Zygomycosis, also known as mucormycosis, is a rare but serious fungal infection caused by a group of molds called mucormycetes. These molds live throughout the environment, particularly in soil and decaying organic matter like leaves and compost piles. People with weakened immune systems are most at risk, including those with diabetes, cancer, or who have undergone organ transplants. Symptoms can vary depending on the part of the body affected but often include fever, headache, and sinus pain. Early diagnosis and treatment are crucial for survival. Understanding zygomycosis can help in recognizing its signs and seeking timely medical intervention.
Key Takeaways:
- Zygomycosis, also known as mucormycosis, is a rare but serious fungal infection that primarily affects individuals with weakened immune systems. It can be life-threatening if not treated promptly.
- Good hygiene practices, avoiding contaminated environments, and early medical intervention are crucial in preventing zygomycosis. Managing underlying health conditions and using protective gear can also reduce the risk.
What is Zygomycosis?
Zygomycosis, also known as mucormycosis, is a rare but serious fungal infection. It primarily affects individuals with weakened immune systems. Here are some intriguing facts about this condition.
-
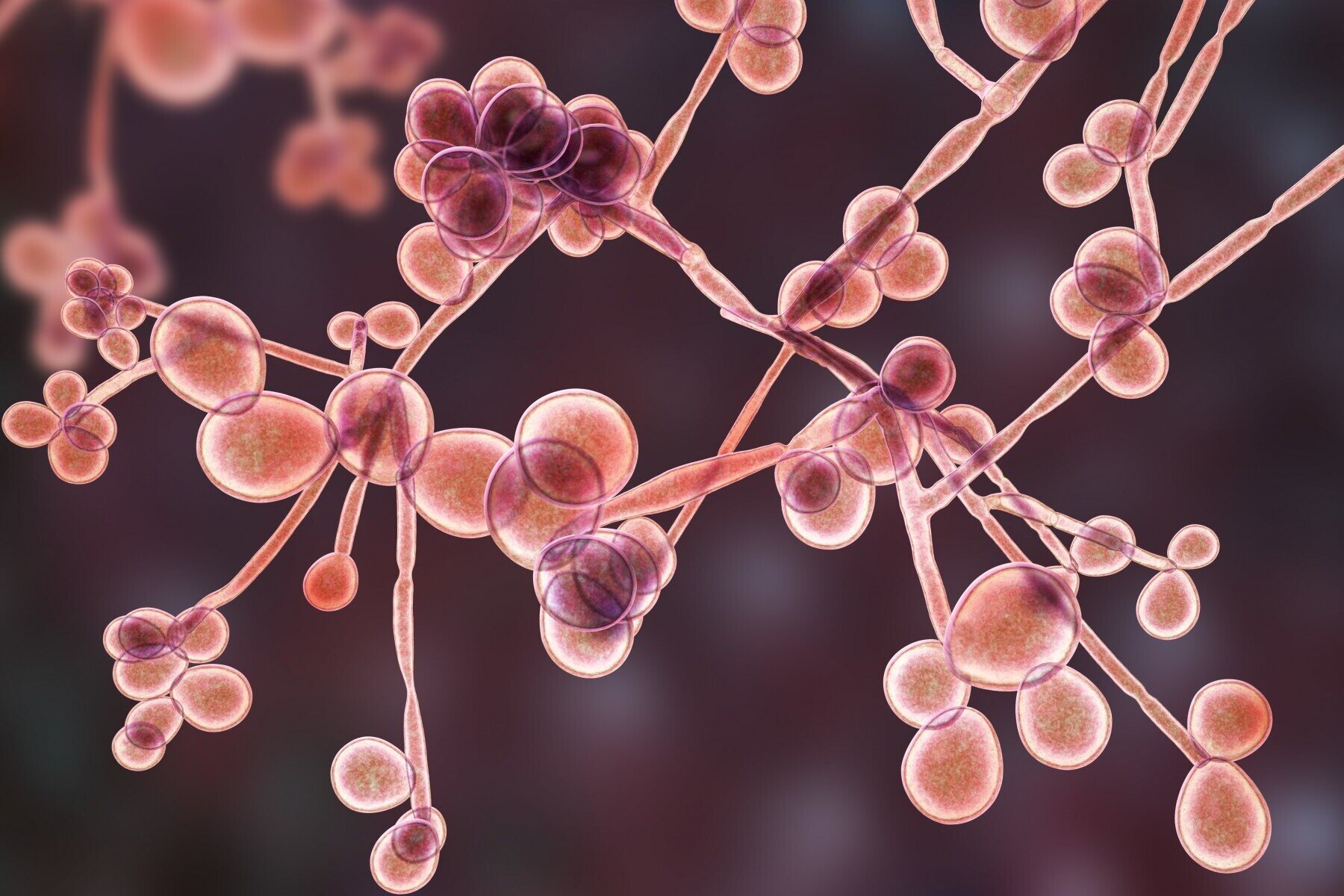
Zygomycosis is caused by fungi in the order Mucorales. These fungi are commonly found in soil, decaying organic matter, and even bread mold.
-
The infection can affect various parts of the body. It can invade the sinuses, brain, lungs, skin, and gastrointestinal tract.
-
Diabetes is a significant risk factor. People with uncontrolled diabetes are more susceptible due to high blood sugar levels and ketoacidosis.
-
Symptoms vary depending on the infection site. Sinus infections may cause facial swelling, while lung infections can lead to fever and cough.
-
Zygomycosis can be life-threatening. If not treated promptly, it can spread rapidly and cause severe complications.
How is Zygomycosis Diagnosed?
Diagnosing zygomycosis involves various methods to confirm the presence of the fungal infection. Here are some key facts about the diagnostic process.
-
Biopsy is a common diagnostic tool. A tissue sample is taken from the infected area and examined under a microscope.
-
Imaging tests help identify the extent of the infection. CT scans and MRIs can reveal the spread of the fungus in the body.
-
Blood tests are not always reliable. They may not detect the fungus, making tissue biopsy more crucial.
-
Early diagnosis is critical. Prompt identification and treatment can significantly improve the prognosis.
-
Histopathology can reveal characteristic features. The presence of broad, ribbon-like hyphae is indicative of zygomycosis.
Treatment Options for Zygomycosis
Treating zygomycosis requires a combination of antifungal medications and sometimes surgical intervention. Here are some important facts about treatment.
-
Amphotericin B is the primary antifungal drug used. It is effective against the fungi causing zygomycosis.
-
Posaconazole and isavuconazole are alternative treatments. These antifungal agents can be used if the patient cannot tolerate amphotericin B.
-
Surgical debridement may be necessary. Removing infected tissue can help control the spread of the infection.
-
Hyperbaric oxygen therapy is sometimes used. This treatment increases oxygen levels in tissues, helping to kill the fungus.
-
Managing underlying conditions is crucial. Controlling diabetes or other risk factors can improve treatment outcomes.
Risk Factors for Zygomycosis
Certain conditions and behaviors increase the risk of developing zygomycosis. Here are some facts about these risk factors.
-
Immunocompromised individuals are at higher risk. This includes people with HIV/AIDS, cancer, or those on immunosuppressive drugs.
-
Trauma or burns can lead to skin infections. Open wounds provide an entry point for the fungus.
-
Prolonged use of corticosteroids can increase susceptibility. These drugs weaken the immune system, making it easier for the fungus to invade.
-
Malnutrition is a significant risk factor. Poor nutrition weakens the body's defenses against infections.
-
Iron overload conditions can promote fungal growth. Excess iron in the body creates an environment conducive to fungal proliferation.
Preventing Zygomycosis
While it may not always be possible to prevent zygomycosis, certain measures can reduce the risk. Here are some preventive strategies.
-
Good hygiene practices are essential. Regular handwashing and keeping wounds clean can help prevent infections.
-
Avoiding exposure to contaminated environments is crucial. People with weakened immune systems should stay away from areas with high fungal spore concentrations.
-
Proper management of underlying health conditions is vital. Keeping diabetes and other chronic diseases under control can lower the risk.
-
Using protective gear in high-risk environments can help. Masks and gloves can reduce exposure to fungal spores.
-
Early medical intervention is key. Seeking prompt treatment for infections or injuries can prevent complications.
Interesting Facts about Zygomycosis
Here are some additional intriguing facts about zygomycosis that you might find interesting.
-
Zygomycosis was first described in 1885. The condition has been known for over a century.
-
The infection is more common in tropical and subtropical regions. Warm, humid climates favor the growth of the fungi.
-
Zygomycosis can affect animals as well. Livestock and pets can also contract the infection.
-
The mortality rate is high if untreated. Without prompt treatment, the infection can be fatal in up to 90% of cases.
-
Research is ongoing to find better treatments. Scientists are continually studying new antifungal agents and therapies to combat zygomycosis.
Understanding Zygomycosis
Zygomycosis, also known as mucormycosis, is a serious fungal infection caused by fungi in the order Mucorales. It primarily affects individuals with weakened immune systems, such as those with diabetes, cancer, or organ transplants. Early diagnosis and treatment are crucial for improving outcomes, as the infection can rapidly progress and become life-threatening. Symptoms vary depending on the infection site but often include fever, facial swelling, and black lesions on the nasal bridge or upper inside of the mouth. Treatment typically involves antifungal medications and, in severe cases, surgical removal of infected tissue. Preventive measures include managing underlying health conditions and maintaining good hygiene. Awareness and prompt medical attention can make a significant difference in managing this rare but dangerous infection. Stay informed, take precautions, and consult healthcare professionals if you suspect any symptoms.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


