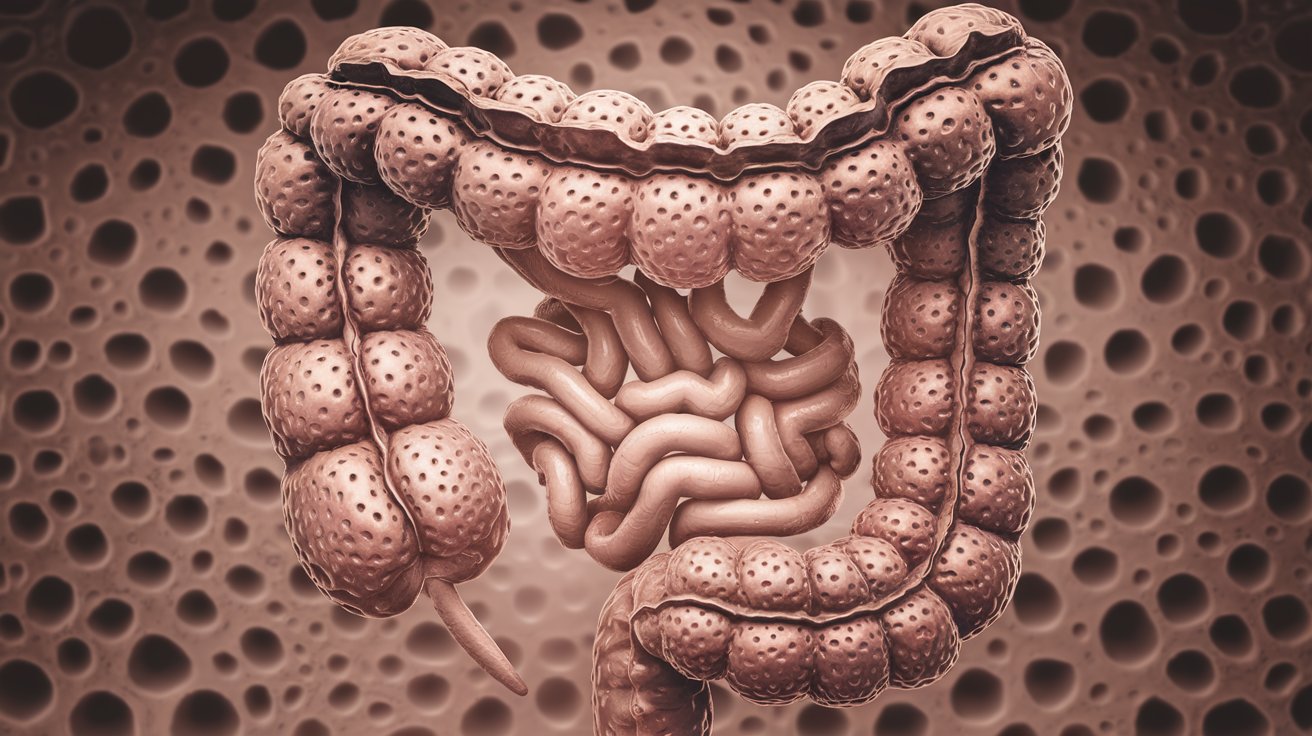
Hereditary Nonpolyposis Colorectal Cancer (HNPCC), also known as Lynch syndrome, is a genetic condition that greatly increases the risk of colorectal cancer and other cancers. Named after Dr. Henry T. Lynch, who first described it in 1966, this syndrome is caused by mutations in DNA mismatch repair (MMR) genes like MLH1, MSH2, MSH6, PMS2, and EPCAM. These genes are vital for fixing DNA errors during cell division. Individuals with HNPCC face a 40-70% lifetime risk of colorectal cancer, often diagnosed around age 44, much earlier than the general population. Besides colorectal cancer, HNPCC also raises the risk of endometrial, ovarian, gastric, and other cancers. Regular screenings and genetic counseling are crucial for managing this condition.
Understanding Hereditary Nonpolyposis Colorectal Cancer
Hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome, is a genetic disorder that significantly increases the risk of developing colorectal cancer and other types of cancer. Let's dive into some essential facts about this condition.
-
Definition and Synonyms: HNPCC is often referred to as Lynch syndrome, named after Henry T. Lynch, who first described the condition in 1966. The term "HNPCC" was coined in 1985 by Lynch himself.
-
Genetic Basis: HNPCC is caused by germline mutations in one of the DNA mismatch repair (MMR) genes, which include MLH1, MSH2, MSH6, PMS2, and EPCAM. These genes are crucial for repairing DNA mismatches that occur during DNA replication.
Increased Cancer Risks
Individuals with HNPCC face a higher risk of developing various cancers, not just colorectal cancer. Here are some of the key risks associated with this syndrome.
-
Risk of Colorectal Cancer: Individuals with HNPCC have a significantly higher risk of developing colorectal cancer (CRC). The lifetime risk of CRC in individuals with HNPCC is estimated to be between 40% and 70%, which is much higher than the general population's risk of about 5-6%.
-
Early Onset: Colorectal cancers in individuals with HNPCC typically occur at a younger age compared to the general population. The average age of diagnosis is around 44 years, whereas in the general population, it is about 64 years.
-
Extracolonic Manifestations: HNPCC is associated with an increased risk of various extracolonic cancers, including endometrial cancer, ovarian cancer, gastric cancer, small bowel cancer, hepatobiliary tract cancer, upper urinary tract cancer, and brain cancer (glioma).
-
Endometrial Cancer Risk: Endometrial cancer is the second most common cancer associated with HNPCC. The risk of endometrial cancer in individuals with HNPCC is significantly higher than in the general population.
-
Ovarian Cancer Risk: Ovarian cancer is another common extracolonic manifestation of HNPCC. The risk of ovarian cancer in individuals with HNPCC is also elevated compared to the general population.
-
Gastric Cancer Risk: Gastric cancer (stomach cancer) is another type of cancer that individuals with HNPCC are at an increased risk for. The risk is particularly high in the proximal part of the stomach.
-
Small Bowel Cancer Risk: Small bowel cancer is another extracolonic manifestation associated with HNPCC. The risk is higher in individuals with this syndrome compared to the general population.
-
Hepatobiliary Tract Cancer Risk: The hepatobiliary tract, which includes the liver and bile ducts, is also at an increased risk for cancer in individuals with HNPCC.
-
Upper Urinary Tract Cancer Risk: Upper urinary tract cancers, including those in the renal pelvis and ureter, are more common in individuals with HNPCC.
-
Brain Cancer Risk: Gliomas, a type of brain cancer, are also associated with an increased risk in individuals with HNPCC.
-
Skin Cancer Risk: Sebaceous neoplasms, a type of skin cancer, are more common in individuals with HNPCC.
Prevalence and Genetic Factors
Understanding the prevalence and genetic factors of HNPCC can help in identifying and managing the condition more effectively.
-
Prevalence: The prevalence of Lynch syndrome-causing mutations in the general population is estimated to be around 1 in 279 individuals, or approximately 0.35%.
-
Founder Mutations: Certain populations have a higher prevalence of founder mutations, including French Canadians, Icelanders, African Americans, and Ashkenazi Jews.
-
CRC Risk in General Population: The lifetime risk of CRC in the general population is about 5-6%, but this risk is significantly higher in individuals with HNPCC.
Diagnostic Criteria and Guidelines
Proper diagnosis of HNPCC involves specific criteria and guidelines to ensure accurate identification and management.
-
Diagnostic Criteria: The diagnosis of HNPCC is typically made using the Amsterdam criteria, which include three or more relatives with CRC, one of whom is a first-degree relative of the other two, and at least two successive generations affected.
-
Bethesda Guidelines: The Bethesda guidelines provide additional criteria for diagnosing HNPCC, including the presence of microsatellite instability (MSI) in tumors, which is a hallmark of HNPCC.
-
Microsatellite Instability (MSI): MSI is a condition where there is an increased frequency of mutations in microsatellites, which are short DNA sequences that repeat. This is a key feature of HNPCC.
-
Family History: A thorough family history is crucial for diagnosing HNPCC. The family history should include information about the age of cancer onset, the pattern of multiple primary cancers, and the generation-to-generation transmission of cancers.
-
Genealogic and Medical Information: Ideally, genealogic and medical information should include three generations: the proband, parents, aunts and uncles, both sets of grandparents, and progeny.
-
Reduced Penetrance: There is a possibility of reduced penetrance in cancer-prone lineages, meaning that not all individuals with the genetic mutation will develop cancer.
Surveillance and Management
Regular surveillance and proper management are essential for individuals with HNPCC to detect and treat cancers early.
-
Surveillance Recommendations: Regular surveillance is essential for individuals with HNPCC. This includes regular colonoscopies, endometrial biopsies, and other screenings to detect cancers early.
-
Management Options: The management of HNPCC involves a multidisciplinary approach. This includes genetic counseling, regular surveillance, and surgical interventions when necessary.
-
Genetic Testing: Genetic testing is available for HNPCC. Testing for mutations in the MMR genes can confirm the diagnosis and help guide management decisions.
-
Prognosis: The prognosis for individuals with HNPCC varies depending on the type and stage of cancer at diagnosis. Early detection through regular surveillance can improve outcomes.
Support and Awareness
Support and awareness are crucial for individuals with HNPCC and their families. Several organizations and initiatives help spread knowledge and provide resources.
-
Non-Profit Organizations: There are several non-profit organizations providing information and support for individuals with HNPCC, including Lynch Syndrome International, AliveAndKickn, Lynch Syndrome UK, and Bowel Cancer UK.
-
National Awareness Day: In the US, National Lynch Syndrome Awareness Day is observed on March 22.
Differential Diagnosis and Molecular Genetics
Understanding the differential diagnosis and molecular genetics of HNPCC is crucial for accurate diagnosis and treatment.
-
Differential Diagnosis: The differential diagnosis of HNPCC includes other hereditary CRC syndromes such as familial adenomatous polyposis (FAP), Peutz-Jeghers syndrome, and mixed adenomatous hamartomatous syndrome.
-
Molecular Genetics: Understanding the molecular genetics of HNPCC is crucial for diagnosis and management. This includes the role of MMR genes and the mechanisms of MSI.
Key Takeaways on HNPCC
Hereditary nonpolyposis colorectal cancer (HNPCC), or Lynch syndrome, is a genetic disorder that greatly increases the risk of colorectal and other cancers. Caused by mutations in MMR genes like MLH1, MSH2, MSH6, PMS2, and EPCAM, it leads to a higher lifetime risk of colorectal cancer, often diagnosed at a younger age. Besides colorectal cancer, individuals with HNPCC face elevated risks for endometrial, ovarian, gastric, small bowel, hepatobiliary tract, upper urinary tract, and brain cancers. Regular surveillance, genetic testing, and a thorough family history are crucial for managing this condition. Understanding the genetic basis and implementing early detection strategies can significantly improve outcomes. Non-profit organizations and awareness days play a vital role in supporting affected individuals. With proper management and vigilance, those with HNPCC can lead healthier lives despite the increased cancer risks.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


