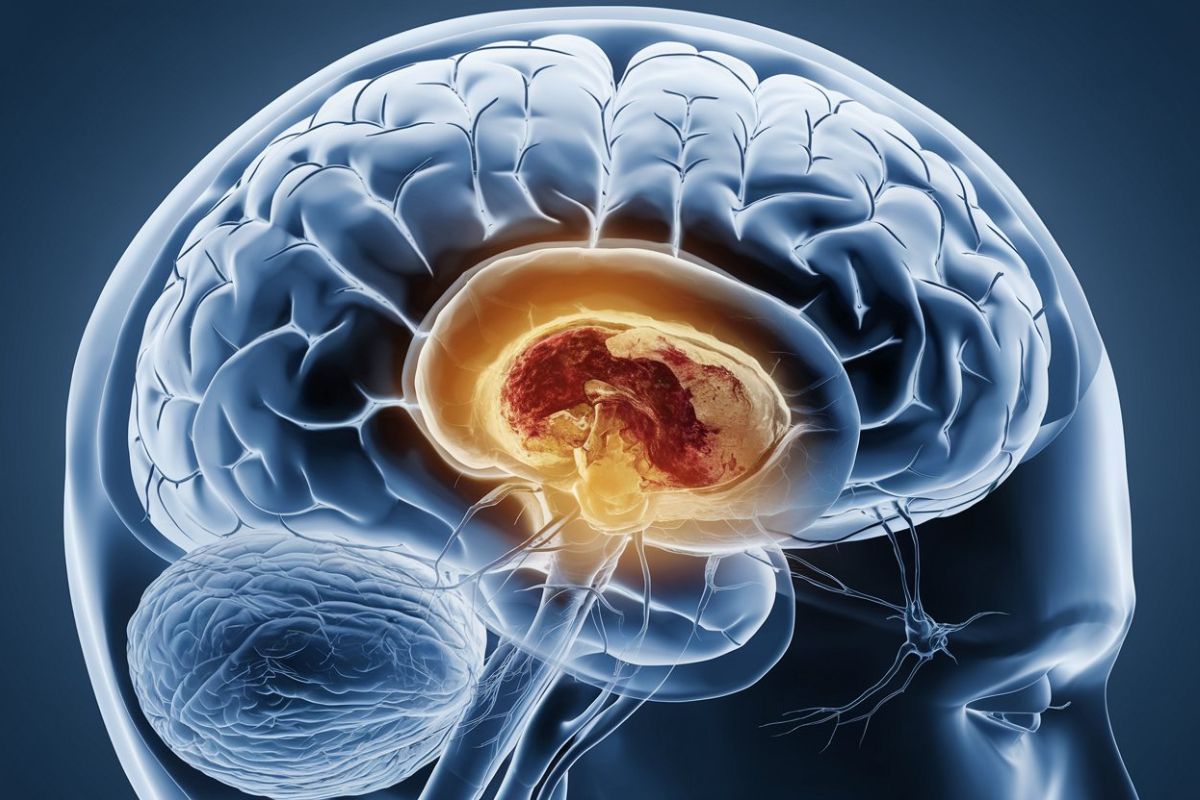
What is Medial Pontine Syndrome? Medial Pontine Syndrome, also known as medial inferior pontine syndrome, is a neurological condition that results from a lesion in the pons, a part of the brainstem. This syndrome primarily causes contralateral hemiplegia, meaning paralysis on the side of the body opposite the lesion. It affects crucial structures like the corticospinal tract and abducens nerve, leading to symptoms such as spastic hemiparesis, strabismus, and sometimes facial nerve involvement. Often caused by occlusion of the basilar artery's paramedian branches, this condition can significantly impact motor and sensory functions. Understanding its clinical presentation, risk factors, and treatment options is vital for effective management.
Key Takeaways:
- Medial Pontine Syndrome causes paralysis on one side of the body and affects eye movements. Understanding its symptoms and causes is crucial for diagnosis and treatment.
- Rehabilitation and a supportive interprofessional team are essential for the recovery of patients with Medial Pontine Syndrome. Understanding the syndrome's clinical presentation and anatomical boundaries is key to effective care.
Understanding Medial Pontine Syndrome
Medial Pontine Syndrome, also known as medial inferior pontine syndrome, is a neurological condition that affects the brainstem. This syndrome can lead to a variety of symptoms due to its impact on different neural pathways and structures. Let's dive into the key facts about this condition.
-
Definition: Medial Pontine Syndrome is associated with contralateral hemiplegia, meaning paralysis on one side of the body opposite to the lesion.
-
Location: The syndrome affects structures at the bottom of the pons, including the corticospinal tract, abducens nerve, and sometimes the facial nerve.
-
Specialty: Neurology is the medical specialty that deals with this condition, focusing on the brainstem and its pathways.
-
Affecting Structures: The corticospinal tract, crucial for motor function, is significantly impacted. The medial lemniscus, which transmits sensory information, is also involved but to a lesser extent.
Key Symptoms and Clinical Presentation
Understanding the symptoms and clinical presentation of Medial Pontine Syndrome is crucial for diagnosis and treatment.
-
Abducens Nerve: The abducens nerve (cranial nerve VI) is affected, leading to strabismus (crossed eyes) due to ipsilateral lateral rectus muscle paralysis. The affected eye looks down and towards the nose.
-
Facial Nerve: Depending on the size of the infarct, the facial nerve can also be involved, leading to facial weakness or paralysis.
-
Contralateral Hemiplegia: The primary presentation is contralateral hemiplegia, meaning paralysis on the opposite side of the body from where the lesion is located.
-
Clinical Presentation: Includes contralateral spastic hemiparesis (weakness) due to the involvement of the corticospinal tract. There is also contralateral PCML (posterior column-medial lemniscus) pathway loss, leading to tactile, vibration, and stereognosis impairments.
-
Strabismus: The abducens nerve lesion localizes the lesion to the inferior pons and results in strabismus, where the affected eye deviates inward and downward.
Causes and Risk Factors
Understanding what causes Medial Pontine Syndrome and the risk factors involved can help in prevention and early diagnosis.
-
Ischemic Injury: Results from occlusion of paramedian branches of the basilar artery, leading to ischemic injury in the affected area.
-
Radiological Findings: Diffusion-weighted magnetic resonance imaging (DW-MRI) can reveal a punctate area of acute ischemia in the right medial pontine mid-tegmentum, indicating a unique pontine stroke syndrome.
-
Unique Syndrome: The medial pontine mid-tegmentum syndrome is characterized by acute combined diplopia (double vision) and unilateral lower extremity sensory abnormality, making it a unique pontine stroke syndrome.
-
Arterial Stroke Territories: Isolated pontine infarcts are common and often associated with well-described syndromes classified based on their specific clinical presentation and arterial stroke territories.
-
Clinical-Radiological Correlation: Studies have shown that large lesions involving the paramedian caudal or middle pons correlate with severe hemiparesis, while lesions of similar size located in the paramedian rostral pons tend to produce dysarthria-clumsy hand syndrome.
-
Hypertension Risk Factor: Hypertension is the single most common and important risk factor for pontine infarction, which often leads to small arterial (lacunar) occlusion or basilar atheromatous branch occlusion.
Prognosis and Treatment
The prognosis and treatment options for Medial Pontine Syndrome can vary based on the severity of the condition and the specific structures affected.
-
Prognosis: The prognosis for patients with pontine infarction is generally fair or good, although residual hemiparesis may remain in patients with initially severe hemiparesis.
-
Anatomical Boundaries: The clinical presentation of a pontine infarction is primarily determined by the anatomical boundaries of the infarcted region within the pons and the blood vessels involved.
-
Tegmental Pontine Syndrome: Can affect various structures including cranial nerve nuclei, medial lemniscus, medial longitudinal fasciculus, respiratory centers, and the pontine reticular formation.
-
Rostral Pontine Syndrome: Obstruction of blood flow in the anterior inferior or superior cerebellar arteries causes rostral pontine syndrome, which presents with ipsilateral facial sensory disturbance and masticator paralysis (trigeminal nuclei).
-
Caudal Pontine Syndrome: Caused by decreased blood flow in the short circumferential or the anterior inferior cerebellar artery. It clinically presents with ipsilateral conjugate gaze palsy and nystagmus (medial longitudinal fasciculus), ipsilateral impaired eye abduction (abducens nucleus), and ipsilateral hemiataxia (middle cerebellar peduncle).
Rehabilitation and Recovery
Rehabilitation plays a crucial role in the recovery process for patients with Medial Pontine Syndrome.
-
Pseudobulbar Palsy: Multiple pontine infarcts primarily affecting the perforating arteries' territories result in pseudobulbar palsy due to the involvement of corticobulbar fibers. This presentation includes severe dysphagia and dysarthria, and some individuals may present with pathological crying or laughing.
-
Clinical Spectrum: The clinical spectrum of pontine infarction can vary widely, ranging from classical crossed syndrome (ipsilateral cranial nerve palsy and contralateral motor and/or sensory impairment) to pure motor hemiparesis or hemiplegia or pure sensory stroke.
-
Epidemiology: Pontine infarction is a significant cause of morbidity and mortality, and understanding its epidemiology is crucial for developing effective prevention strategies. A majority of stroke events and their complications can be prevented with proper care.
-
Treatment Considerations: Treatment considerations for patients with pontine infarction include immediate medical intervention to restore blood flow, manage symptoms, and prevent further complications. Improving care coordination, collaboration, and communication among the interprofessional team is essential for enhancing the delivery of care and improving outcomes.
-
Interprofessional Team: The interprofessional team plays a crucial role in evaluating and treating patients with pontine infarction. This team includes neurologists, radiologists, emergency medicine specialists, physical therapists, occupational therapists, and speech therapists.
-
Rehabilitation Exercises: Rehabilitation exercises are essential for patients recovering from pontine infarction. These exercises can help improve motor function, reduce spasticity, and enhance overall neurological recovery. Physical therapy, occupational therapy, and speech therapy are critical components of the rehabilitation process.
Additional Considerations
There are other important aspects to consider when dealing with Medial Pontine Syndrome.
-
Horizontal Gaze Problems: Lesions in the pons often result in horizontal gaze problems due to the involvement of the parapontine reticular formation and the medial longitudinal fasciculus. These structures are crucial for coordinating eye movements.
-
Dorsal Pontine Syndromes: The dorsal pontine syndromes involve structures such as the sixth nerve nucleus, seventh nerve nucleus, and the medial longitudinal fasciculus. These syndromes can present with complex neurological deficits including diplopia and hemiataxia.
-
Facial Colliculus: The facial colliculus is a structure located in the dorsal pons where the seventh nerve nucleus wraps around the sixth nerve nucleus. This anatomical arrangement is critical for the coordination of facial and eye movements.
-
Clinical-Pathological Correlation: Understanding the clinical-pathological correlation of medial pontine syndrome is essential for accurate diagnosis and treatment. This involves correlating the patient's symptoms with the specific anatomical structures affected by the lesion.
Understanding Medial Pontine Syndrome
Medial Pontine Syndrome is a complex neurological condition that affects the brainstem, specifically the pons. It leads to contralateral hemiplegia, meaning paralysis on one side of the body. Key structures like the corticospinal tract and abducens nerve are impacted, causing symptoms such as strabismus (crossed eyes) and spastic hemiparesis (muscle weakness). The syndrome often results from an ischemic injury due to occlusion of the basilar artery's branches. Hypertension is a significant risk factor. Diagnosis typically involves MRI to identify the infarcted area. Treatment focuses on restoring blood flow and rehabilitation exercises to improve motor function. Understanding the clinical presentation and anatomical basis of this syndrome is crucial for effective management. With proper care, many patients can achieve a fair or good prognosis, although some may experience lasting effects.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


