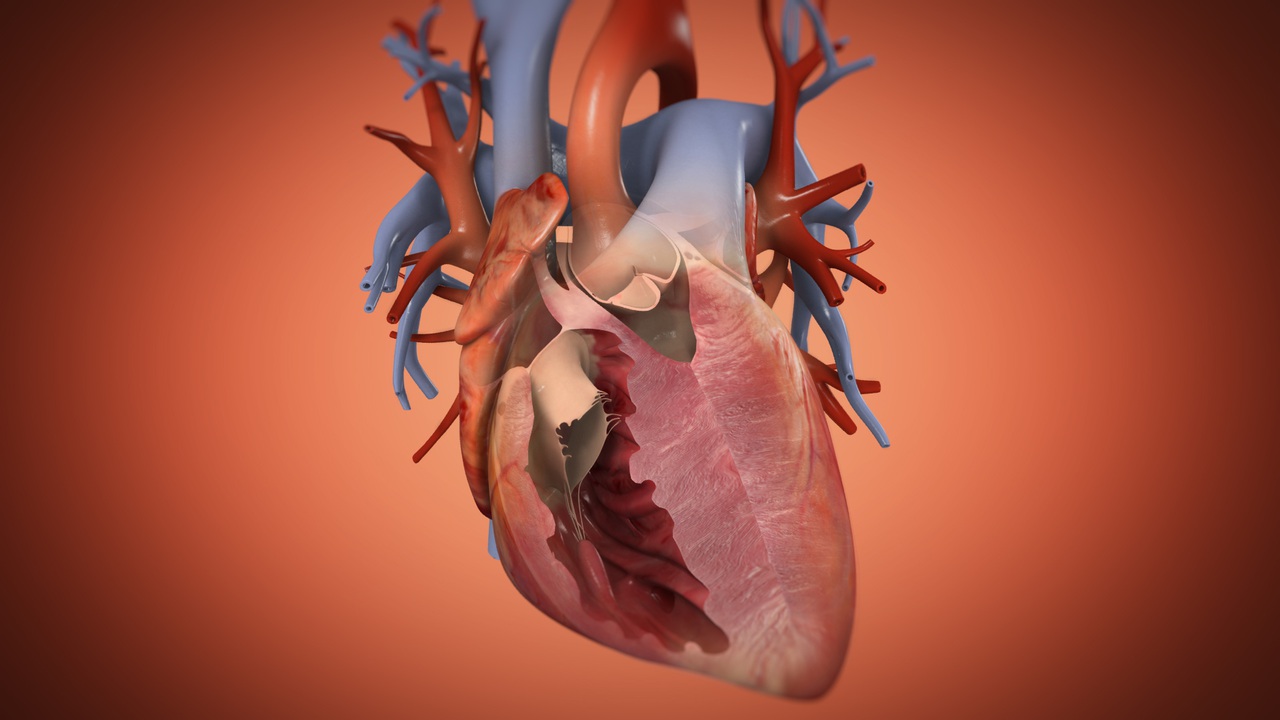
Hypoplastic Left Heart Syndrome (HLHS) is a serious congenital heart defect where the left side of the heart is underdeveloped. Affecting about 1 in 5,000 newborns, HLHS presents significant challenges right from birth. Babies with HLHS often show symptoms like cyanosis, rapid breathing, and poor feeding. Diagnosed through prenatal ultrasounds or postnatal tests like echocardiograms, this condition requires immediate medical attention. Treatment usually involves a series of surgeries, including the Norwood, Glenn, and Fontan procedures, or in some cases, a heart transplant. Despite advancements, managing HLHS is complex, requiring a dedicated medical team and ongoing care.
What is Hypoplastic Left Heart Syndrome?
Hypoplastic Left Heart Syndrome (HLHS) is a serious congenital heart defect. It affects the left side of the heart, making it underdeveloped. This condition requires immediate medical attention after birth.
-
Definition: HLHS involves the underdevelopment of the left ventricle, aortic valve, mitral valve, ascending aorta, and aortic arch.
-
Incidence: Approximately 1 in 5,000 neonates are affected by HLHS, accounting for about 3% of all congenital heart disease cases.
-
History: HLHS was first described by Nadas and NoonanFontan in 1958, initially referred to as combined aortic and mitral atresia.
Recognizing the Symptoms
Early detection of HLHS can be life-saving. Knowing the symptoms helps in seeking timely medical intervention.
-
Cyanosis: Babies with HLHS often have a grayish-blue color of the skin, lips, and nails due to poor oxygenation.
-
Rapid Breathing: Difficulty breathing and a fast heart rate are common symptoms.
-
Poor Feeding: Trouble feeding can lead to dehydration and poor weight gain.
-
Cold Hands and Feet: Sweaty, clammy, or cool skin is another sign.
-
Weak Pulse: Poor pulses in the feet can indicate HLHS.
-
Drowsiness: Unusual drowsiness or inactivity is often observed.
How is HLHS Diagnosed?
Diagnosing HLHS involves several tests and examinations. Early diagnosis can significantly improve outcomes.
-
Prenatal Ultrasound: HLHS can often be diagnosed before birth through ultrasound scans.
-
Chest X-ray: This test shows any abnormalities in the heart and lungs.
-
Electrocardiogram (ECG): Records the heart's electrical activity and detects arrhythmias.
-
Echocardiogram (Echo): Uses sound waves to create moving pictures of the heart and its valves, the primary diagnostic tool for HLHS.
Treatment Options for HLHS
Treating HLHS requires a combination of medical management and surgical interventions. The goal is to ensure adequate blood flow and manage symptoms.
-
Prostaglandin E1 (PGE1): This medication keeps the ductus arteriosus open, allowing blood to bypass the underdeveloped left side of the heart.
-
Norwood Procedure: The first stage of surgery, performed within the first two weeks of life, creates a new aorta and pulmonary artery connection.
-
Glenn Procedure: The second stage, done several months after the Norwood procedure, creates a shunt between the superior vena cava and the pulmonary artery.
-
Fontan Procedure: The final stage, performed around two years old, connects the inferior vena cava directly to the pulmonary artery.
-
Heart Transplant: In some cases, a heart transplant may be necessary if other treatments are ineffective or complications arise.
Managing HLHS with Palliative Care
Palliative care focuses on alleviating symptoms and improving the quality of life for children with HLHS.
-
Pain Management: Effective pain relief is crucial for comfort.
-
Nutritional Support: Addressing feeding challenges and ensuring adequate nutrition is vital.
-
Emotional Support: Providing emotional support to both the child and their family is essential.
Genetic Factors and Risk
Understanding the genetic aspects and risk factors of HLHS can help in early detection and management.
-
Genetic Factors: While no clear genetic causes exist, HLHS is more common in families with a history of congenital heart defects.
-
Risk Factors: Having a child with HLHS increases the risk of having another child with a similar condition.
Complications and Long-term Outcomes
Despite advances in treatment, children with HLHS may face complications later in life.
-
Arrhythmias: Abnormal heart rhythms are common.
-
Pulmonary Hypertension: High blood pressure in the lungs can occur.
-
Heart Failure: The heart may struggle to pump enough blood to meet the body's needs.
-
Infections: Increased risk of infections, particularly endocarditis, due to prosthetic material or damaged heart tissue.
Improving Survival Rates
Advances in medical care have significantly improved survival rates for babies born with HLHS.
-
Specialized Treatment Centers: Centers with experienced surgeons have higher survival rates compared to less experienced centers.
-
Prenatal Diagnosis: Early diagnosis through prenatal ultrasound allows for better preparation and planning for postnatal care.
The Role of an Interprofessional Team
Effective management of HLHS requires a collaborative approach involving various healthcare professionals.
-
Pediatric Cardiologists: Specialists in diagnosing and treating heart conditions in children.
-
Surgeons: Perform the necessary surgical interventions.
-
Nurses: Provide essential care and support throughout the treatment process.
Advances in Care and Research
Ongoing research and advancements in medical care continue to improve the outlook for children with HLHS.
-
Better Diagnostic Tools: Improved tools for early and accurate diagnosis.
-
Effective Surgical Techniques: Advances in surgical methods enhance outcomes.
-
Postoperative Care: Improved care after surgery helps in better recovery and long-term health.
Understanding HLHS: A Lifelong Journey
Hypoplastic Left Heart Syndrome (HLHS) is a serious congenital heart defect that demands immediate attention and ongoing care. From the moment of diagnosis, whether prenatally or shortly after birth, families face a challenging road ahead. The condition involves the underdevelopment of the left side of the heart, leading to severe symptoms and requiring a series of complex surgeries. Medical management, including medications like prostaglandin E1, plays a crucial role in keeping affected babies stable. Despite advances in treatment, children with HLHS often experience long-term complications, making continuous medical follow-up essential. Support from an interprofessional team and palliative care services can significantly improve quality of life. Advances in medical care and research continue to offer hope, but understanding and managing HLHS remains a lifelong journey for both patients and their families.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


