Hepatorenal Syndrome (HRS) is a severe condition affecting kidney function in people with advanced liver disease. It involves a dramatic reduction in blood flow to the kidneys, leading to acute kidney injury. What makes HRS particularly alarming? The kidneys themselves aren't damaged; instead, the issue lies in the blood flow. This syndrome is split into two types: Type 1, which progresses rapidly, and Type 2, which is slower but still serious. Symptoms often include jaundice, reduced urine output, and swelling. Understanding HRS is crucial for early detection and treatment, potentially saving lives. Let's dive into 40 essential facts about this life-threatening condition.
Understanding Hepatorenal Syndrome
Hepatorenal Syndrome (HRS) is a severe condition affecting kidney function in those with advanced liver disease. It involves complex interactions between the liver and kidneys, leading to acute kidney injury. Let's explore some key facts about this condition.
-
Definition and Overview: HRS is a functional kidney impairment seen in advanced liver disease. The kidneys themselves aren't damaged; they would work fine if transplanted into a healthy person.
-
Etiology: The exact cause remains unknown. However, it's believed to result from factors like portal hypertension and systemic circulatory disturbances.
-
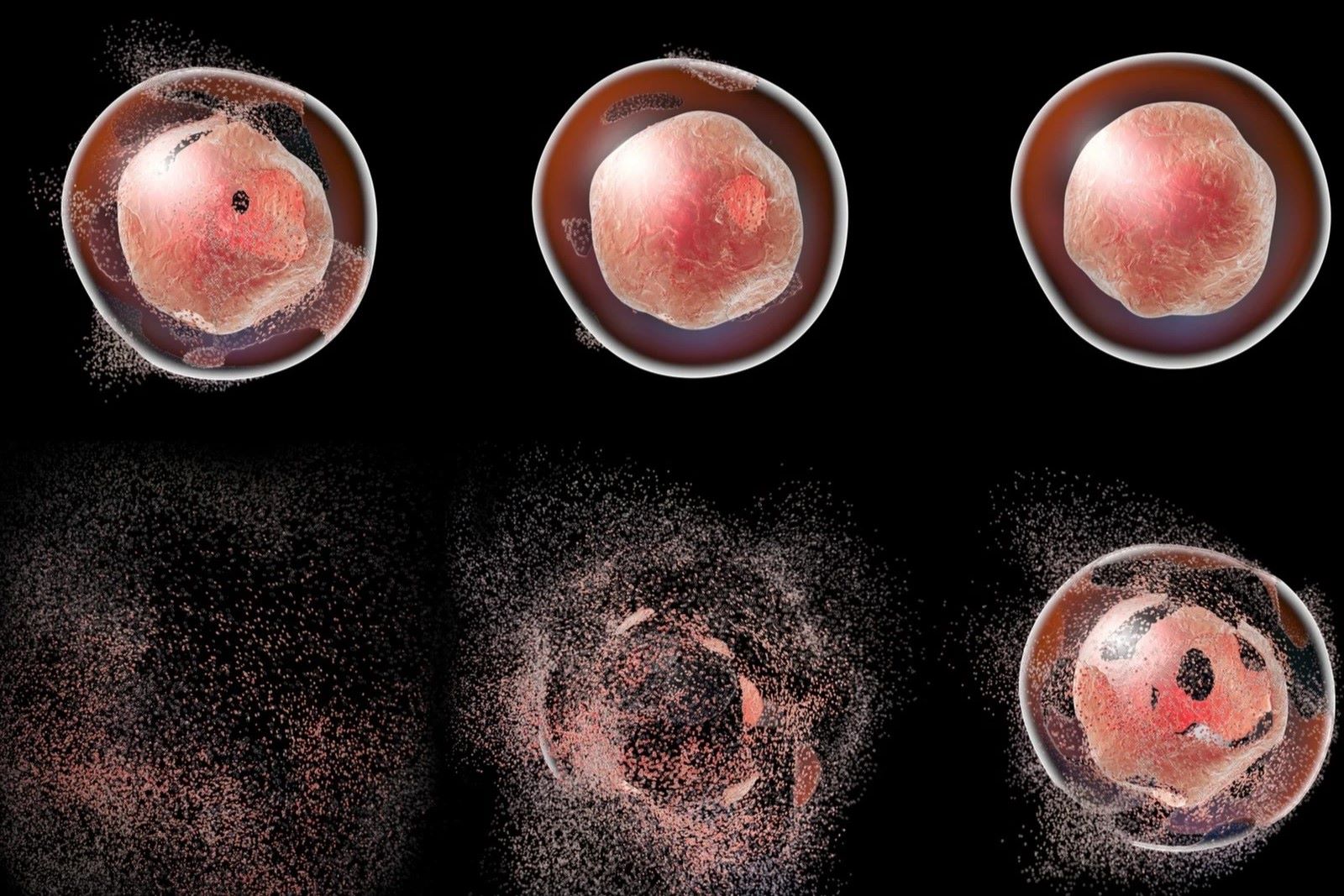
Pathophysiology: HRS involves severe renal vasoconstriction, reducing blood flow to the kidneys. This leads to a decreased glomerular filtration rate (GFR) and increased serum creatinine levels.
Types of Hepatorenal Syndrome
HRS is classified into two main types based on the severity and progression of renal impairment.
-
Type 1 HRS: This rapidly progressive form doubles the initial serum creatinine level to over 221 μmol/L within two weeks. The median survival time is less than two weeks.
-
Type 2 HRS: This subtler form progresses more slowly. The main clinical consequence is diuretic-resistant ascites, with a median survival time of about six months.
Clinical Manifestations
Patients with HRS often present with signs and symptoms of advanced liver disease.
-
Jaundice: Yellowing of the skin and eyes due to high bilirubin levels.
-
Finger Clubbing: Swelling of the fingers and toes.
-
Palmar Erythema: Reddening of the palms.
-
Spider Naevi: Small, spider-like blood vessels visible on the skin.
-
Splenomegaly: Enlarged spleen.
-
Bleeding Tendency: Increased risk of bleeding due to impaired liver function.
-
Hepatic Encephalopathy: Cognitive impairment due to liver dysfunction.
-
Oedema: Swelling due to fluid retention.
-
Ascites: Accumulation of fluid in the abdomen.
-
Reduced Urine Output: Particularly in Type 1 HRS, urine output is drastically reduced.
Diagnostic Criteria
The International Ascites Club has set specific criteria for diagnosing HRS.
-
Chronic or Acute Liver Disease: Advanced hepatic failure and portal hypertension.
-
Low GFR: Serum creatinine >133 μmol/L or 24-hour creatinine clearance <40 mL/min.
-
Absence of Shock: No ongoing bacterial infection or treatment with nephrotoxic drugs.
-
Absence of Gastrointestinal or Renal Fluid Losses: No sustained improvement in renal function following diuretic withdrawal and plasma volume expansion with 1.5 L of isotonic saline.
-
Proteinuria <0.5 g/d: No ultrasonographic evidence of obstructive uropathy or parenchymal renal disease.
-
Additional Criteria: Urine volume <0.5 L/d, urine sodium <10 mmol/L, urine osmolality > plasma osmolality, urine red blood cells <50 high power field, serum sodium concentration <130 mmol/L.
Epidemiology and Risk Factors
Understanding who is at risk can help in early detection and management.
-
Epidemiology: HRS occurs in about 4% of patients admitted with decompensated cirrhosis. The cumulative probability of developing HRS is 18% at one year and 39% at five years.
-
Spontaneous Bacterial Peritonitis (SBP): An infection of the membrane lining the abdominal cavity increases the risk.
-
Diuretic Use: High doses of diuretics can worsen renal vasoconstriction.
-
Refractory Ascites: Lack of response to high doses of diuretics (400 mg of spironolactone per day plus 160 mg of furosemide per day) is a risk factor.
Symptoms and Diagnosis
Recognizing symptoms and diagnosing HRS early can improve outcomes.
-
Symptoms: Nonspecific symptoms related to advanced liver disease, including jaundice, fatigue, and abdominal swelling. Reduced urine output is critical, especially in Type 1 HRS.
-
Diagnosis: No specific test exists for HRS-AKI. However, serum creatinine levels are a key indicator of kidney function.
-
Monitoring: Regular monitoring of serum creatinine levels is crucial for early detection. Patients with cirrhosis and ascites should have frequent blood creatinine checks, especially if on diuretics.
Treatment Options
Treating HRS involves both medical and surgical interventions.
-
Vasoconstrictor Therapy: Using vasoconstrictors like terlipressin can improve short-term outcomes by reducing renal vasoconstriction.
-
Albumin Infusion: Administering albumin helps expand plasma volume and improve renal function.
-
Liver Transplantation: Often the definitive treatment, liver transplantation can restore normal liver function and improve kidney function.
Medical and Surgical Management
Different approaches are used to manage HRS effectively.
-
Terlipressin: A synthetic analogue of vasopressin that reduces renal vasoconstriction.
-
Midodrine: An alpha-adrenergic agonist that helps increase blood pressure and reduce renal vasoconstriction.
-
Albumin: Administering albumin helps expand plasma volume and improve renal function.
-
Surgical Interventions: Liver transplantation is the definitive treatment, restoring normal liver function and improving kidney function.
Prognosis and Prevention
Understanding the prognosis and ways to prevent HRS can help manage the condition better.
-
Prognosis: The prognosis for HRS is poor, especially for Type 1 HRS. The median survival time for Type 1 HRS is less than two weeks, with nearly all patients dying within 8-10 weeks after renal failure onset. Type 2 HRS has a longer median survival time of about six months.
-
Prevention: Managing cirrhosis and its complications can help prevent HRS. Administering albumin to patients with spontaneous bacterial peritonitis can prevent the circulatory disturbances leading to HRS.
Complications and Interprofessional Team
Complications of HRS and the importance of a coordinated healthcare team.
-
Complications: Acute kidney injury, diuretic resistance, and hepatic encephalopathy are common complications.
-
Interprofessional Team: Improving care coordination among the interprofessional team, including hepatologists and nephrologists, is crucial for enhancing care delivery and outcomes.
Research and Future Directions
Ongoing research and future directions in HRS management.
- Research Developments: Recent research has provided new treatment modalities with improved prognosis. Vasoconstrictor therapy and albumin infusion have improved short-term outcomes and survival chances for HRS patients.
Final Thoughts on Hepatorenal Syndrome
Hepatorenal syndrome (HRS) is a severe condition affecting kidney function in those with advanced liver disease. It involves complex changes in blood flow, leading to kidney impairment. There are two types: Type 1, which progresses rapidly, and Type 2, which is slower but still serious. Symptoms include jaundice, reduced urine output, and ascites. Diagnosis relies on specific criteria, including serum creatinine levels and absence of shock or infection.
Treatment options include vasoconstrictor therapy, albumin infusion, and liver transplantation. Despite these interventions, the prognosis remains poor, especially for Type 1 HRS. Preventive measures focus on managing cirrhosis and its complications. Public awareness and early detection are crucial for improving outcomes. Future research aims to better understand the condition and develop more effective treatments. Understanding HRS is essential for those affected and their caregivers.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.