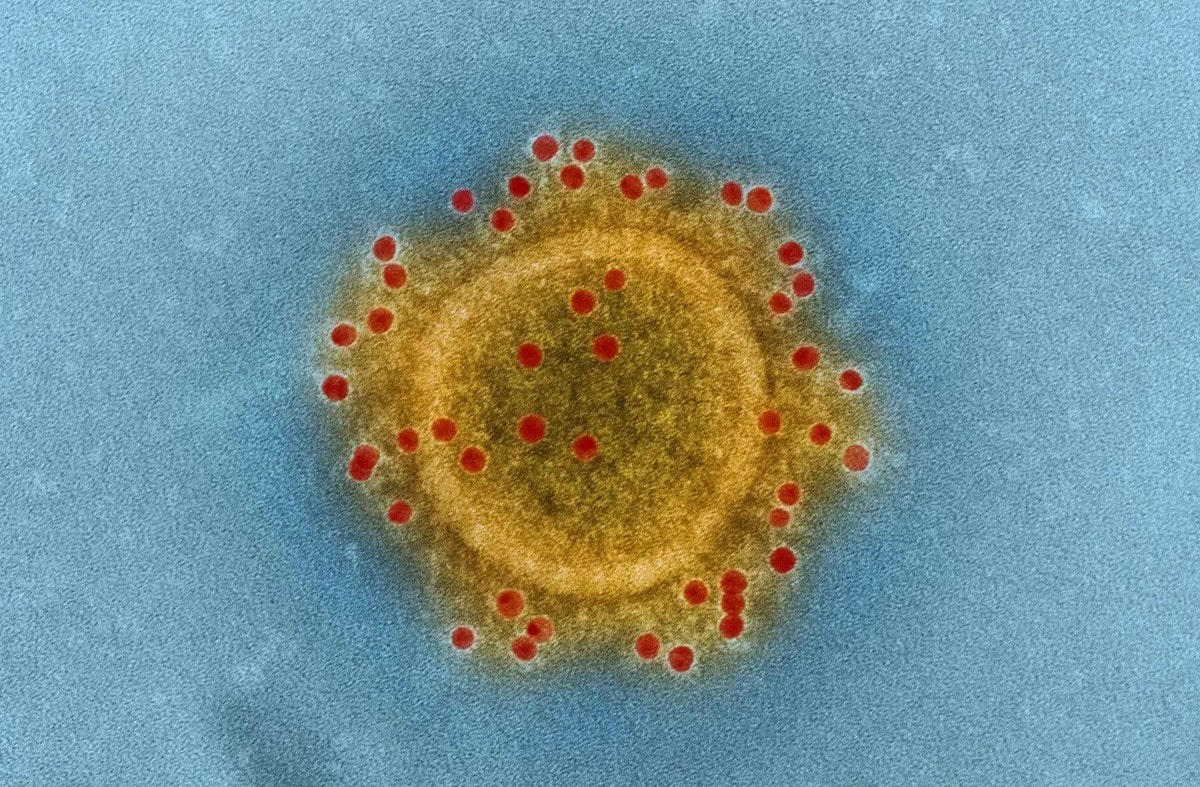
What is Middle East Respiratory Syndrome (MERS)? Middle East Respiratory Syndrome, or MERS, is a viral respiratory illness caused by the MERS-CoV virus. First identified in Saudi Arabia in 2012, this virus is believed to have originated from bats and later transmitted to dromedary camels. The virus spreads to humans through direct or indirect contact with infected camels. While human-to-human transmission is rare, it can occur, especially in healthcare settings. Symptoms range from mild respiratory issues to severe pneumonia and even death. With a high mortality rate of 30-40%, understanding MERS is crucial for public health.
Key Takeaways:
- MERS is a viral respiratory illness transmitted from camels to humans. It can cause severe symptoms and is more dangerous for people with pre-existing medical conditions. Preventive measures and public awareness are crucial.
- International coordination and ongoing research are essential in combating MERS. Understanding the symptoms, high-risk groups, and global impact can help in developing effective treatments and vaccines.
What is Middle East Respiratory Syndrome?
Middle East Respiratory Syndrome (MERS) is a viral respiratory illness caused by the MERS-CoV virus. Understanding its origins, transmission, and symptoms is crucial for public health.
-
First Identified Case: The first identified case of MERS was reported in September 2012 in a patient from Saudi Arabia who had hypoxemic respiratory failure and multiorgan illness.
-
Viral Origin: The MERS-CoV virus is believed to have originated from bats and later transmitted to dromedary camels, which are considered the primary animal reservoir.
-
Transmission: MERS-CoV is transmitted between animals and humans through direct or indirect contact with infected dromedary camels. This can occur through exposure to camel nasal secretions, milk, urine, feces, meat, or birthing products.
How Does MERS Spread?
Understanding how MERS spreads helps in taking preventive measures. The virus can move from animals to humans and between humans, though the latter is less common.
-
Global Spread: Since its first identification, MERS-CoV has been reported in 27 countries, with the majority of cases linked to countries in or near the Arabian Peninsula.
-
Human-to-Human Transmission: While human-to-human transmission is possible, it is relatively rare and mostly occurs in healthcare settings. Transmission between family members has been documented, but it is not common.
-
Healthcare Settings: The majority of reported cases involve healthcare settings, where the virus can spread from patients to healthcare providers and between patients before diagnosis.
Symptoms and Severity of MERS
MERS can range from mild to severe. Knowing the symptoms can help in early detection and treatment.
-
Symptoms: MERS-CoV infections range from asymptomatic to severe acute respiratory disease. Common symptoms include fever, cough, and shortness of breath. Pneumonia is a common finding, but not always present. Gastrointestinal symptoms like diarrhea have also been reported.
-
Severe Illness: Severe illness can cause respiratory failure requiring mechanical ventilation and support in an intensive care unit. The virus appears to cause more severe disease in older people, those with weakened immune systems, and those with chronic diseases such as renal disease, cancer, chronic lung disease, and diabetes.
-
Mortality Rate: The case fatality rate for MERS-CoV is approximately 30-40%, although this may be an overestimate due to the underreporting of mild cases.
Who is at Risk?
Certain groups are more vulnerable to severe MERS. Knowing who is at risk can guide preventive measures.
- Risk Factors: People with diabetes, renal failure, chronic lung disease, and immunocompromised individuals are at high risk of severe disease from MERS-CoV infection. These individuals should avoid contact with camels, drinking raw camel milk or urine, or eating meat that has not been properly cooked.
Diagnosing and Treating MERS
Early diagnosis and supportive treatment are key to managing MERS. There are specific methods to diagnose the virus.
-
Diagnostic Methods: Real-time reverse-transcription–polymerase-chain-reaction (RT-PCR) testing of respiratory secretions is the mainstay for diagnosing MERS-CoV. Samples from the lower respiratory tract have the greatest yield among seriously ill patients.
-
No Antiviral Therapy: There is no antiviral therapy of proven efficacy for MERS-CoV. Treatment remains largely supportive, focusing on managing symptoms and complications.
-
Vaccine Development: Several MERS-CoV specific vaccines are in development, but none are currently available for public use. Ongoing research aims to develop effective vaccines to combat the virus.
MERS in Healthcare Settings
Healthcare settings are hotspots for MERS transmission. Strict infection control measures are essential.
- Transmission in Healthcare Settings: In healthcare settings, MERS-CoV can spread through close contact with infected patients or contaminated surfaces. This highlights the importance of infection control measures in healthcare facilities.
Community and Global Impact
MERS has affected communities and countries worldwide. Understanding its global impact helps in coordinated responses.
-
Community Clusters: Intermittent sporadic cases and community clusters of MERS-CoV continue to occur, particularly in regions where dromedary camels are present.
-
Outbreaks: Large outbreaks of human-to-human transmission have occurred, including the largest known outbreak in Riyadh and Jeddah in 2014 and in South Korea in 2015.
-
Travel-Associated Cases: Travel-associated cases have been identified in several countries, including Algeria, Austria, China, Egypt, France, Germany, Greece, Italy, Malaysia, Netherlands, Philippines, Republic of Korea, Thailand, Tunisia, Turkey, United Kingdom (UK), and United States (US).
-
US Cases: Only two cases have been reported in the United States, both in men who had recently returned from Saudi Arabia. These cases highlight the potential for travel-related transmission.
Public Health Measures and Research
Public health measures and ongoing research are vital in combating MERS. Agencies worldwide are working together to understand and prevent the virus.
-
CDC Guidance: The Centers for Disease Control and Prevention (CDC) has published guidance for health departments and healthcare infection-control programs to investigate potential cases of MERS and prevent its spread.
-
Public Health Measures: Public health agencies continue to investigate clusters of cases in several countries to better understand how MERS-CoV spreads and to implement effective prevention measures.
-
Prevention Tips: To reduce the risk of respiratory illnesses like MERS, individuals should practice good hygiene by washing hands often with soap and water for at least 20 seconds, using an alcohol-based hand sanitizer if soap and water are not available, covering the nose and mouth with a tissue when coughing or sneezing, and avoiding close contact with sick individuals.
Understanding MERS Symptoms and Complications
Recognizing the onset and range of symptoms can aid in early detection and treatment.
-
Symptom Onset: Symptoms of MERS-CoV typically start to appear about 5 or 6 days after exposure but can range from 2 to 14 days.
-
Mild Symptoms: Some people infected with MERS-CoV may experience mild symptoms, such as cold-like symptoms, or no symptoms at all.
-
Severe Complications: For many people with MERS, more severe complications follow, such as pneumonia and kidney failure. These complications can lead to multiorgan failure and death.
High-Risk Groups and Global Response
Certain groups are more vulnerable to severe MERS. The global response involves collaboration and research.
-
High-Risk Groups: Individuals with pre-existing medical conditions such as diabetes, cancer, chronic lung disease, chronic heart disease, and chronic kidney disease are at higher risk for severe illness from MERS-CoV infection.
-
Global Response: The global response to MERS-CoV involves ongoing collaboration between public health agencies, research institutions, and healthcare providers to better understand the virus, develop effective treatments, and implement prevention measures.
Ongoing Research and Public Awareness
Research and public awareness are key to combating MERS. Efforts are ongoing to understand and prevent the virus.
-
Ongoing Research: Ongoing research aims to fill gaps in knowledge regarding the evolution and transmission of MERS-CoV, disease pathogenesis, treatment, and vaccine development.
-
Public Awareness: Public awareness campaigns are crucial in educating people about the risks associated with MERS-CoV and the importance of preventive measures, especially for high-risk groups.
International Coordination and Future Prospects
International coordination and future research hold promise for combating MERS. Continued efforts are essential.
-
International Coordination: International coordination is essential for monitoring risk and informing preventive measures. The World Health Organization (WHO) plays a critical role in coordinating global responses to emerging infectious diseases like MERS-CoV.
-
Future Prospects: Despite the challenges posed by MERS-CoV, there are promising prospects for future research and development. Continued collaboration and investment in research could lead to the development of effective treatments and vaccines, ultimately reducing the impact of this viral respiratory syndrome.
Final Thoughts on MERS
Middle East Respiratory Syndrome (MERS) is a serious viral illness caused by the MERS-CoV virus. First identified in 2012, it primarily spreads through contact with infected dromedary camels and, less commonly, from person to person in healthcare settings. Symptoms range from mild to severe, with older adults and those with chronic conditions at higher risk for severe disease. The mortality rate is high, around 30-40%. Diagnosis relies on RT-PCR testing, and while no specific antiviral treatment exists, supportive care is crucial. Preventive measures include good hygiene practices and avoiding contact with camels. Ongoing research aims to develop effective vaccines and treatments. Public awareness and international coordination remain key in managing and reducing the impact of MERS. By staying informed and following preventive guidelines, we can help protect ourselves and others from this potentially deadly virus.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


