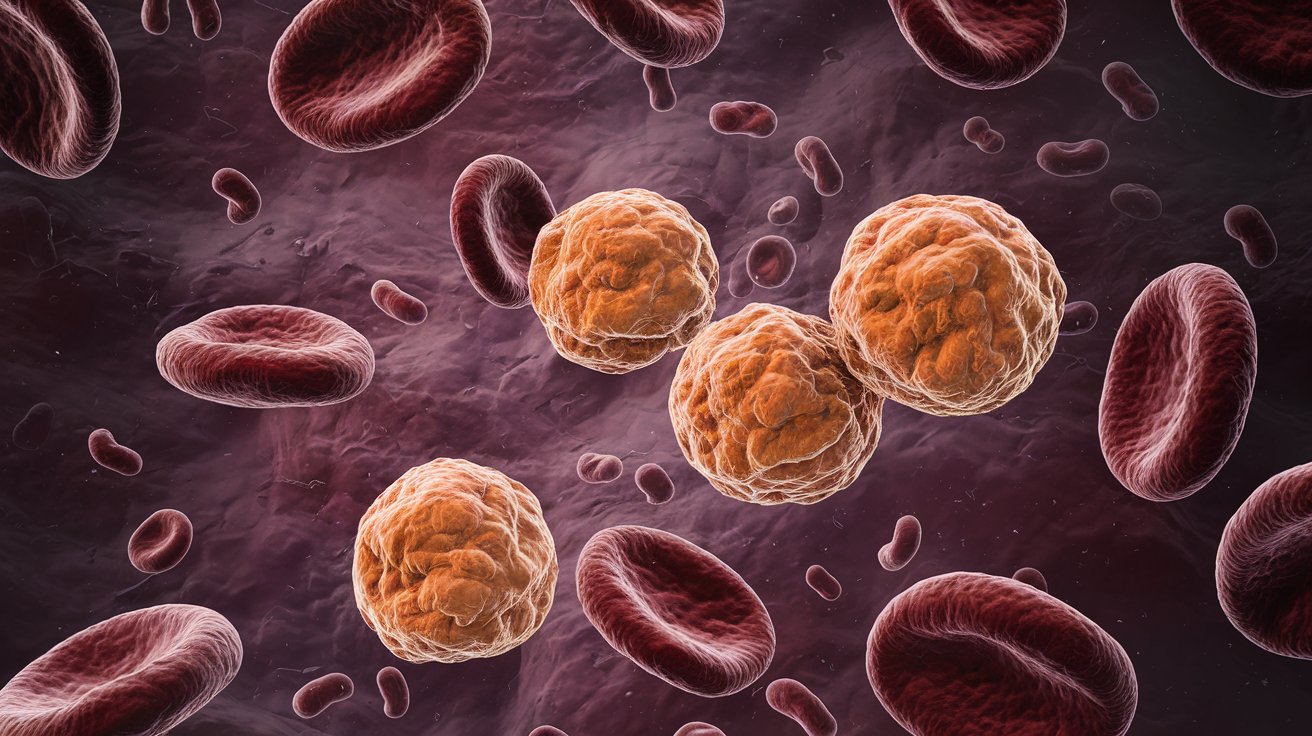
Clonal hypereosinophilia is a rare blood disorder where a specific group of white blood cells, called eosinophils, multiply uncontrollably. This condition often stems from genetic mutations that cause these cells to grow and spread, leading to various health issues. Eosinophils can invade different tissues and organs, causing damage and dysfunction. Diagnosing this condition involves identifying the genetic mutations responsible, often through molecular genetic testing. Treatment usually includes targeted therapies like tyrosine kinase inhibitors, which can effectively manage symptoms. Understanding clonal hypereosinophilia is crucial for proper diagnosis and treatment, ensuring better outcomes for those affected.
Key Takeaways:
- Clonal hypereosinophilia is a rare blood disorder caused by genetic mutations leading to uncontrolled growth of eosinophils, affecting organs and tissues. Accurate diagnosis and targeted therapy are crucial for effective treatment.
- Understanding the clinical presentation, genetic mutations, and treatment options for clonal hypereosinophilia is essential for improving patient care and outcomes. Ongoing research aims to identify new genetic mutations and enhance diagnostic algorithms.
What is Clonal Hypereosinophilia?
Clonal hypereosinophilia, also known as primary hypereosinophilia or clonal eosinophilia, is a rare blood disorder. It involves the abnormal growth of a specific type of white blood cell called eosinophils. Let's dive into some key facts about this condition.
-
Definition and Classification
Clonal hypereosinophilia is a hematological disorder marked by the proliferation of a clone of eosinophils. These cells grow uncontrollably due to genetic mutations. -
Etiology
The cause involves germline mutations in genes that affect hematopoietic stem cells. These mutations lead to the continuous growth and proliferation of these cells. -
Genetic Mutations
Common genetic mutations include the FIP1L1-PDGFRA fusion gene. These mutations cause the cells to grow without regulation.
Clinical Presentation and Symptoms
Understanding how clonal hypereosinophilia presents itself can help in early diagnosis and treatment.
-
Clinical Presentation
Symptoms often resemble those of chronic or acute leukemias, lymphomas, or myeloproliferative disorders. Elevated eosinophil counts are a hallmark. -
Tissue Damage and Organ Dysfunction
High eosinophil levels can lead to tissue damage and organ dysfunction, affecting the heart, lungs, skin, and sinuses.
Diagnosing Clonal Hypereosinophilia
Accurate diagnosis is crucial for effective treatment. Here are some key diagnostic criteria and methods.
-
Diagnostic Criteria
Diagnosis involves identifying a clone of eosinophils in the bone marrow or blood. Molecular genetic testing confirms specific mutations. -
World Health Organization Classification
The WHO classifies clonal hypereosinophilia under "Myeloid and lymphoid neoplasms associated with eosinophilia and abnormalities of PDGFRA, PDGFRB, and FGFR1." -
Chronic Eosinophilic Leukemia (CEL)
CEL-NOS is a subtype characterized by increased blast cells in the blood or bone marrow and eosinophil-related tissue damage.
Treatment Options
Treatment varies depending on the underlying genetic mutations and clinical presentation.
-
Treatment Susceptibility
Many types of clonal hypereosinophilias respond well to relatively non-toxic drugs, making targeted therapy a viable option. -
Tyrosine Kinase Inhibitors
These drugs target specific genetic mutations like the FIP1L1-PDGFRA fusion gene. They effectively reduce eosinophil counts and alleviate symptoms.
Bone Marrow and Cytogenetic Abnormalities
Bone marrow morphology and cytogenetic abnormalities play a significant role in diagnosis and treatment planning.
-
Bone Marrow Morphology
Bone marrow studies help identify true myeloid neoplasms. Genome-wide studies can further clarify "idiopathic" cases. -
Clonal Cytogenetic Abnormalities
Abnormalities like 16q breakage, partial 6q or 10p deletions, and trisomy 7 provide additional diagnostic clues.
Role of Cytokines and T Cells
Cytokines and T cells also play a role in the pathogenesis of clonal hypereosinophilia.
-
Th2 Cytokines and Associated Biological Features
Th2 cytokines like IL-5, IL-4, and IL-13 can lead to increased IgE synthesis and other immune responses. -
Clonality of Phenotypically Aberrant T Cells
Clonal T cells, identified through TCR gene rearrangement patterns, can initially be benign but may progress to T cell lymphoma. -
Progression to T Cell Lymphoma
Clonal cytogenetic abnormalities in T cells can lead to full-blown T cell lymphoma, indicating a pre-malignant state.
Diagnostic Algorithms and Classification Systems
A structured approach to diagnosis helps in identifying the underlying cause and guiding treatment.
-
Diagnostic Algorithm
A multimodality approach, including molecular genetic testing and bone marrow morphology, helps in evaluating patients with hypereosinophilia. -
Etiological Spectrum
Causes range from infections and allergic disorders to drugs and malignancies. Infections are the most common cause. -
Classification Systems
The WHO system focuses on clonal causes, while the ICOG-EO system includes both clonal and non-clonal disorders.
Challenges and Socioeconomic Factors
Managing clonal hypereosinophilia presents several challenges, especially in resource-limited settings.
-
Treatment Outcome
Outcomes vary depending on the underlying cause. Targeted therapy has shown significant efficacy in managing clonal hypereosinophilia. -
Challenges in Diagnosis and Treatment
The wide spectrum of molecular abnormalities and co-occurrence of non-clonal and clonal causes make diagnosis and treatment complex. -
Socioeconomic Factors
Limited resources and expertise in tropical countries pose additional challenges. Published data on HES from these regions is scarce.
Comprehensive Evaluation and Future Directions
A thorough evaluation and ongoing research are essential for improving patient care.
-
Clinical Pathological Evaluation
A comprehensive evaluation, including laboratory tests and clinical assessments, helps identify the underlying cause and guide treatment. -
Point-of-Care Diagnostic Algorithm
This algorithm categorizes acquired eosinophilia into secondary, clonal, and idiopathic types, aiding in accurate diagnosis. -
Future Directions
Ongoing studies aim to identify new genetic mutations and include them in the classification of myeloid and lymphoid neoplasms associated with eosinophilia. -
Research and Advancements
Continued research is needed to address the challenges posed by clonal hypereosinophilia, particularly in resource-limited settings.
Key Takeaways on Clonal Hypereosinophilia
Clonal hypereosinophilia is a complex condition marked by the abnormal growth of eosinophils due to genetic mutations. It can lead to serious tissue damage and organ dysfunction. Diagnosing it involves genetic testing and bone marrow analysis. Treatment often includes tyrosine kinase inhibitors, which target specific mutations. The condition can resemble other hematological disorders, making diagnosis tricky. A comprehensive approach, including molecular genetic testing and clinical evaluation, is essential. Understanding the broad spectrum of causes, from infections to malignancies, helps in managing the condition effectively. Socioeconomic factors, especially in tropical regions, add to the challenges. Ongoing research aims to uncover more about the genetic mutations involved, offering hope for better treatments. Recognizing the signs and seeking timely medical advice can significantly improve outcomes for those affected by clonal hypereosinophilia.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


