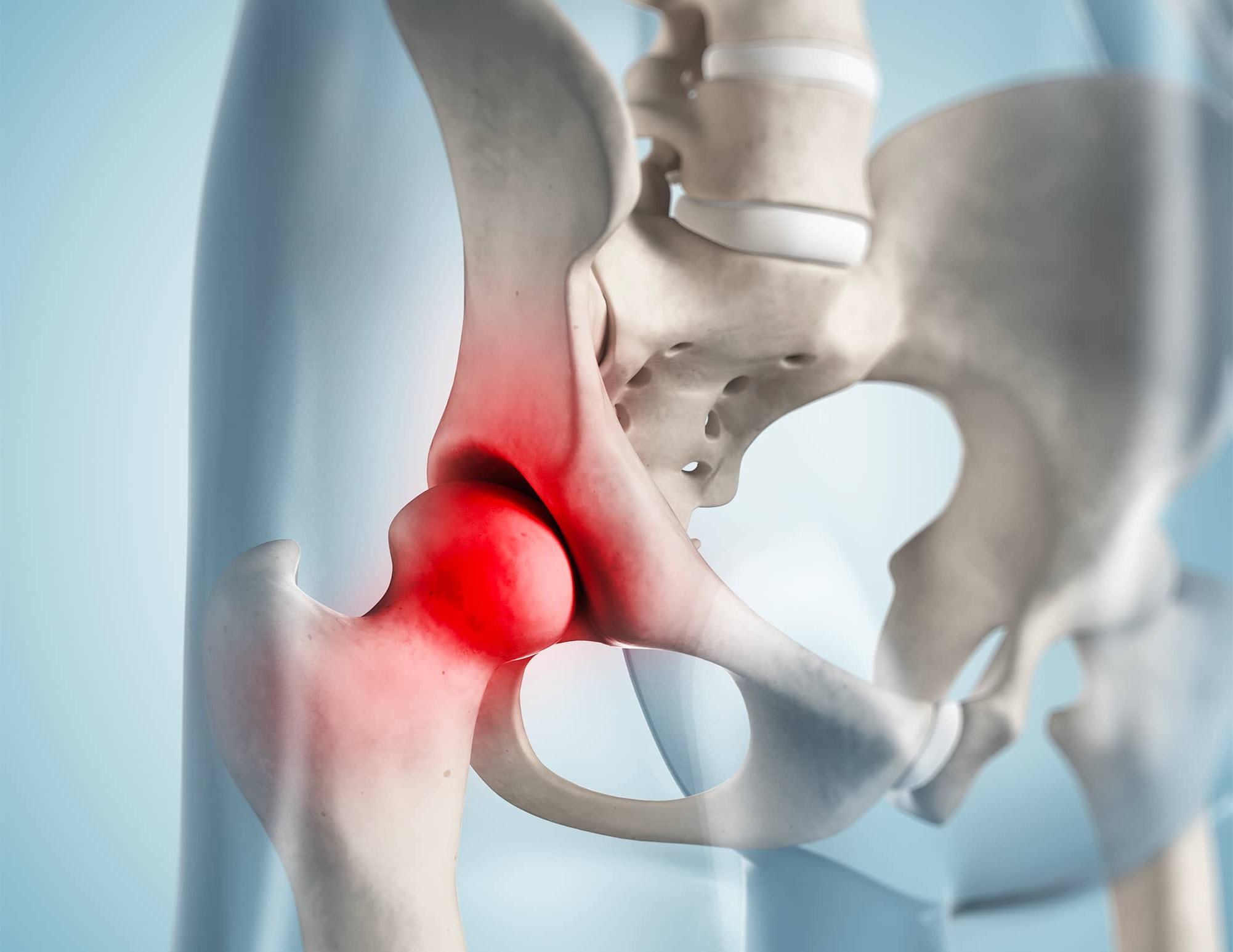
What is Chondromatosis? Chondromatosis, specifically synovial chondromatosis, is a rare, non-cancerous condition where cartilage nodules form within the synovial membrane of joints, tendon sheaths, and bursae. These nodules can cause joint pain, swelling, and stiffness, often leading to significant discomfort and disability. The condition primarily affects men between 30 and 60 years old, with the knee being the most commonly impacted joint. While the exact cause remains unknown, it can be classified as either primary, occurring without underlying joint issues, or secondary, associated with joint degeneration or trauma. Treatment usually involves surgical removal of the loose bodies and synovectomy to alleviate symptoms and prevent recurrence.
Key Takeaways:
- Chondromatosis is a rare joint condition that causes cartilaginous nodules, leading to joint pain and stiffness. Surgery is the main treatment, and long-term monitoring is crucial for recurrence.
- Understanding the types, symptoms, and treatment options for chondromatosis is essential for early diagnosis and effective management. Collaboration between healthcare professionals and patient education are key for comprehensive care.
What is Chondromatosis?
Chondromatosis, specifically synovial chondromatosis, is a rare condition affecting the joints. It involves the formation of cartilaginous nodules within the synovial membrane. These nodules can cause significant joint issues.
-
Definition and Etiology: Synovial chondromatosis is a metaplastic condition where the synovial membrane turns into cartilage and bone, creating loose bodies in the joint space.
-
Incidence and Prevalence: The exact number of cases is unknown, but in England, it's reported as 1.8 per million people annually. It's a rare joint disorder.
-
Demographics: Men are more often affected, with a male-to-female ratio of up to 4:1. It usually strikes those aged 30 to 60, with the knee being the most commonly affected joint.
Types of Synovial Chondromatosis
There are two main types: primary and secondary. Understanding the differences can help in diagnosing and treating the condition.
- Primary vs. Secondary Synovial Chondromatosis: Primary occurs without any underlying joint issues, often in younger people. Secondary is linked to joint degeneration or trauma, more common in older individuals.
Symptoms and Clinical Presentation
Recognizing the symptoms is crucial for early diagnosis and treatment. Patients often experience joint pain and other discomforts.
-
Clinical Presentation: Symptoms include joint pain, swelling, and stiffness. Crepitus, a grinding sensation, can occur due to loose bodies in the joint.
-
Radiological Findings: X-rays show multiple loose, radio-opaque chondroid bodies of different sizes within the joint. MRI scans help when X-rays are inconclusive.
Diagnosis and Histopathology
Accurate diagnosis involves radiological imaging and histopathological examination. These methods help differentiate between primary and secondary forms.
- Histopathological Characteristics: Primary synovial chondromatosis shows a disorganized pattern with many binucleate chondrocytes and patchy calcification. Secondary features fragments of articular cartilage or bone in the loose bodies.
Treatment Options
Treatment usually involves surgery to remove loose bodies and possibly the inflamed synovial membrane. Different surgical approaches are used based on the joint and extent of the disease.
-
Treatment Options: Surgery is the main treatment, often involving the removal of loose bodies and synovectomy. Arthroscopic surgery is commonly used.
-
Surgical Approaches: The approach varies depending on the joint and disease extent. Sometimes, an open biopsy is necessary.
Recurrence and Complications
Even after treatment, synovial chondromatosis can recur. Long-term follow-up is essential to monitor and manage potential complications.
-
Recurrence Rates: Recurrence varies between 0% and 17% in short-term follow-ups. Long-term monitoring is crucial.
-
Complications: The condition can cause severe joint disability and dysfunction. It may also form a swollen, tender mass, mimicking other conditions.
Differential Diagnosis
Due to its rarity and nonspecific symptoms, synovial chondromatosis can be challenging to diagnose. Several other conditions need to be ruled out.
- Differential Diagnosis: Conditions to consider include ganglion cysts, giant cell tumors, calcifying aponeurotic fibroma, crystal arthropathy, inflammatory arthritis, and degenerative joint diseases.
Age and Bilateral Involvement
Understanding the typical age of onset and the possibility of bilateral involvement can aid in diagnosis and treatment planning.
-
Age of Onset: It usually presents in the third to fifth decade of life but can rarely occur in children and adolescents.
-
Bilateral Involvement: Bilateral cases are reported in about 10% of patients.
Extra-Articular Presentation
Though rare, synovial chondromatosis can present outside the joints, affecting synovial-lined bursal tissue or tenosynovium.
- Extra-Articular Presentation: Known as tenosynovial or bursal chondromatosis, it involves cartilaginous nodules forming outside the joints.
Milgram's Classification
Milgram's classification helps in understanding the stages of synovial chondromatosis, aiding in diagnosis and treatment planning.
- Milgram's Classification: It includes three phases: active (no loose bodies), transition (active lesions and loose bodies), and major (multiple free osteochondral bodies).
Common Symptoms
Recognizing common symptoms can lead to early diagnosis and treatment, improving patient outcomes.
- Clinical Symptoms: Joint pain, swelling, stiffness, and crepitus are common. A painless tumor may become tender under pressure.
Diagnostic Challenges
Due to its rarity, diagnosing synovial chondromatosis can be difficult. A thorough evaluation is necessary.
- Diagnostic Challenges: Accurate diagnosis requires clinical evaluation, radiological imaging, and histopathological examination.
Management in Resource-Limited Settings
Even in resource-limited settings, synovial chondromatosis can be managed effectively with careful planning and resource use.
- Management in Resource-Limited Settings: Thoughtful application of resources and surgical principles can ensure safe and effective management.
Importance of Histopathological Examination
Histopathological examination is crucial for confirming the diagnosis and differentiating between primary and secondary forms.
- Histopathological Examination: Essential for confirming the diagnosis and differentiating between primary and secondary forms based on loose body characteristics.
Surgical Intervention
Surgery is key to relieving symptoms and preventing joint destruction. It involves removing loose bodies and addressing the synovial membrane pathology.
- Surgical Intervention: Crucial for alleviating symptoms and preventing joint destruction. It involves removing loose bodies and performing synovectomy.
Arthroscopic Surgery
Arthroscopic surgery is a preferred method due to its minimally invasive nature and ability to directly visualize the joint space.
- Arthroscopic Surgery: Preferred for its minimally invasive nature and direct visualization of the joint space.
Postoperative Care
Proper postoperative care ensures healing and prevents recurrence. Physical therapy may be needed to restore joint function.
- Postoperative Care: Critical for healing and preventing recurrence. Physical therapy may be required to restore joint mobility and function.
Follow-Up
Long-term follow-up is essential to monitor for recurrence and assess treatment effectiveness.
- Follow-Up: Essential for monitoring recurrence and assessing treatment effectiveness. Regular check-ups help identify complications early.
Interprofessional Team Approach
Managing synovial chondromatosis effectively requires collaboration between various healthcare professionals.
- Interprofessional Team Approach: Collaboration between orthopedic surgeons, radiologists, pathologists, and physical therapists ensures comprehensive care.
Patient Education
Educating patients about their condition, symptoms, and treatment options helps them manage their condition better and prevent complications.
- Patient Education: Vital for managing the condition. Patients need to understand symptoms and treatment options to manage their condition and prevent complications.
Complications in Resource-Limited Settings
Managing synovial chondromatosis in resource-limited settings can be challenging, but thoughtful application of resources can ensure effective management.
- Complications in Resource-Limited Settings: Thoughtful application of resources and surgical principles can ensure safe and effective management.
Case Reports
Case reports provide valuable insights into the clinical presentation, diagnosis, and management of synovial chondromatosis.
- Case Reports: Highlight the variability in presentation and the need for a comprehensive diagnostic approach.
Recurrence Prevention
Preventing recurrence is crucial for long-term management. Regular follow-up and physical therapy can help.
- Recurrence Prevention: Achieved through regular follow-up, physical therapy, and addressing any underlying joint pathology.
Future Research Directions
Future research aims to better understand the etiology, develop more effective diagnostic tools, and explore new treatment modalities.
- Future Research Directions: Focus on understanding the etiology, developing better diagnostic tools, and exploring new treatment options to improve patient outcomes.
Final Thoughts on Chondromatosis
Chondromatosis, particularly synovial chondromatosis, is a rare but impactful joint condition. It involves the formation of cartilaginous nodules within the synovial membrane, leading to pain, swelling, and stiffness. Though it primarily affects men between 30 and 60, anyone can develop it. Diagnosis often requires X-rays and MRI scans, with histopathological examination confirming the type. Treatment usually involves surgical removal of loose bodies and synovectomy. Recurrence rates vary, so long-term follow-up is crucial. Managing this condition effectively often requires a team approach, including orthopedic surgeons, radiologists, and physical therapists. Patient education is key to understanding symptoms and treatment options. Future research aims to improve diagnostic tools and treatment methods. Understanding these facts can help healthcare providers better diagnose and manage chondromatosis, ultimately improving patient outcomes.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.