What is autonomic dysfunction? Autonomic dysfunction, or dysautonomia, is a condition where the autonomic nervous system (ANS) doesn't work properly. The ANS controls involuntary functions like heart rate, blood pressure, digestion, and body temperature. When it malfunctions, these essential processes can go haywire, leading to a range of symptoms that can significantly impact daily life. From dizziness and fainting to digestive issues and abnormal sweating, the effects are widespread and varied. Understanding autonomic dysfunction is crucial for managing its symptoms and improving quality of life. Let's dive into 40 key facts that shed light on this complex condition.
Understanding Autonomic Dysfunction
Autonomic dysfunction, also known as dysautonomia, affects the autonomic nervous system (ANS). This system controls involuntary functions like heart rate, blood pressure, digestion, and body temperature. Let's dive into some key facts about this complex condition.
-
Definition: Autonomic dysfunction occurs when the autonomic nervous system is damaged, leading to impaired control over involuntary functions.
-
Functions Controlled: The ANS manages a wide range of bodily functions, including heart rate, blood pressure, digestion, body temperature, sweating, and more.
-
Subsystems: The ANS is part of the peripheral nervous system and is divided into two main subsystems: the sympathetic nervous system and the parasympathetic nervous system.
-
Divisions: The autonomic nervous system breaks down into three divisions: the sympathetic nervous system, the parasympathetic nervous system, and the enteric nervous system.
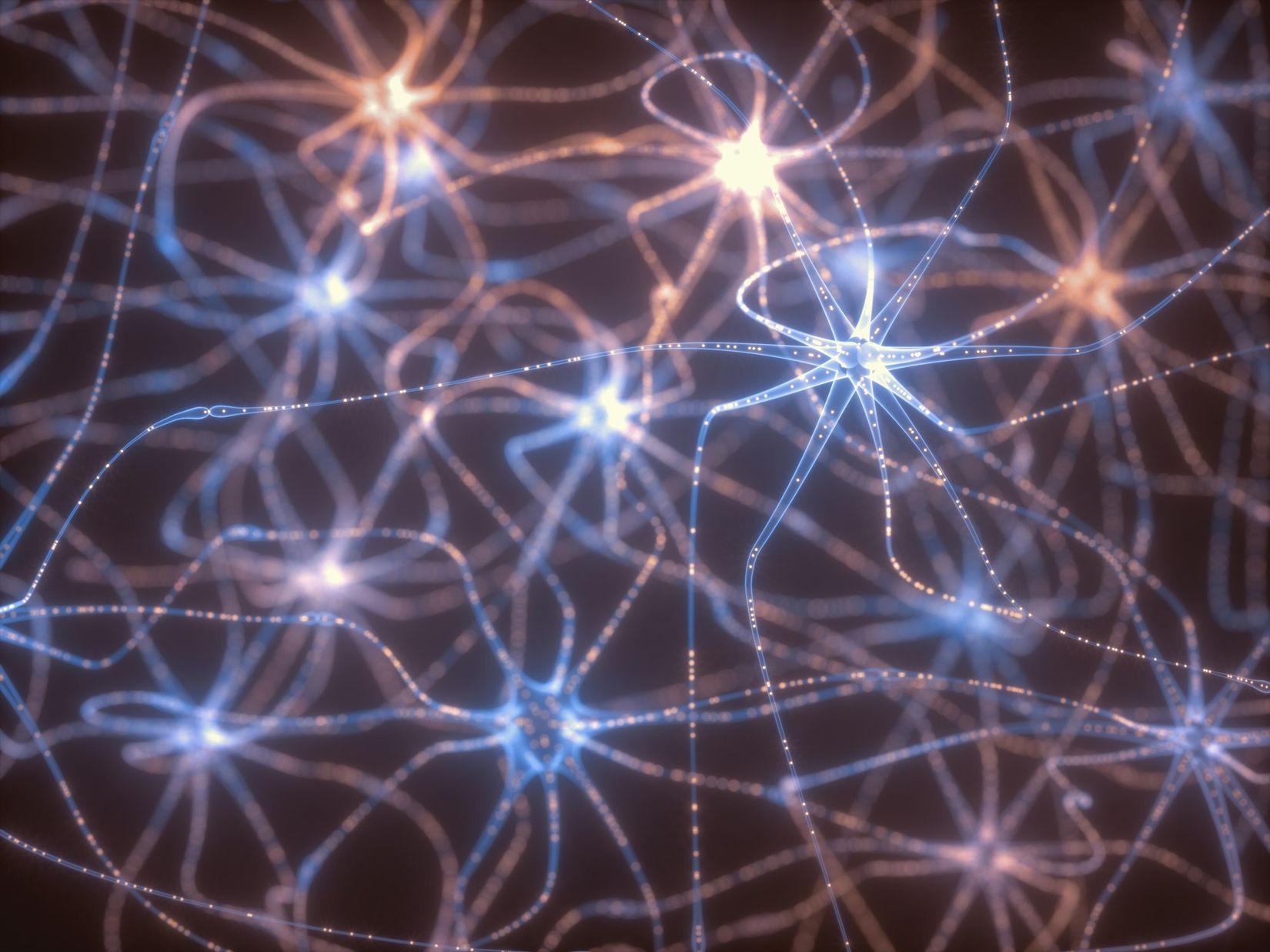
The Brain and Neural Network
The brain plays a crucial role in controlling the ANS. It operates through a complex neural network involving both the brain and spinal cord.
-
Brain Control: The autonomic nervous system is controlled by the brain, specifically the hypothalamus, which acts as the primary regulator of autonomic functions.
-
Neural Network: The ANS operates through a complex neural network involving both the brain and spinal cord. Nerve fibers from the brain and spinal cord extend to various organs and tissues, controlling their functions.
-
Cranial Nerves: Four cranial nerves (III, VII, IX, and X) are involved in autonomic functions, managing pupil dilation, eye focusing, tears, nasal mucus, saliva, and organs in the chest and belly.
-
Spinal Nerves: The ANS uses most of the 31 spinal nerves, including those in the thoracic, lumbar, and sacral regions, to control various bodily functions.
Cells and Neurons
The ANS consists of various cell types, including neurons and glial cells, which play essential roles in maintaining neural function and health.
-
Cell Types: The main cell types in the ANS include neurons and glial cells. Glial cells help develop and maintain neurons, shield the nervous system from infections, control chemical balance, and coat neurons’ axons with myelin.
-
Neuron Structure: Each neuron consists of dendrites, a cell body, and an axon. Dendrites connect to thousands of other synapses, while glial cells support these structures.
-
Glial Cells: There are 10 times more glial cells than neurons, indicating their crucial role in maintaining neural function and health.
Causes and Symptoms
Autonomic dysfunction can result from various causes, leading to a wide range of symptoms depending on the location of the damage.
-
Damage Causes: Autonomic neuropathy occurs due to damage or disease affecting the nerves of the ANS. This can result from conditions like diabetes, high blood pressure, heavy drinking, and autoimmune disorders.
-
Symptoms: Symptoms of autonomic dysfunction depend on the location of the damage. Common symptoms include orthostatic hypotension, nausea, sweating, excessive tiredness, and ill feelings.
Cardiovascular Control
The ANS plays a significant role in cardiovascular control, managing heart rate, blood pressure, and vascular tone.
-
Cardiovascular Control: The ANS plays a significant role in cardiovascular control, managing heart rate, blood pressure, and vascular tone. Dysfunction in this area can lead to conditions like orthostatic hypotension and syncope.
-
Neurocardiogenic Syncope: This is a common cause of syncope, triggered by dehydration, prolonged standing, warm surroundings, and stressful emotions. It results in a sudden slowing of blood flow to the brain.
Specific Conditions
Certain conditions are closely associated with autonomic dysfunction, each with unique characteristics and challenges.
-
Multiple System Atrophy (MSA): MSA is a fatal form of autonomic dysfunction with symptoms similar to Parkinson’s disease. It typically affects adults over 40 and has no known cure or treatment.
-
Hereditary Sensory and Autonomic Neuropathies (HSAN): HSAN is a group of genetic disorders causing widespread nerve dysfunction. It affects pain, temperature, and touch sensation and can impact various body functions.
-
Holmes-Adie Syndrome (HAS): HAS primarily affects the nerves controlling eye muscles, causing vision problems and pupil abnormalities. It may occur due to viral infections and is not life-threatening but can be permanent.
Diabetes and Other Causes
Diabetes and other conditions can lead to autonomic dysfunction, causing various symptoms and complications.
-
Diabetes-Related Damage: Diabetes is a common cause of autonomic neuropathy, leading to damage in multiple areas of the body. This can result in symptoms like orthostatic hypotension and gastrointestinal issues.
-
Parkinson’s Disease Impact: Parkinson’s disease can cause orthostatic hypotension and other symptoms of ANS damage, leading to significant disability in affected individuals.
-
Autoimmune Disorders: Autoimmune disorders like rheumatoid arthritis and lupus can also cause autonomic dysfunction by damaging the nerves of the ANS.
-
Heavy Drinking Effects: Long-term heavy drinking can lead to autonomic neuropathy, affecting various bodily functions and causing symptoms like orthostatic hypotension.
Managing Orthostatic Hypotension
Orthostatic hypotension is a common symptom of autonomic dysfunction. Managing it involves lifestyle changes and medications.
-
Orthostatic Hypotension: This condition occurs when standing up, causing a sudden drop in blood pressure. It can be managed with lifestyle changes and medication like midodrine.
-
Lifestyle Changes: Elevating the head of the bed, drinking enough fluids, adding salt to the diet, wearing compression stockings, and changing positions slowly can help alleviate orthostatic hypotension symptoms.
-
Medications: Medications such as midodrine can help manage orthostatic hypotension by increasing blood pressure when standing up.
Physical Therapy and Mental Health
Physical therapy and mental health support play crucial roles in managing autonomic dysfunction.
-
Physical Therapy: Physical therapy, walking aids, and feeding tubes may be necessary for more severe nerve involvement in autonomic dysfunction.
-
Depression and Autonomic Dysfunction: Depression is a common comorbidity with autonomic dysfunction. Therapy with a qualified counselor, therapist, or psychologist can help individuals cope with these symptoms.
Support Systems
Support from family, friends, and support groups is vital for individuals with autonomic dysfunction.
-
Support Groups: Support groups are available for individuals with autonomic dysfunction. These groups provide emotional support and help individuals set priorities to manage their condition effectively.
-
Family and Friends Support: Accepting help and support from family and friends is crucial for managing autonomic dysfunction. This can include assistance with daily tasks and emotional support.
-
Online Therapy Options: Online therapy options are available for those who prefer remote counseling. These options can provide flexibility and convenience in managing mental health related to autonomic dysfunction.
Diagnosis and Prognosis
Early diagnosis and understanding the prognostic significance of autonomic dysfunction are essential for effective management.
-
Early Diagnosis: Early diagnosis and treatment of underlying conditions causing autonomic dysfunction are essential for slowing the progression of the disease and lessening symptoms.
-
Symptom Management: Managing symptoms of autonomic dysfunction is crucial for improving quality of life. This involves addressing both physical and emotional symptoms through various treatments and lifestyle changes.
-
Complexity of Diagnosis: Diagnosing autonomic dysfunction can be complex due to the variety of symptoms and underlying causes. A comprehensive evaluation by a healthcare provider is necessary to determine the extent of damage and appropriate treatment.
Diagnostic Tests and HRV
Various tests help diagnose autonomic dysfunction, including heart rate variability (HRV) tests and autonomic function tests.
-
Diagnostic Tests: Various tests can help diagnose autonomic dysfunction, including heart rate variability (HRV) tests, blood pressure monitoring, and autonomic function tests.
-
Prognostic Significance: The prognostic significance of autonomic dysfunction has been well established, particularly in cardiovascular diseases. Diminished HRV has been associated with increased mortality and sudden cardiac death.
-
Nonlinear Analysis Techniques: Nonlinear analysis techniques have been applied to further characterize HRV, providing prognostic information beyond traditional measures. However, these techniques have not become widely used in clinical practice.
Autonomic Blockade and Exercise
Autonomic blockade and exercise play roles in understanding and managing autonomic dysfunction.
-
Autonomic Blockade: Autonomic blockade markedly attenuates all HRV measures, indicating the complexity of assessing autonomic effects on the heart.
-
Exercise and Sympathoexcitation: Exercise and conditions associated with sympathoexcitation can precipitate myocardial infarction (MI) and ventricular arrhythmias. Beta-adrenergic blockers improve survival after MI and in heart failure with reduced ejection fraction, highlighting the role of autonomic dysfunction in clinical heart disease.
Clinical Evaluation and Care Coordination
Effective clinical evaluation and care coordination are essential for managing autonomic dysfunction.
-
Clinical Evaluation: Measures of HRV have not entered the realm of clinical evaluation despite decades of study. Further efforts are required to develop optimal approaches to delineate cardiac autonomic dysfunction and its adverse effects.
-
Interprofessional Care Coordination: Improving care coordination among the interprofessional team is essential for enhancing care delivery for patients with autonomic sphere symptoms and disorders. This involves better communication and collaboration among healthcare providers to manage the complex needs of these patients.
Understanding Autonomic Dysfunction
Autonomic dysfunction, or dysautonomia, affects the autonomic nervous system (ANS), which controls involuntary body functions. The ANS is divided into the sympathetic, parasympathetic, and enteric nervous systems. Damage to the ANS can result from conditions like diabetes, high blood pressure, and autoimmune disorders. Symptoms vary but often include orthostatic hypotension, nausea, and excessive tiredness.
Managing this condition involves lifestyle changes, medications, and sometimes physical therapy. Early diagnosis and treatment are crucial for slowing progression and improving quality of life. Support from family, friends, and support groups can make a significant difference.
Understanding the complexity of autonomic dysfunction helps in recognizing symptoms and seeking appropriate care. With the right approach, individuals can manage their symptoms and lead fulfilling lives.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.