can be life-threatening for both mother and baby. Symptoms often mimic other illnesses, making early detection crucial. HELLP syndrome usually appears in the third trimester but can occur anytime from 20 weeks of pregnancy to a week after delivery. Understanding the risk factors, symptoms, and treatment options can help manage this condition effectively. Regular prenatal care and collaboration among healthcare specialists are essential for improving outcomes.
What is HELLP Syndrome?
HELLP syndrome is a serious condition that affects pregnant women. It stands for hemolysis, elevated liver enzymes, and low platelet count. This syndrome can be life-threatening if not managed properly. Let's dive into some crucial facts about HELLP syndrome.
- Definition: HELLP syndrome involves the breakdown of red blood cells, elevated liver enzymes, and a low platelet count.
- Incidence: It is relatively rare, occurring in 0.1% to 0.6% of all pregnancies.
- Symptoms: Common symptoms include pain in the upper belly, blurred vision, fatigue, and swelling. These symptoms can sometimes be mistaken for other conditions like gastritis or flu.
- Diagnostic Criteria: Diagnosis is based on lab tests showing hemolysis, elevated liver enzymes, and low platelet count. A microangiopathic blood smear often indicates small vessel damage.
Risk Factors and Genetic Associations
Understanding the risk factors and genetic predispositions can help in early detection and management.
- Risk Factors: Multiparity and advanced maternal age increase the risk of developing HELLP syndrome.
- Genetic Association: There is a genetic predisposition to HELLP syndrome, though the exact genetic markers are not fully understood.
- Preeclampsia Connection: HELLP syndrome often occurs with preeclampsia but can also occur independently. About 1 in 5 cases of HELLP syndrome occur without elevated blood pressure or protein in the urine.
- Etiology: The exact cause is unknown, but it likely involves endothelial dysfunction and abnormal placental development.
Clinical Presentation and Complications
Knowing how HELLP syndrome presents and its potential complications is crucial for timely intervention.
- Clinical Presentation: Symptoms typically appear in the third trimester but can occur anytime from 20 weeks onwards. It can also develop in the seven days after childbirth.
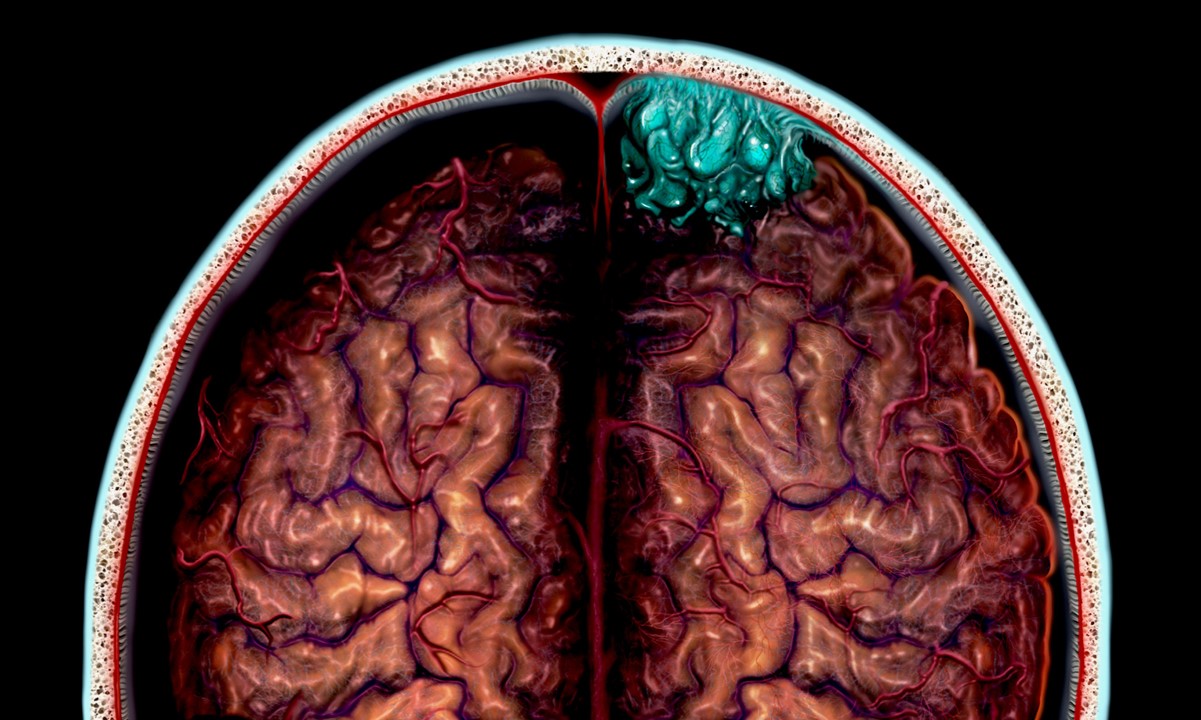
- Complications: Maternal complications include eclampsia, abruptio placentae, disseminated intravascular coagulation (DIC), acute renal failure, severe ascites, cerebral edema, pulmonary edema, wound hematoma/infection, subcapsular liver hematoma, liver rupture/hematoma, fulminant liver failure, cerebral infarction, cerebral hemorrhage, and cardiovascular instability.
- Fetal Complications: Fetal complications include perinatal death, intrauterine growth restriction (IUGR), preterm birth, neonatal thrombocytopenia, leukopenia, neutropenia, and respiratory distress syndrome (RDS).
- Maternal Mortality: The maternal mortality rate is significant, with about 1% to 25% of cases resulting in maternal death.
- Fetal Mortality: The fetal mortality rate is also high, with perinatal death occurring in 7.4% to 34% of cases.
Early Detection and Treatment
Early detection and appropriate treatment can significantly improve outcomes for both mother and baby.
- Early Detection: Early detection is critical for managing HELLP syndrome effectively. Regular prenatal care and lab testing are essential for identifying the condition early.
- Treatment: The primary treatment is delivery, which can be vaginal or cesarean, depending on the clinical situation. Corticosteroids may be administered to promote fetal lung maturity if delivery is imminent.
- Corticosteroids: Corticosteroids like dexamethasone can help reduce the severity of the condition by promoting fetal lung maturity and reducing inflammation.
- Monitoring: Close monitoring of both the mother and the fetus is necessary to manage the condition effectively. This includes regular blood tests, ultrasound scans, and fetal monitoring.
Risk of Recurrence and Prevention
Understanding the risk of recurrence and preventive measures can help manage future pregnancies.
- Risk of Recurrence: Women who have had HELLP syndrome are at a higher risk of developing it again in subsequent pregnancies. Up to 1 in 5 women who have had HELLP syndrome experience it a second time.
- Prevention: Maintaining a healthy lifestyle, preventing diseases such as hypertension and diabetes, and regular exercise can help reduce the risk of developing HELLP syndrome in subsequent pregnancies.
- Patient Education: Educating patients about the risks and complications associated with HELLP syndrome is crucial. Patients should be informed about the importance of regular prenatal care and early detection.
Collaboration Among Specialists
Managing HELLP syndrome often requires a team of specialists to address the various complications that may arise.
- Collaboration Among Specialists: Collaboration among different specialties such as maternal-fetal medicine, pediatrics/neonatology, anesthesiology, surgery, nephrology, hematology, and ophthalmology is essential for managing HELLP syndrome effectively.
- Intensive Care: Patients with severe cases may require intensive care unit (ICU) admission for close monitoring and management of complications.
- Anesthesiology Consultation: Anesthesiology consultation is often required for managing pain and ensuring safe delivery, especially if a cesarean section is necessary.
- Pediatrics/Neonatology Consultation: Neonatal care is critical for managing complications in newborns, including respiratory distress syndrome and thrombocytopenia.
- Maternal-Fetal Medicine Consultation: Maternal-fetal medicine specialists play a crucial role in managing the condition, including monitoring fetal well-being and planning delivery.
- Hepatology Consultation: Hepatology consultation may be required for managing liver-related complications such as liver rupture or fulminant liver failure.
- Surgery Consultation: Surgical intervention may be necessary for managing severe complications such as liver rupture or wound hematoma.
- Nephrology Consultation: Nephrology consultation may be required for managing renal complications such as acute renal failure.
- Hematology Consultation: Hematology consultation is essential for managing blood-related complications such as thrombocytopenia and DIC.
- Ophthalmology Consultation: Ophthalmology consultation may be required for managing visual disturbances such as blurred vision.
Risk Factors for Preeclampsia and Eclampsia
Preeclampsia and eclampsia are significant risk factors for developing HELLP syndrome.
- Risk Factors for Preeclampsia: Preeclampsia is a significant risk factor for developing HELLP syndrome. Women with preeclampsia are at a higher risk of developing HELLP syndrome.
- Risk Factors for Eclampsia: Eclampsia, which is characterized by seizures during pregnancy or postpartum, is another significant risk factor for developing HELLP syndrome.
- Symptoms of Preeclampsia: Symptoms of preeclampsia include high blood pressure, proteinuria, and visual disturbances. These symptoms can sometimes be mistaken for other conditions.
- Symptoms of Eclampsia: Symptoms of eclampsia include seizures, which can be life-threatening if not managed promptly. Eclampsia is a severe complication of preeclampsia.
HELLP Syndrome vs. Preeclampsia and Eclampsia
Understanding the differences between HELLP syndrome, preeclampsia, and eclampsia is crucial for proper diagnosis and treatment.
- HELLP Syndrome vs. Preeclampsia: While HELLP syndrome is often considered a variant of preeclampsia, recent evidence suggests they may be separate disorders. About 15 to 20% of patients with HELLP syndrome do not have preceding hypertension or proteinuria.
- HELLP Syndrome vs. Eclampsia: HELLP syndrome and eclampsia are distinct conditions. Eclampsia involves seizures, whereas HELLP syndrome involves hemolysis, elevated liver enzymes, and low platelet count.
HELLP Syndrome in Special Populations
Certain populations may have an increased risk of developing HELLP syndrome.
- HELLP Syndrome in COVID-19: Patients with SARS-CoV-2 infection during pregnancy have an increased risk for preeclampsia and HELLP syndrome.
- HELLP Syndrome in Multiparity: Multiparity increases the risk of developing HELLP syndrome. Women who have had multiple pregnancies are at a higher risk of developing this condition.
- HELLP Syndrome in Advanced Maternal Age: Advanced maternal age also increases the risk of developing HELLP syndrome. Women over 35 years old are at a higher risk of developing this condition.
- HELLP Syndrome and Genetic Predisposition: There is a genetic predisposition to HELLP syndrome. Women with a family history of preeclampsia or HELLP syndrome are at a higher risk of developing this condition.
Lifestyle Factors and Prenatal Care
Maintaining a healthy lifestyle and regular prenatal care can help reduce the risk of developing HELLP syndrome.
- HELLP Syndrome and Lifestyle Factors: Maintaining a healthy lifestyle, including regular exercise and avoiding diseases such as hypertension and diabetes, can help reduce the risk of developing HELLP syndrome in subsequent pregnancies.
- HELLP Syndrome and Prenatal Care: Regular prenatal care is essential for early detection of HELLP syndrome. Women should attend all scheduled prenatal appointments to monitor their health and the health of their fetus.
- HELLP Syndrome and Delivery: Early delivery is often necessary to manage HELLP syndrome effectively. The timing of delivery depends on the severity of the condition and the well-being of the fetus.
- HELLP Syndrome and Neonatal Care: Neonatal care is critical for managing complications in newborns, including respiratory distress syndrome and thrombocytopenia. Newborns with HELLP syndrome may require close monitoring and treatment in a neonatal intensive care unit (NICU).
- HELLP Syndrome and Patient Education: Educating patients about the risks and complications associated with HELLP syndrome is crucial. Patients should be informed about the importance of regular prenatal care, early detection, and the potential need for early delivery.
Understanding HELLP Syndrome
HELLP syndrome is a serious condition that can affect pregnant women, characterized by hemolysis, elevated liver enzymes, and low platelet count. Though rare, it poses significant risks to both mother and baby. Early detection through regular prenatal care is crucial. Symptoms like upper belly pain, blurred vision, and fatigue should never be ignored. Treatment often involves early delivery, and close monitoring is essential. Women with a history of HELLP syndrome should be particularly vigilant in subsequent pregnancies. Collaboration among various medical specialists ensures comprehensive care. Educating patients about the risks and importance of prenatal care can make a big difference. Understanding the condition, its symptoms, and treatment options can help manage HELLP syndrome effectively, improving outcomes for both mother and child. Stay informed, stay vigilant, and prioritize health during pregnancy.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.