What is Northern Epilepsy Syndrome? Northern Epilepsy Syndrome (NES), also known as Progressive Epilepsy with Mental Retardation (EPMR), is a rare, severe neurological disorder. It primarily affects people in Finland, making it a Finnish heritage disease. NES is caused by mutations in the CLN8 gene, inherited in an autosomal recessive manner. Symptoms usually start in early childhood with recurrent seizures and progressively worsen, leading to mental deterioration and physical impairment. By adulthood, individuals often require assistance for daily living. Despite its severity, NES remains relatively unknown outside Finland. Understanding NES involves exploring its genetic roots, clinical features, and historical context.
Key Takeaways:
- Northern Epilepsy Syndrome (NES) is a rare neurological disorder predominantly found in Finland, causing seizures and mental decline. It is associated with mutations in the CLN8 gene and has a high carrier rate among people of Finnish descent.
- Understanding and managing NES is crucial. Genetic testing, MRI, and EEG are used for diagnosis, while treatment focuses on managing symptoms. Future directions include improving access to treatments and educating about epilepsy to reduce stigma.
What is Northern Epilepsy Syndrome?
Northern Epilepsy Syndrome (NES) is a rare and severe neurological disorder. It is also known as Progressive Epilepsy with Mental Retardation (EPMR). This condition affects the brain, leading to seizures and mental decline.
-
Definition and Synonyms: NES is a subtype of neuronal ceroid lipofuscinosis (NCL), a group of inherited lysosomal storage disorders. It is also known as Progressive Epilepsy with Mental Retardation (EPMR) and is specifically associated with mutations in the CLN8 gene.
-
Geographical Distribution: NES is predominantly found in Finland, where it is considered a Finnish heritage disease. The condition has been reported only in Finland, making it a unique example of a geographically localized genetic disorder.
Genetic Causes and Prevalence
Understanding the genetic roots and how common NES is can help in grasping its impact.
-
Genetic Causes: The disease is caused by an autosomal recessive mutation in the telomeric region of the short arm of chromosome 8. The most common missense mutation occurs at codon 24, where a glycine replaces an arginine (Arg24Gly). This mutation leads to the creation of a new protein, CLN8, which alters the lipid content of the brain.
-
Prevalence: The prevalence of NES is relatively low, with approximately 1 in every 135 people of Finnish descent being a carrier of the mutation. This high carrier rate is due to the founder effect and relative isolation of the Finnish population.
Clinical Presentation and Symptoms
NES manifests in specific ways, primarily through seizures and mental decline.
-
Clinical Presentation: The clinical presentation of NES typically begins in early childhood, with recurrent seizures occurring between the ages of 5 to 10. These seizures can be classified as tonic-clonic or partial seizures and may last up to 15 minutes. The initial seizure frequency is usually one to two times per month, but it increases during puberty to one to two times per week.
-
Seizure Characteristics: Seizures in NES are characterized by muscle rigidity, convulsions, and loss of consciousness. The seizures often involve focal areas of the brain, which can lead to focal seizures with impaired awareness and occipital phenomenology. Unlike other forms of NCL, myoclonus (jerky involuntary movements) is not a typical feature of NES, although some patients may develop myoclonias on certain medications like lamotrigine.
-
Mental Deterioration: As the disease progresses, there is a noticeable decline in intellectual capacity. During adolescence, mental function rapidly deteriorates, leading to a lack of coordination, failure to complete education, and fine motor activities. In rare cases, some patients may experience loss of vision.
-
Adulthood Symptoms: By adulthood, the seizure frequency decreases to four to six seizures per year. However, the mental and physical capabilities of the individual are severely impaired, making them incapable of living without assistance due to total mental degradation. The life expectancy for individuals with NES is at least 50 years, which is shorter than the average worldwide age of 70.
Pathophysiology and Diagnosis
The underlying mechanisms and how NES is diagnosed are crucial for understanding the disease.
-
Pathophysiology: The pathophysiology of NES involves the accumulation of transmembrane protein in the brain tissue. This protein, CLN8, is linked to the accumulation of subunit c of mitochondrial ATP synthase and small amounts of sphingolipid activator proteins in neurons. The β-amyloid peptide, involved in Alzheimer's disease, is also seen in this protein accumulation.
-
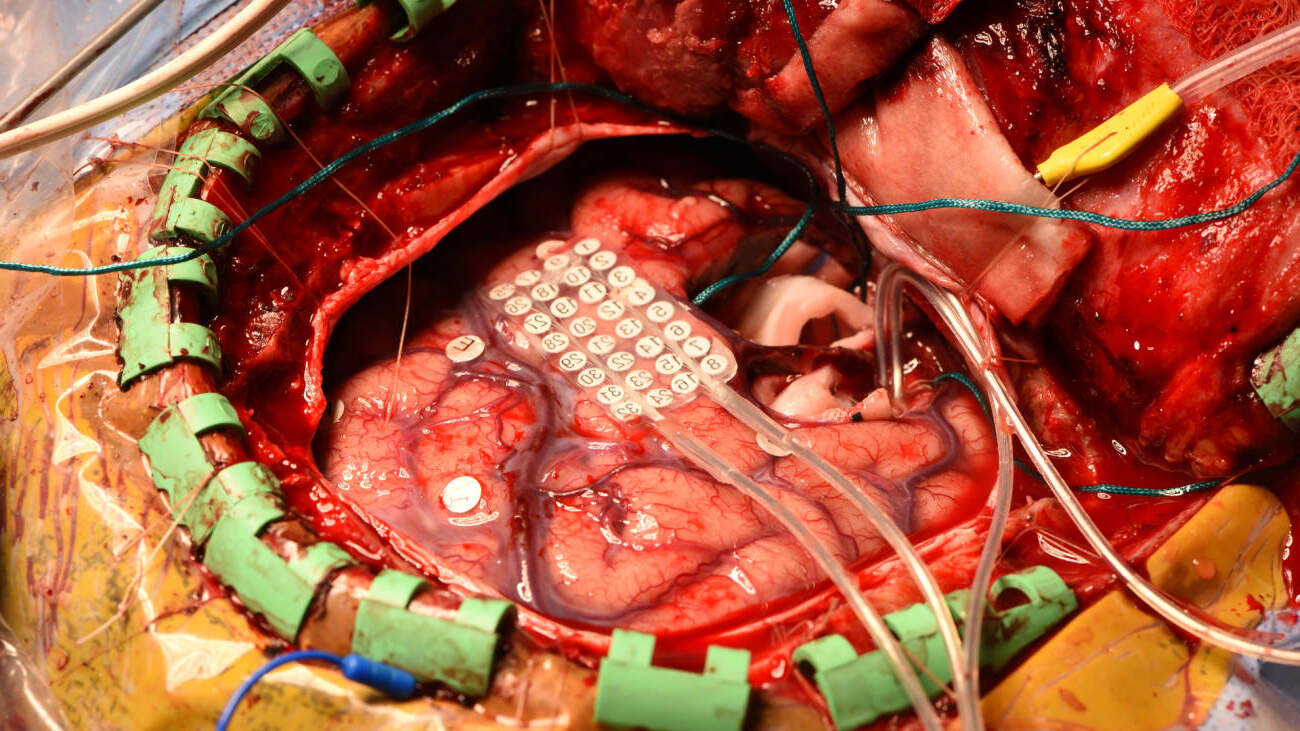
Diagnosis: Diagnosis of NES is primarily based on genetic testing. A patient's DNA is sequenced from a blood sample using the ABI Big Dye Terminator v.3.0 kit. The DNA sequence can be run with CLN8 Sanger sequencing or CLN8 Targeted Familial Mutations, whether it involves single, double, or triple exon sequencing. Preliminary evidence of the disease can also be detected by means of MRI and EEG, which identify lipid content anomalies in the brain.
Historical Context and Ancient Documentation
Epilepsy has a long history, often misunderstood and stigmatized.
-
Historical Context: Epilepsy has been historically associated with evil spirits and mystery. In ancient times, epilepsy was often attributed to demonic possession or divine wrath. This stigma has persisted, with people with epilepsy facing discrimination and social isolation throughout history. Even in modern times, epilepsy carries significant social stigma, impacting the quality of life for individuals with the condition and their families.
-
Ancient Documentation: Evidence of epilepsy dates back to ancient civilizations. The Edwin Smith Surgical Papyrus from Egypt (circa 1700 BC) describes several accounts of epilepsy, including a case where direct stimulation of the brain resulted in a physiologic response. In contrast, the Mesopotamians believed seizures were caused by spirits and gods. Documentation of epilepsy is also found in Chinese texts, such as The Yellow Emperor’s Classic of Internal Medicine, which outlined generalized seizures.
Current Understanding and Global Prevalence
Modern science has shed light on epilepsy, making it less mysterious but still challenging.
-
Current Understanding: Despite the historical misconceptions, epilepsy is now understood to be a chronic noncommunicable disease of the brain characterized by recurrent seizures. Seizures result from excessive electrical discharges in a group of brain cells and can vary in frequency and severity. Epilepsy affects around 50 million people worldwide and is one of the world’s oldest recognized conditions.
-
Global Prevalence: Epilepsy is a global health issue, affecting both sexes and all ages. The prevalence and incidence of epilepsy are slightly higher in men compared to women, and the disease tends to peak in the elderly due to higher frequencies of stroke, neurodegenerative diseases, and tumors in this age group.
Seizure Types and Etiology
Different types of seizures and their causes help in understanding NES better.
-
Seizure Types: Seizures can be classified into focal and generalized types. Focal seizures involve a specific area of the brain, while generalized seizures affect the entire brain. Focal seizures are more common in children and adults, whereas generalized seizures are more typical in infants and young children.
-
Etiology: The etiology of epilepsy varies depending on the sociodemographic characteristics of the affected population and the extent of diagnostic workup. About 50% of cases in high-income countries lack a documented cause, highlighting the complexity of diagnosing epilepsy.
Prognosis and Treatment Challenges
The outlook for NES patients and the hurdles in treating the condition.
-
Prognosis: The prognosis of epilepsy varies widely among individuals. The overall prognosis is favorable for most patients when measured by seizure freedom. However, some patients experience a worsening course characterized by remission followed by relapse and unremitting seizures. Sudden unexplained death is most frequent in people with generalized tonic-clonic seizures, nocturnal seizures, and drug-refractory epilepsy.
-
Treatment Challenges: Current available treatments for NES are limited to symptomatic approaches, such as the use of benzodiazepines to control seizures. There is no cure for the disease, and treatments primarily focus on managing symptoms rather than addressing the underlying genetic cause.
Social Stigma and Educational Environment
The impact of societal views and education on those with NES.
-
Social Stigma: Despite advances in medical understanding, epilepsy continues to carry significant social stigma. Patients with epilepsy often face discrimination in various aspects of life, including access to health insurance, jobs, and marriage equality. This stigma can impact their quality of life and educational environments.
-
Educational Environment: Studies have shown that patients with epilepsy in communities that understand the pathology and cause of seizures are generally more successful in social and educational environments. Education about epilepsy is crucial for reducing stigma and improving the lives of individuals affected by the condition.
Global Burden and Age-Specific Incidence
The widespread impact of epilepsy and how it varies with age.
-
Global Burden: Epilepsy presents a significant global burden, with approximately 50 million people worldwide affected by the disease. The disease burden is decreasing due to better health care, increased survival rates, and a reduction in environmental risk factors such as communicable diseases.
-
Age-Specific Incidence: The age-specific incidence of epilepsy shows a shift with progressive aging of the worldwide population. The disease is decreasing in younger age groups but increasing in the elderly due to higher frequencies of stroke, neurodegenerative diseases, and tumors in this age group.
Diagnostic Methods and Treatment Approaches
How NES is diagnosed and the ways it is treated.
-
Diagnostic Methods: Diagnostic methods for NES include genetic testing, MRI, and EEG. Genetic testing involves sequencing the CLN8 gene to identify mutations. MRI and EEG help identify lipid content anomalies and electrical discharges in the brain, respectively.
-
Treatment Approaches: Treatment approaches for NES are primarily symptomatic, focusing on managing seizures rather than addressing the underlying genetic cause. Benzodiazepines are commonly used to control seizures, but there is no cure for the disease.
Future Directions
Looking ahead, what can be done to better manage NES?
- Future Directions: Future directions in managing NES include improved access to existing treatments in low-income countries and the development of new effective drugs worldwide. Additionally, education about epilepsy is crucial for reducing stigma and improving the lives of individuals affected by the condition.
Understanding Northern Epilepsy Syndrome
Northern Epilepsy Syndrome (NES) is a rare, severe neurological disorder mostly found in Finland. It's caused by a mutation in the CLN8 gene, leading to seizures, mental deterioration, and cerebellar atrophy. Symptoms usually start in childhood with recurrent seizures and progressively worsen, affecting intellectual and physical abilities. Diagnosis relies on genetic testing, MRI, and EEG. While there's no cure, treatments focus on managing symptoms, primarily using benzodiazepines for seizures. The social stigma around epilepsy remains a significant challenge, impacting patients' quality of life. Education about NES and epilepsy is crucial for reducing this stigma and improving support for affected individuals. Continued research and better access to treatments are essential for future advancements. Understanding NES helps in recognizing the importance of genetic research and the need for comprehensive care for those living with this condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.