Aspergillosis is a fungal infection caused by species of the genus Aspergillus. This condition can range from mild to severe and is often associated with individuals who have compromised immune systems. Aspergillosis can manifest in various forms, including allergic reactions, colonization, and invasive tissue invasion. The most common cause is Aspergillus fumigatus, which is found everywhere in the environment. People inhale these tiny spores daily, but those with weakened immune systems are at higher risk. Symptoms vary widely, from wheezing and coughing to severe systemic infections. Diagnosing and treating aspergillosis can be challenging, requiring a combination of laboratory tests, imaging techniques, and antifungal therapies. Early detection and treatment are crucial for improving outcomes.
What is Aspergillosis?
Aspergillosis is a fungal infection caused by species of the genus Aspergillus. This condition can range from mild to severe and is often associated with individuals who have compromised immune systems. Let's dive into some key facts about this condition.
-
Definition of Aspergillosis
Aspergillosis is an opportunistic fungal infection caused by Aspergillus species. It can manifest in various forms, including allergic reactions, colonization, and invasive tissue invasion. -
Common Causes of Aspergillosis
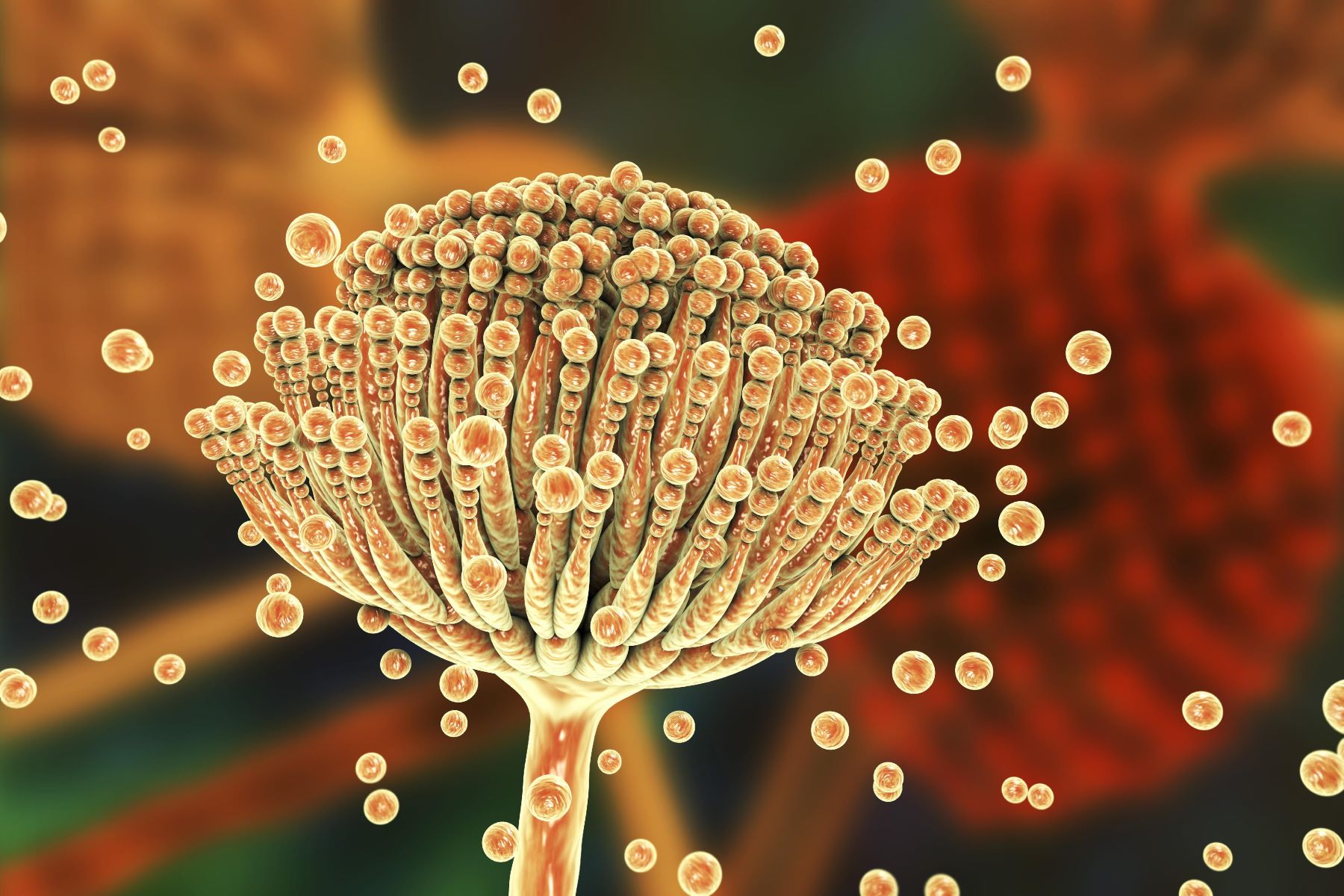
The most common cause of aspergillosis is Aspergillus fumigatus, which is ubiquitous in the environment and can be inhaled by humans and animals. -
Transmission
Aspergillosis is primarily transmitted through the inhalation of airborne conidia (spores) of Aspergillus species. These spores are small enough (2.5–3 μm) to reach the alveoli or paranasal sinuses.
Who is at Risk?
Certain factors increase the likelihood of developing aspergillosis. Understanding these can help in prevention and early diagnosis.
- Risk Factors
Several risk factors increase the likelihood of developing aspergillosis, including prolonged neutropenia, chronic administration of glucocorticoids, cytotoxic agent administration, bone marrow transplant, chronic granulomatous disease, leukemia, lymphoma, acute rejection of transplanted organs, and HIV infection.
Types of Aspergillosis
Aspergillosis can be categorized into several types based on the severity and nature of the infection.
-
Allergic Bronchopulmonary Aspergillosis (ABPA)
An allergic reaction to Aspergillus species, often seen in individuals with asthma or cystic fibrosis. -
Chronic Pulmonary Aspergillosis (CPA)
A chronic form of aspergillosis characterized by the formation of aspergillomas (fungus balls) in pre-existing lung cavities. -
Invasive Aspergillosis (IA)
A severe form of aspergillosis that invades tissues and can disseminate to other parts of the body.
Symptoms of Aspergillosis
Symptoms of aspergillosis vary depending on the type of infection. Recognizing these symptoms can lead to timely medical intervention.
-
Allergic Forms
Symptoms include wheezing, coughing, shortness of breath, and chest tightness. -
Chronic Forms
Symptoms include mild to severe hemoptysis (coughing up blood), chronic cough, and chest pain. -
Invasive Forms
Symptoms include fever, pleuritic chest pain, hemoptysis, and signs of systemic infection such as confusion, headache, and abdominal pain.
How Aspergillosis Develops
The pathogenesis of aspergillosis involves the inhalation of Aspergillus spores, which can colonize the lungs. In immunocompromised individuals, the fungus can invade tissues and cause severe infections.
-
Pathogenesis of Aspergillosis
Impaired phagocytosis is a critical factor in the development of invasive disease. -
Aspergilloma Formation
Aspergillomas are formed when Aspergillus species colonize pre-existing lung cavities, often due to conditions like pulmonary tuberculosis. These fungus balls can cause hemoptysis and other respiratory symptoms.
Where is Aspergillosis Found?
Aspergillosis is a significant health problem worldwide, particularly in immunocompromised individuals. The incidence of invasive aspergillosis has increased dramatically in recent years due to the use of more aggressive immunosuppressive therapies.
-
Epidemiology
Aspergillosis is a significant health problem worldwide, particularly in immunocompromised individuals. -
Geographical Distribution
Aspergillus fumigatus is one of the most ubiquitous airborne saprophytic fungi, found in soil, water, and decaying organic matter. Its widespread distribution contributes to the high incidence of aspergillosis globally. -
Species Diversity
The genus Aspergillus includes over 837 species, with A. fumigatus, A. flavus, and A. niger being the most commonly pathogenic species.
Diagnosing Aspergillosis
Diagnosing aspergillosis can be challenging due to the presence of Aspergillus species in the environment and as a normal commensal in the gastrointestinal tract and respiratory secretions.
-
Clinical Presentation
The clinical presentation of aspergillosis can vary widely depending on the type of infection. Common signs and symptoms include pleuritic chest pain, fever, hemoptysis, and signs of systemic infection in invasive cases. -
Diagnostic Challenges
Definitive diagnosis often requires repeated culture and microscopic examination of tissue samples. -
Laboratory Tests
Laboratory tests for diagnosing aspergillosis include blood cultures, ELISA (Enzyme-Linked Immunosorbent Assay) to detect galactomannan, and the (1,3)-β-D-Glucan test to detect β-D-glucan in serum or other body fluids. -
Imaging Techniques
Imaging techniques used for diagnosing aspergillosis include CT scans and chest radiographs.
Treatment Options
Treatment of aspergillosis depends on the severity and type of infection. Early diagnosis and treatment are crucial for improving outcomes.
-
Antifungal Therapy
Empiric antifungal therapy is often started in patients at high risk for invasive disease. -
Surgery
May be necessary for localized infections or to remove aspergillomas. -
Supportive Care
Includes management of symptoms and supportive measures such as oxygen therapy and fluid management. -
Antifungal Agents
Common antifungal agents used to treat aspergillosis include Amphotericin B, Voriconazole, and Posaconazole.
Prognosis and Prevention
The prognosis of aspergillosis varies widely depending on the severity and type of infection. Preventive measures can help reduce the risk of infection.
-
Prognosis
Invasive aspergillosis has a high mortality rate, especially in immunocompromised individuals. Early diagnosis and treatment are crucial for improving outcomes. -
Prevention Strategies
Prevention strategies for aspergillosis include minimizing the use of immunosuppressive therapies, controlling the environment to reduce exposure to Aspergillus spores, and using personal protective equipment (PPE) in high-risk settings.
Aspergillosis in Specific Populations
Certain populations are at a higher risk for developing aspergillosis. Understanding these risks can help in targeted prevention and treatment.
-
Aspergillosis in Immunocompromised Patients
Immunocompromised patients are at a higher risk for developing severe forms of aspergillosis. These patients include those with cancer, HIV/AIDS, and those undergoing chemotherapy or bone marrow transplantation. -
Aspergillosis in Cystic Fibrosis Patients
Patients with cystic fibrosis are at an increased risk for developing allergic bronchopulmonary aspergillosis (ABPA). The lung microbiome in these patients is complex, often involving multiple bacterial and fungal species. -
Aspergillosis in Asthma Patients
Asthma patients can develop allergic bronchopulmonary aspergillosis (ABPA), which is characterized by an allergic reaction to Aspergillus species. The lung microbiome in asthmatics differs significantly from that of healthy controls, and modulation between airway dysbiosis and allergen response can worsen allergy symptoms.
Complications and Chronic Forms
Aspergillosis can lead to various complications, especially in chronic forms of the disease.
-
Aspergilloma Complications
Aspergillomas can complicate a wide spectrum of cavitating pulmonary diseases, including pulmonary tuberculosis, sarcoidosis, and other chronic cavitary lung diseases. Hemoptysis is the typical manifestation, but it can be massive or even fatal in some cases. -
Chronic Pulmonary Aspergillosis (CPA)
CPA is a chronic form of aspergillosis characterized by the formation of aspergillomas in pre-existing lung cavities. It often develops in patients who have recovered from cavitary tuberculosis, with 20% of patients developing aspergillomas within 3 years.
Diagnostic Markers
Certain diagnostic markers are crucial for identifying invasive aspergillosis.
-
Galactomannan Antigen
The galactomannan antigen is a key diagnostic marker for invasive aspergillosis. It is released by Aspergillus species and can be detected in serum or other body fluids using ELISA. -
β-D-Glucan Test
The β-D-glucan test is another diagnostic tool for invasive aspergillosis. It detects β-D-glucan in serum or other body fluids, which is a component of the cell wall of Aspergillus species.
Imaging Findings
Imaging techniques play a crucial role in diagnosing aspergillosis, particularly in invasive cases.
-
CT Scan Findings
CT scans are crucial for diagnosing aspergillosis, particularly in invasive cases. Early manifestations may show characteristic signs such as the "halo sign," diffuse pulmonary infiltrates, consolidation, ground glass opacities, or the crescent sign. -
Chest Radiograph Findings
Chest radiographs can also help in diagnosing aspergillosis, showing wedge-shaped, pleural-based infiltrates. However, these findings are less specific and often require further diagnostic testing.
Treatment Outcomes and Prognostic Factors
Understanding the treatment outcomes and prognostic factors can help in managing aspergillosis effectively.
- Treatment Outcomes
Treatment outcomes for aspergillosis vary widely depending on the severity and type of infection. Invasive aspergillosis has a high mortality rate, especially in immunocompromised individuals. Early diagnosis and treatment are crucial for improving outcomes.
Key Points on Aspergillosis
Aspergillosis, caused by Aspergillus species, is a fungal infection that can range from mild to severe. It primarily affects those with compromised immune systems. Types include Allergic Bronchopulmonary Aspergillosis (ABPA), Chronic Pulmonary Aspergillosis (CPA), and Invasive Aspergillosis (IA). Symptoms vary but often involve respiratory issues like coughing, wheezing, and chest pain. Diagnosis can be tricky due to the fungus's presence in the environment. Tests like blood cultures, ELISA, and imaging techniques help identify the infection. Treatment usually involves antifungal medications such as Amphotericin B, Voriconazole, and Posaconazole. Prevention focuses on reducing exposure to spores and managing immunosuppression. Early diagnosis and treatment are crucial for better outcomes. Understanding these aspects helps in managing and preventing this opportunistic infection effectively.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


