Pulmonary-Renal Syndrome is a rare but serious condition that affects both the lungs and kidneys. This syndrome can lead to life-threatening complications if not diagnosed and treated promptly. What causes Pulmonary-Renal Syndrome? It often stems from autoimmune diseases like Goodpasture's syndrome or systemic lupus erythematosus. Symptoms may include coughing up blood, shortness of breath, and swelling in the legs. How is it diagnosed? Doctors typically use blood tests, imaging studies, and sometimes a biopsy. Treatment usually involves immunosuppressive medications and, in severe cases, plasmapheresis. Understanding this syndrome is crucial for early intervention and better outcomes.
Key Takeaways:
- Pulmonary-Renal Syndrome (PRS) is a rare but serious condition affecting the lungs and kidneys, often caused by autoimmune diseases. Early recognition of symptoms and prompt treatment are crucial for managing PRS.
- Symptoms of PRS include coughing up blood, difficulty breathing, and blood in the urine. Accurate diagnosis through blood and urine tests, chest X-rays, and kidney biopsies is essential for effective treatment.
What is Pulmonary-Renal Syndrome?
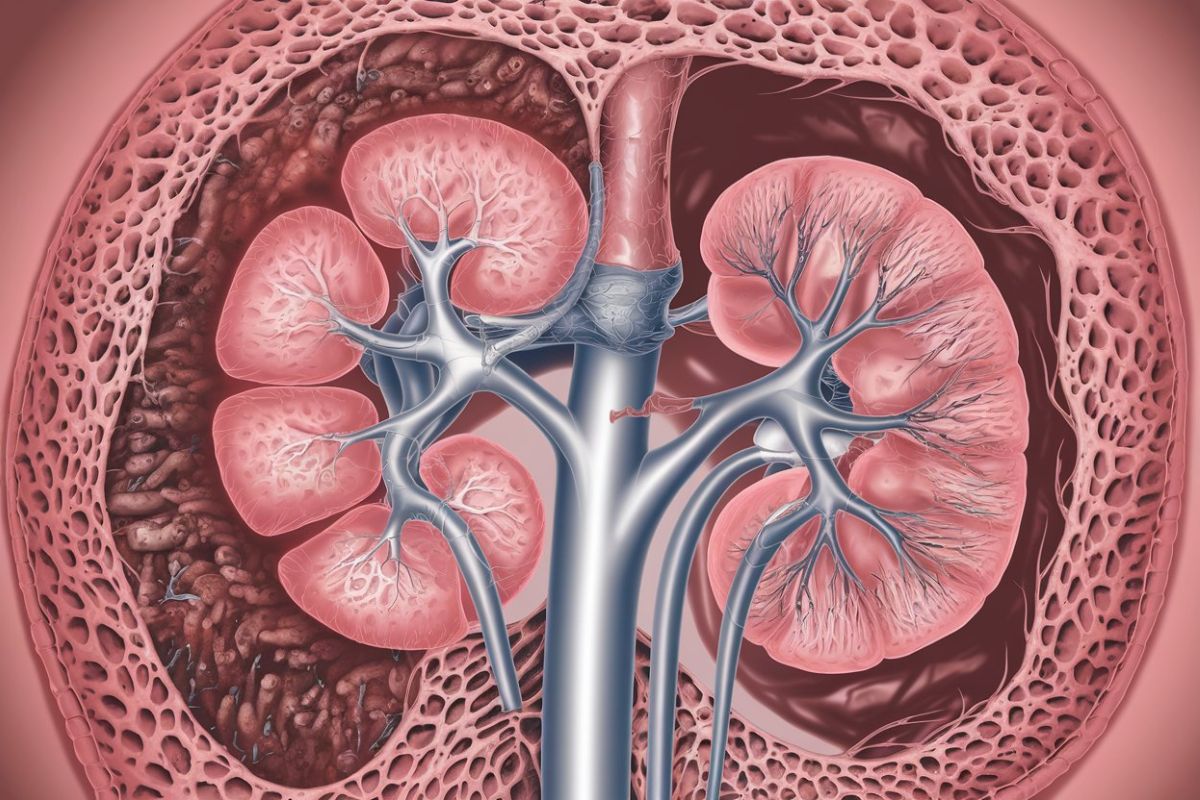
Pulmonary-Renal Syndrome (PRS) is a rare but serious condition that affects both the lungs and kidneys. It involves inflammation and bleeding in the small blood vessels of these organs. Understanding PRS can help in recognizing symptoms early and seeking appropriate treatment.
-
PRS is a combination of lung and kidney disease. It involves both pulmonary hemorrhage and glomerulonephritis, which is inflammation of the kidney's filtering units.
-
Autoimmune diseases often cause PRS. Conditions like Goodpasture syndrome, systemic lupus erythematosus, and Wegener's granulomatosis are common culprits.
-
Symptoms can be severe and sudden. Patients may experience coughing up blood, shortness of breath, and blood in the urine.
-
Diagnosis requires multiple tests. Blood tests, urine tests, chest X-rays, and kidney biopsies are often needed to confirm PRS.
-
Treatment usually involves immunosuppressive drugs. Medications like corticosteroids and cyclophosphamide help reduce inflammation and immune system activity.
Causes of Pulmonary-Renal Syndrome
Understanding the causes of PRS can help in early detection and management. Various factors contribute to this syndrome, making it essential to know what to look out for.
-
Goodpasture syndrome is a leading cause. This autoimmune disorder causes the immune system to attack the lungs and kidneys.
-
Systemic lupus erythematosus (SLE) can trigger PRS. SLE is another autoimmune disease that can cause widespread inflammation, including in the lungs and kidneys.
-
Wegener's granulomatosis is also a culprit. Now known as granulomatosis with polyangiitis, this condition causes inflammation of blood vessels.
-
Certain infections can lead to PRS. Bacterial, viral, and fungal infections can sometimes trigger the syndrome.
-
Medications may induce PRS. Some drugs, particularly those affecting the immune system, can cause this condition.
Symptoms of Pulmonary-Renal Syndrome
Recognizing the symptoms of PRS is crucial for timely treatment. The signs can be alarming and often require immediate medical attention.
-
Hemoptysis is a common symptom. Coughing up blood is often one of the first signs of PRS.
-
Shortness of breath can occur. Difficulty breathing is another alarming symptom that needs prompt evaluation.
-
Blood in the urine is a red flag. Hematuria, or blood in the urine, indicates kidney involvement.
-
Fatigue and weakness are frequent complaints. These symptoms result from the body's struggle to cope with the inflammation.
-
Joint pain may also be present. Inflammation can affect multiple body parts, including the joints.
Diagnosis of Pulmonary-Renal Syndrome
Accurate diagnosis is essential for effective treatment. Multiple tests are often required to confirm PRS and rule out other conditions.
-
Blood tests are crucial. They help detect antibodies and other markers of inflammation.
-
Urine tests reveal kidney involvement. These tests can show blood, protein, and other abnormalities in the urine.
-
Chest X-rays are often used. They help identify lung involvement and rule out other causes of symptoms.
-
Kidney biopsies provide definitive diagnosis. A small sample of kidney tissue is examined under a microscope.
-
CT scans may be necessary. These imaging tests offer detailed views of the lungs and kidneys.
Treatment Options for Pulmonary-Renal Syndrome
Effective treatment can significantly improve outcomes for PRS patients. Various therapies aim to reduce inflammation and manage symptoms.
-
Corticosteroids are commonly used. These drugs help reduce inflammation quickly.
-
Cyclophosphamide is another option. This immunosuppressive drug is often used in severe cases.
-
Plasmapheresis can be beneficial. This procedure removes harmful antibodies from the blood.
-
Rituximab is a newer treatment. This medication targets specific immune cells involved in PRS.
-
Supportive care is essential. Oxygen therapy, dialysis, and other supportive measures help manage symptoms.
Prognosis and Long-term Management
Living with PRS requires ongoing care and monitoring. Understanding the long-term outlook can help patients and families prepare for the future.
-
Early treatment improves prognosis. Prompt medical intervention can prevent severe complications.
-
Regular monitoring is crucial. Frequent check-ups help detect any changes in the condition.
-
Lifestyle changes can help. A healthy diet, regular exercise, and avoiding smoking can improve overall health.
-
Emotional support is important. Coping with a chronic illness can be challenging, so emotional and psychological support is beneficial.
-
Research is ongoing. Scientists continue to study PRS to develop better treatments and improve outcomes.
Final Thoughts on Pulmonary-Renal Syndrome
Pulmonary-Renal Syndrome (PRS) is a serious condition that affects both the lungs and kidneys. Understanding its symptoms, causes, and treatments can make a big difference in managing the disease. Early diagnosis is crucial for better outcomes. Treatments often involve medications to control the immune system and reduce inflammation. Regular check-ups and monitoring are essential to keep the condition under control.
Living with PRS can be challenging, but with the right medical support and lifestyle adjustments, many people lead fulfilling lives. Staying informed and proactive about your health is key. Always consult healthcare professionals for personalized advice and treatment plans.
Remember, knowledge is power. The more you know about PRS, the better equipped you'll be to handle it. Stay vigilant, stay informed, and take charge of your health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


