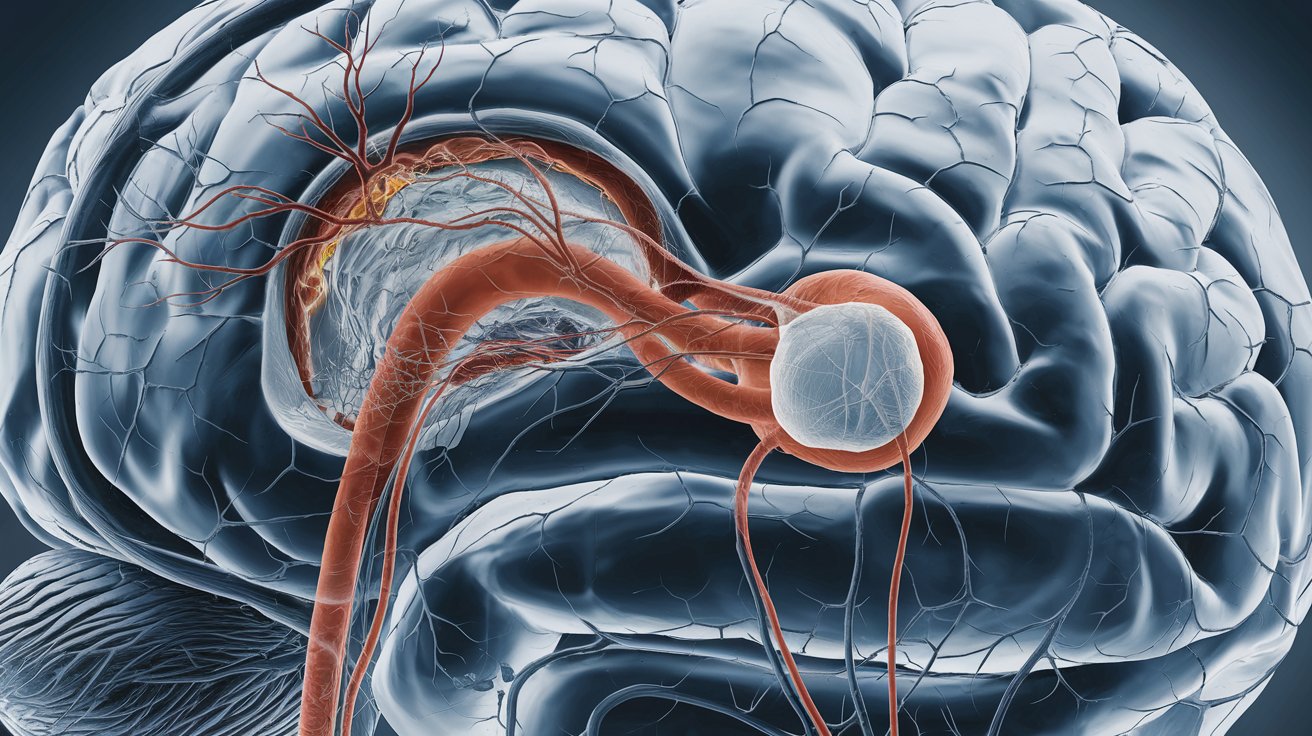
Congenital Arteriovenous Shunt is a rare condition where abnormal connections form between arteries and veins, bypassing the capillary system. This can lead to various complications, including heart failure, bleeding, and tissue damage. Understanding congenital arteriovenous shunt is crucial for early diagnosis and effective treatment. These shunts can occur anywhere in the body but are most commonly found in the brain, lungs, and liver. Symptoms vary widely depending on the location and size of the shunt. Early detection often involves imaging techniques like MRI or CT scans. Treatment options range from medication to surgical intervention. Knowing the facts about this condition can help manage it better and improve quality of life.
Key Takeaways:
- Congenital arteriovenous shunts are rare connections between arteries and veins present at birth, causing varied symptoms. Early diagnosis and monitoring are crucial for effective management and treatment options include surgery, embolization, or medication.
- Living with a congenital arteriovenous shunt involves regular medical care, lifestyle adjustments, and emotional support. Ongoing research aims to improve understanding and treatment, offering hope for future minimally invasive treatments and potential stem cell therapies.
What is a Congenital Arteriovenous Shunt?
A congenital arteriovenous shunt is a rare condition where abnormal connections form between arteries and veins during fetal development. These connections bypass the capillary system, causing various health issues. Let's dive into some fascinating facts about this condition.
-
Congenital arteriovenous shunts are present at birth. They develop during fetal growth, leading to abnormal blood flow patterns from the start of life.
-
These shunts can occur anywhere in the body. They are most commonly found in the brain, lungs, and liver but can appear in other organs and tissues.
-
Symptoms vary widely. Depending on the location and size of the shunt, symptoms can range from mild to severe, including headaches, seizures, or heart failure.
-
Diagnosis often involves imaging techniques. Doctors use MRI, CT scans, and angiography to visualize the abnormal blood vessels.
-
Some shunts may remain asymptomatic. In certain cases, individuals may live without noticeable symptoms, only discovering the condition incidentally.
Causes and Risk Factors
Understanding the causes and risk factors can help in early detection and management of congenital arteriovenous shunts.
-
Genetic factors play a role. Some cases are linked to genetic mutations, though the exact cause is often unknown.
-
Family history increases risk. If a close relative has a congenital arteriovenous shunt, the likelihood of developing one is higher.
-
Certain syndromes are associated with shunts. Conditions like Hereditary Hemorrhagic Telangiectasia (HHT) often involve multiple arteriovenous malformations.
-
Environmental factors during pregnancy may contribute. Exposure to certain toxins or infections during fetal development can increase the risk.
-
More common in males. Studies show a slightly higher prevalence in males compared to females.
Symptoms and Complications
The symptoms and potential complications of congenital arteriovenous shunts can significantly impact quality of life.
-
Headaches are a common symptom. Especially with brain shunts, persistent headaches can be a primary complaint.
-
Seizures may occur. Abnormal electrical activity in the brain caused by shunts can lead to seizures.
-
Heart failure is a serious risk. Large shunts can overload the heart, leading to heart failure if untreated.
-
Pulmonary hypertension can develop. Shunts in the lungs can cause high blood pressure in the pulmonary arteries.
-
Bleeding risks increase. Fragile abnormal vessels are prone to rupture, leading to potentially life-threatening bleeding.
Diagnosis and Treatment
Early diagnosis and appropriate treatment are crucial for managing congenital arteriovenous shunts effectively.
-
Ultrasound is often the first diagnostic tool. Especially in newborns, ultrasound can help detect abnormal blood flow.
-
MRI provides detailed images. It helps in assessing the extent and exact location of the shunt.
-
CT scans offer quick results. They are useful in emergency situations to quickly identify shunts.
-
Angiography is the gold standard. This invasive procedure provides a detailed map of the blood vessels involved.
-
Treatment options vary. Depending on the shunt's size and location, treatments can include surgery, embolization, or medication.
Living with a Congenital Arteriovenous Shunt
Managing life with a congenital arteriovenous shunt involves regular medical care and lifestyle adjustments.
-
Regular monitoring is essential. Frequent check-ups help track the shunt's progression and effectiveness of treatments.
-
Lifestyle changes can help. Avoiding activities that increase blood pressure or risk of injury can reduce complications.
-
Support groups provide emotional help. Connecting with others facing similar challenges can offer valuable support.
-
Physical therapy may be beneficial. For those with mobility issues due to shunts, physical therapy can improve quality of life.
-
Medication management is crucial. Some patients may need medications to control symptoms or prevent complications.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of congenital arteriovenous shunts.
-
Genetic research is expanding. Scientists are identifying more genetic mutations linked to shunts, which could lead to targeted therapies.
-
New imaging techniques are emerging. Advances in imaging technology are making it easier to diagnose and monitor shunts.
-
Minimally invasive treatments are being developed. New procedures aim to reduce risks and recovery times for patients.
-
Stem cell research shows promise. Early studies suggest stem cells could help repair damaged blood vessels.
-
Patient registries are growing. Collecting data from patients worldwide helps researchers identify patterns and improve treatments.
Final Thoughts on Congenital Arteriovenous Shunt
Understanding congenital arteriovenous shunt is crucial for grasping its impact on health. These abnormal connections between arteries and veins can lead to serious complications if not managed properly. Early detection and treatment are key to preventing issues like heart failure, hemorrhages, and other vascular problems.
Medical advancements have made it possible to diagnose and treat these shunts more effectively than ever before. From imaging techniques to surgical interventions, options are available to improve patient outcomes.
If you or someone you know is affected by this condition, consulting with a healthcare professional is essential. They can provide personalized advice and treatment plans tailored to individual needs.
Staying informed and proactive can make a significant difference in managing congenital arteriovenous shunts, ensuring a better quality of life for those affected.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


