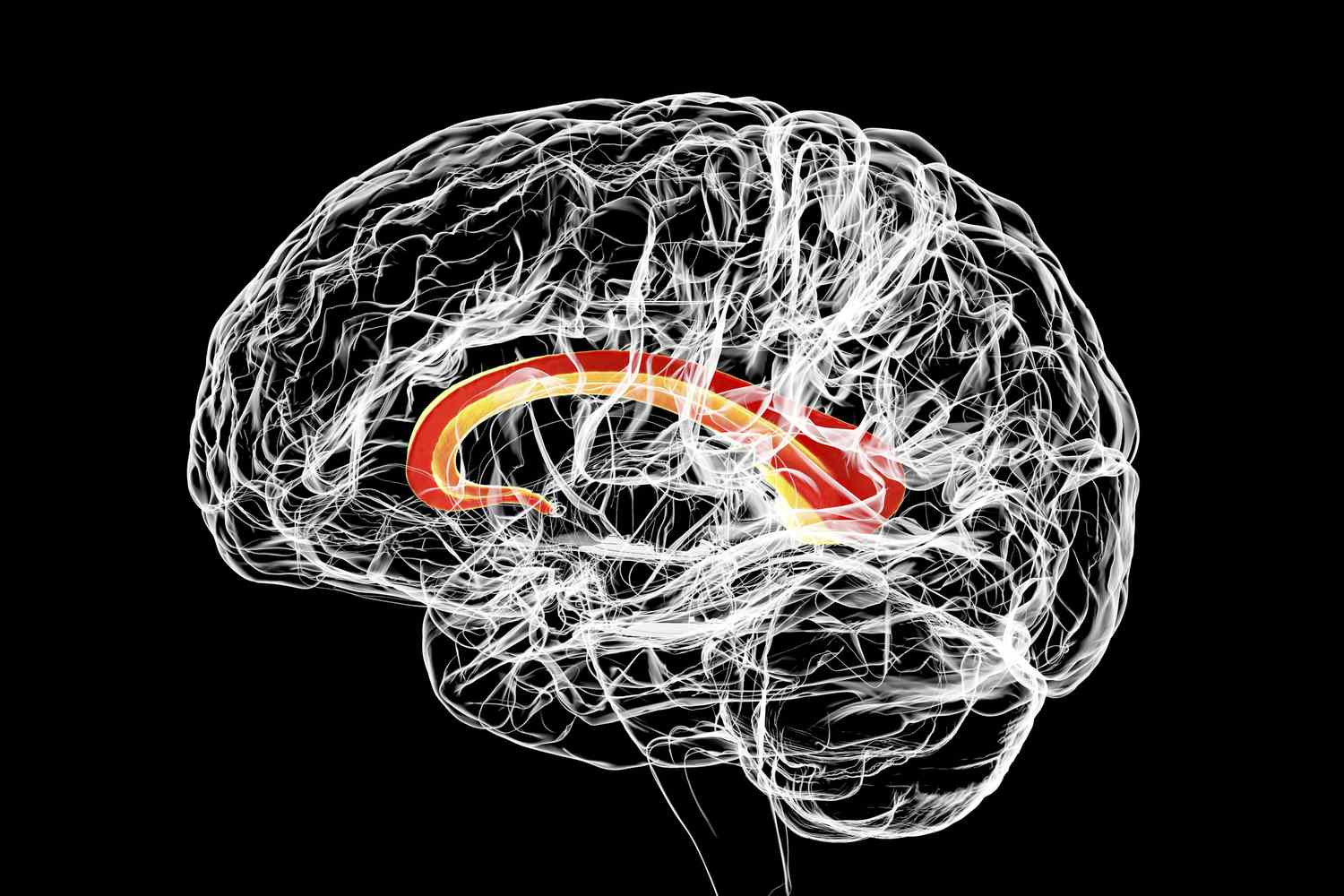
What is Marchiafava-Bignami Disease? Marchiafava-Bignami Disease (MBD) is a rare, serious brain disorder that mainly affects the corpus callosum, the part of the brain connecting the two hemispheres. This condition, first described in 1903 by Italian pathologists Amico Bignami and Ettore Marchiafava, is often linked to chronic alcoholism and malnutrition. Symptoms can vary widely, including altered mental status, speech difficulties, and loss of coordination. Diagnosis is challenging due to its nonspecific symptoms but is primarily confirmed through MRI scans. Treatment focuses on stopping alcohol consumption and addressing nutritional deficiencies, though outcomes can vary significantly.
Key Takeaways:
- Marchiafava-Bignami Disease is a rare neurological disorder linked to chronic alcoholism and malnutrition, causing symptoms like altered mental status and gait abnormalities. Early diagnosis and intervention are crucial for better outcomes.
- MRI is crucial for diagnosing Marchiafava-Bignami Disease, showing symmetric lesions in the corpus callosum. Treatment involves stopping alcohol consumption and addressing nutritional deficiencies, with a poor prognosis in severe cases.
What is Marchiafava-Bignami Disease?
Marchiafava-Bignami Disease (MBD) is a rare neurological disorder that primarily affects the corpus callosum, the part of the brain connecting the two hemispheres. This condition is often linked to chronic alcoholism and malnutrition.
-
Definition and Pathophysiology: MBD involves demyelination and necrosis of the corpus callosum, disrupting signal transmission in the brain.
-
Epidemiology: It's a rare condition, with only around 300 cases reported until 2008, mostly affecting middle-aged or elderly males with a history of chronic alcohol consumption and malnutrition.
-
Symptoms: Symptoms can vary widely, including altered mental status, dementia, spasticity, dysarthria, ataxia, gait abnormalities, seizures, and desynchronization of bilateral symmetric movements.
Causes and Mechanism
Understanding the root causes and mechanisms behind MBD can help in identifying and managing the disease more effectively.
-
Causes: MBD is classically associated with chronic alcoholism, particularly red wine consumption, and can also occur in non-alcoholic individuals with malnutrition or other nutritional deficiencies.
-
Mechanism: The exact mechanism is not fully understood but involves thiamine deficiency, malnutrition, and alcohol-induced brain damage.
-
Thiamine Deficiency: Thiamine depletion impairs myelin synthesis and disrupts metabolic pathways, leading to demyelination and necrosis of the corpus callosum.
Clinical Subtypes and Diagnosis
MBD can present in different forms, making diagnosis challenging but crucial for effective treatment.
-
Clinical Subtypes: MBD can be categorized into Type A, characterized by stupor and coma with extensive corpus callosum involvement, and Type B, presenting with normal or mildly impaired mental status and partial lesions.
-
Diagnosis: Diagnosis is primarily based on MRI, which can visualize lesions in the corpus callosum and other affected brain regions. CT scans may also be used to rule out other conditions.
-
Radiological Findings: MRI is the gold standard for diagnosing MBD, showing symmetric involvement of the corpus callosum, with lesions possibly extending to adjacent subcortical white matter.
Differential Diagnosis and Treatment
Differentiating MBD from other neurological conditions is essential for appropriate treatment.
-
Differential Diagnosis: MBD must be differentiated from conditions like Wernicke’s encephalopathy, neoplastic conditions, and multiple sclerosis.
-
Treatment: There is no specific treatment for MBD. Management is largely supportive, including stopping alcohol consumption and addressing nutritional deficiencies with thiamine and vitamin B complex therapy.
-
Prognosis: The prognosis is generally poor, especially in Type A cases with extensive corpus callosum involvement. Type A has a high mortality rate, while Type B has a better prognosis.
Historical Background and Incidence
The history and incidence of MBD provide context for understanding its development and prevalence.
-
Historical Background: MBD was first described by Marchiafava and Bignami in 1903 in an Italian Chianti drinker, noting necrosis of the corpus callosum in individuals who died from seizures and comas associated with alcohol use disorder.
-
Incidence in Non-Alcoholic Patients: While predominantly associated with chronic alcoholism, MBD can also occur in non-alcoholic individuals with malnutrition or other nutritional deficiencies.
-
Role of Imaging Techniques: Advanced imaging techniques like MRI have significantly improved the diagnosis of MBD, allowing for early detection and intervention.
Symmetry of Lesions and Brain Regions Involved
The specific characteristics of MBD lesions and the brain regions affected are crucial for diagnosis and understanding the disease's impact.
-
Symmetry of Lesions: One distinguishing feature of MBD is the symmetry of lesions in the corpus callosum, helping differentiate it from other demyelinating diseases.
-
Involvement of Adjacent White Matter: Lesions can extend to adjacent subcortical white matter, indicating a broader impact on brain function.
-
Impact on Brain Regions: MBD can affect various brain regions, including the basal ganglia, cerebral lobes, and white matter in the hemisphere, contributing to the severity of symptoms.
Risk Factors and Early Diagnosis
Identifying risk factors and achieving early diagnosis are key to managing MBD effectively.
-
Risk Factors: Primary risk factors include chronic alcoholism, particularly red wine consumption, and malnutrition. Middle-aged or elderly males are most commonly affected.
-
Early Diagnosis: Early diagnosis using advanced imaging techniques like MRI is crucial for improving outcomes, allowing for timely intervention.
-
Treatment Challenges: Treatment is challenging due to variable responses to interventions. Stopping alcohol consumption and addressing nutritional deficiencies are essential components of management.
Prognostic Factors and Differential Diagnosis Considerations
Several factors influence the prognosis of MBD, and careful differential diagnosis is necessary.
-
Prognostic Factors: Factors influencing prognosis include the extent of corpus callosum involvement, the presence of other affected brain regions, and the severity of consciousness disturbances.
-
Differential Diagnosis Considerations: Differential diagnosis involves ruling out other neurological conditions, with the symmetry of lesions in the corpus callosum helping distinguish MBD.
Historical Case Reports and Recent Research Findings
Historical case reports and recent research provide valuable insights into MBD.
-
Historical Case Reports: Historical reports document MBD in individuals with chronic alcohol consumption and malnutrition, highlighting the importance of considering MBD in patients with non-specific neurological symptoms.
-
Recent Research Findings: Recent studies have documented cases in non-alcoholic patients with nutritional deficiencies, emphasizing that alcohol is not the sole cause of MBD.
MRI Findings and Clinical Presentation Variability
MRI findings and the variability in clinical presentation are critical for diagnosing and understanding MBD.
-
MRI Findings: MRI typically shows symmetric involvement of the corpus callosum, with lesions possibly extending to adjacent subcortical white matter and other brain regions.
-
Clinical Presentation Variability: The clinical presentation can vary widely, from mild cognitive impairment to coma, making diagnosis challenging.
Treatment Similarities with Other Conditions
Treatment of MBD often involves similar interventions as those used for other related conditions.
-
Treatment Similarities with Other Conditions: Treatment often involves similar interventions as those used for Wernicke-Korsakoff syndrome or alcohol use disorder, including stopping alcohol consumption and addressing nutritional deficiencies.
-
Nutritional Deficiencies: Other nutritional deficiencies besides thiamine can contribute to MBD, with malnutrition and frequent vomiting increasing the risk.
-
Conclusion: Marchiafava-Bignami Disease is a complex condition requiring a comprehensive approach to diagnosis and management, with early detection and intervention being crucial for improving outcomes.
Final Thoughts on Marchiafava-Bignami Disease
Marchiafava-Bignami Disease (MBD) is a rare but serious neurological disorder. It primarily affects the corpus callosum, leading to demyelination and necrosis. Often linked to chronic alcoholism and malnutrition, MBD presents with a variety of symptoms like altered mental status, dementia, and ataxia. Diagnosis relies heavily on MRI to identify characteristic lesions. Treatment focuses on stopping alcohol consumption and addressing nutritional deficiencies, particularly thiamine. Prognosis varies; some patients improve with treatment, while others face long-term disability or even death. Early diagnosis and intervention are crucial for better outcomes. Understanding MBD's complexities helps in managing this challenging condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.