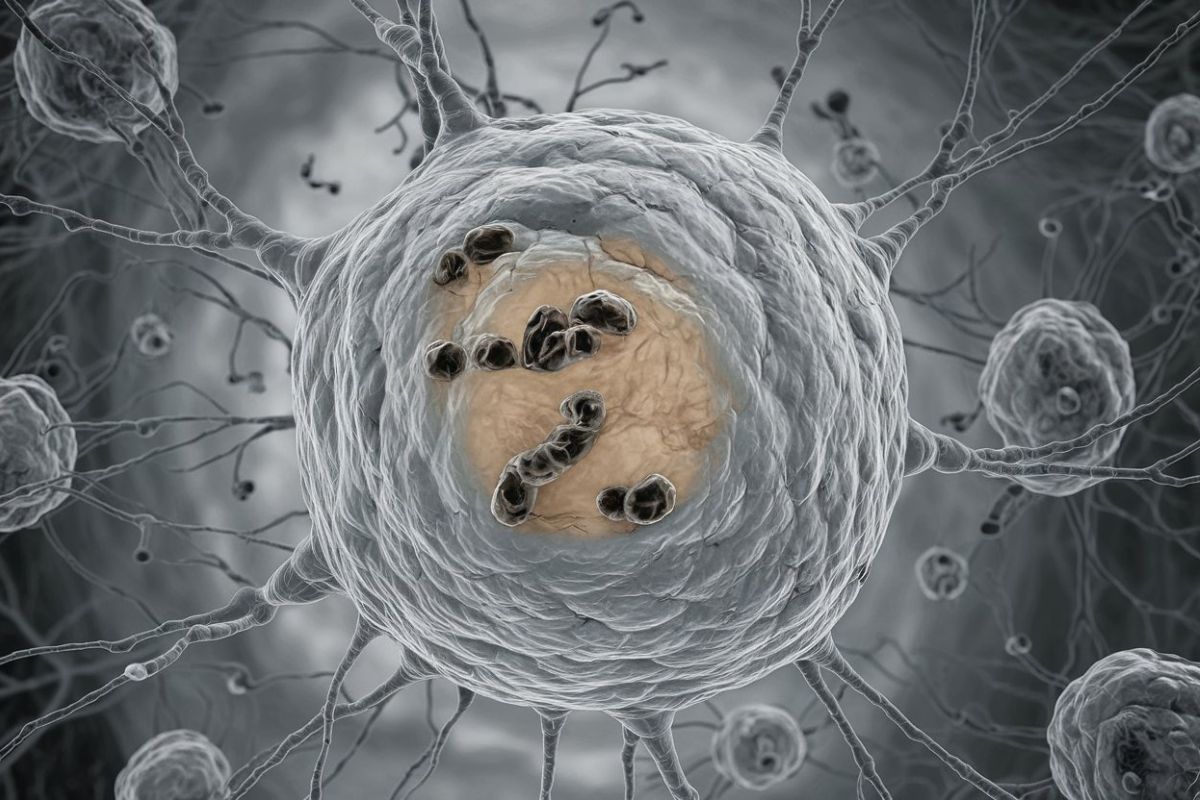
What is Mitochondrial DNA Depletion Syndrome (MDS)? Mitochondrial DNA Depletion Syndrome (MDS) is a rare genetic disorder that causes a significant reduction in mitochondrial DNA (mtDNA) within cells. This reduction hampers the mitochondria's ability to produce energy, leading to various symptoms affecting multiple organs. MDS typically appears early in life, often during infancy or the first two years. Symptoms can include muscle weakness, seizures, developmental delays, and liver problems. The condition is usually inherited in an autosomal recessive pattern, meaning both parents must carry the mutated gene. Diagnosing MDS involves genetic testing, and while there's no cure, supportive care and emerging therapies aim to manage symptoms and improve quality of life.
Key Takeaways:
- Mitochondrial DNA Depletion Syndrome (MDS) is a rare genetic disorder affecting energy production in cells, leading to symptoms like muscle weakness, seizures, and liver problems, often appearing in early childhood.
- Understanding the genetic causes of MDS is crucial for family planning and developing new therapeutic strategies, while ongoing research offers hope for improved care and treatment options.
What is Mitochondrial DNA Depletion Syndrome?
Mitochondrial DNA Depletion Syndrome (MDS) is a rare genetic disorder that affects the mitochondria, the powerhouses of our cells. This condition leads to a significant reduction in mitochondrial DNA (mtDNA), impairing the cell's ability to produce energy. Let's dive into some key facts about this complex condition.
-
Definition and Prevalence: MDS refers to a group of rare genetic disorders characterized by a severe reduction in mtDNA content within cells. It's considered a rare condition with an unclear exact prevalence.
-
Causes: Mutations in nuclear genes involved in mitochondrial dNTP synthesis or mtDNA replication cause MDS. Key genes include TK2, SUCLA2, SUCLG1, RRM2B, DGUOK, and TYMP.
-
Genetic Inheritance: MDS typically follows an autosomal recessive inheritance pattern. This means a person must inherit two copies of the mutated gene, one from each parent, to develop the condition.
Symptoms and Organ Involvement
MDS can manifest in various ways, affecting multiple organs and systems in the body. Here are some common symptoms and areas of involvement.
-
Symptoms: Onset usually occurs early in life, often during infancy or the first two years. Symptoms include developmental regression, muscle weakness, seizures, difficulty feeding, and liver problems.
-
Organ Involvement: MDS can affect multiple organs, including the muscles, gastrointestinal system, brain, and liver. The severity and specific organs involved vary among individuals.
-
Brain Involvement: Neurologic manifestations like seizures, movement disorders, ataxia, and stroke-like episodes are common. SUCLA2-related MDS, for example, affects early brain development.
-
Muscle Weakness: Muscle weakness (hypotonia) is frequent, delaying motor skills development. Affected infants may struggle with eating and require a feeding tube.
-
Liver Involvement: Liver dysfunction is common, with symptoms like elevated hepatic transaminase levels. Severe cases may lead to liver failure, necessitating a transplant.
-
Hearing Loss: Sensorineural hearing loss can occur. Regular audiology testing is recommended, and hearing aids or cochlear implants may be necessary.
-
Intellectual Disabilities: Intellectual disabilities can occur, especially in SUCLA2-related cases. The severity varies widely among individuals.
Metabolic and Prognostic Factors
Understanding the metabolic abnormalities and prognosis of MDS is crucial for managing the condition effectively.
-
Metabolic Abnormalities: Elevated methylmalonic acid levels are common, particularly in SUCLA2-related MDS, where methylmalonic aciduria is a characteristic feature.
-
Prognosis: Prognosis varies widely depending on the genetic cause and severity of organ involvement. Approximately 30% of individuals with SUCLA2-related MDS do not survive past childhood.
Diagnostic Methods and Advances
Accurate diagnosis is essential for managing MDS. Recent advances in genetic testing have improved diagnostic capabilities.
-
Diagnostic Methods: Diagnosis typically involves genetic testing to identify the underlying nuclear gene mutation. Blood tests are often sufficient, though muscle or liver biopsies may be needed.
-
Genetic Testing Advances: Next-generation sequencing (NGS) technologies have significantly improved MDS diagnosis, allowing for the identification of multiple genetic mutations simultaneously.
Therapeutic Options and Supportive Care
While there is no cure for MDS, various therapeutic strategies and supportive care options can help manage symptoms and improve quality of life.
-
Therapeutic Options: Medications supporting mitochondrial enzyme deficiencies, such as amino acids, antioxidants, and vitamins, are being explored. Liver transplants may be an option for managing liver failure.
-
Supportive Care: Regular monitoring by specialists like neurologists, gastroenterologists, and audiologists is crucial for managing symptoms and complications.
Family Planning and Molecular Understanding
Understanding the genetic causes of MDS is important for family planning and developing new therapeutic strategies.
-
Family Planning: Identifying causative genes helps with family planning and prenatal diagnosis, allowing parents to make informed decisions about future pregnancies.
-
Molecular Basis Understanding: Research into the molecular mechanisms underlying MDS is essential for developing novel and effective therapeutic strategies.
Resource Availability and Clinical Heterogeneity
Caring for a child with MDS can be overwhelming. Resources and individualized care plans are crucial for managing this complex condition.
-
Resource Availability: Resources like the Mitochondrial Medicine Program provide support and guidance for families, helping them navigate the complex care required.
-
Clinical Heterogeneity: MDS is a clinically heterogeneous group of disorders with varying degrees of organ involvement and symptom severity, necessitating individualized care plans.
Mitochondrial dNTP Pool Maintenance and Replication Defects
Mutations affecting mitochondrial dNTP pool maintenance and mtDNA replication are key contributors to MDS.
-
Mitochondrial dNTP Pool Maintenance: Mutations in genes encoding proteins that maintain the mitochondrial dNTP pool lead to mtDNA depletion.
-
mtDNA Replication Defects: Mutations in genes essential for mtDNA replication impair the replication process, leading to reduced mtDNA content.
Energy Production and Organ Dysfunction
The primary consequence of mtDNA depletion is impaired energy production, leading to organ dysfunction.
-
Energy Production Impairment: Reduced mtDNA content impairs energy production in affected tissues and organs, as mtDNA is required for synthesizing key subunits of mitochondrial respiratory chain complexes.
-
Organ Dysfunction: Impaired energy production results in organ dysfunction, manifesting as muscle weakness, developmental delays, seizures, and other systemic symptoms.
Specific Syndromes and Symptom Variability
MDS encompasses several specific syndromes, each with unique characteristics and symptom variability.
-
Specific Syndromes: Specific syndromes associated with MDS include SUCLA2-related MDS, affecting brain development, and FBXL4-related encephalomyopathic MDS, affecting multiple organs.
-
Symptom Variability: Symptoms vary significantly among individuals. Some may experience severe developmental delays and organ dysfunction, while others may have milder manifestations developing later in life.
Management Challenges and Research Directions
Managing MDS poses significant challenges due to its rarity and clinical heterogeneity. Ongoing research aims to improve understanding and treatment options.
-
Management Challenges: Regular monitoring by multiple specialists and adherence to individualized care plans are crucial for optimizing patient outcomes.
-
Research Directions: Research focuses on understanding the molecular mechanisms underlying MDS, developing new diagnostic tools, and exploring novel therapeutic strategies.
Family Support and Future Outlook
Supporting families affected by MDS is essential. Resources and ongoing research offer hope for improved care and treatment options.
-
Family Support: Resources like the Mitochondrial Medicine Program provide emotional support, educational materials, and practical guidance for families.
-
Future Outlook: Ongoing research and the development of new diagnostic and therapeutic tools hold promise for improving the lives of those affected by MDS.
Understanding Mitochondrial DNA Depletion Syndrome
Mitochondrial DNA Depletion Syndrome (MDS) is a rare, complex genetic disorder that significantly reduces mitochondrial DNA within cells. This reduction impairs energy production, leading to various symptoms like muscle weakness, developmental delays, seizures, and liver dysfunction. MDS usually appears early in life and can affect multiple organs. Diagnosing MDS involves genetic testing, often using next-generation sequencing. While there's no cure, supportive care and potential therapies, including liver transplants, can help manage symptoms. Research continues to explore new treatments and improve diagnostic tools. Families dealing with MDS need comprehensive support, including resources like the Mitochondrial Medicine Program. Understanding the genetic causes and clinical manifestations of MDS is crucial for providing optimal care and improving patient outcomes. Ongoing research offers hope for better treatments and a brighter future for those affected by this challenging condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


