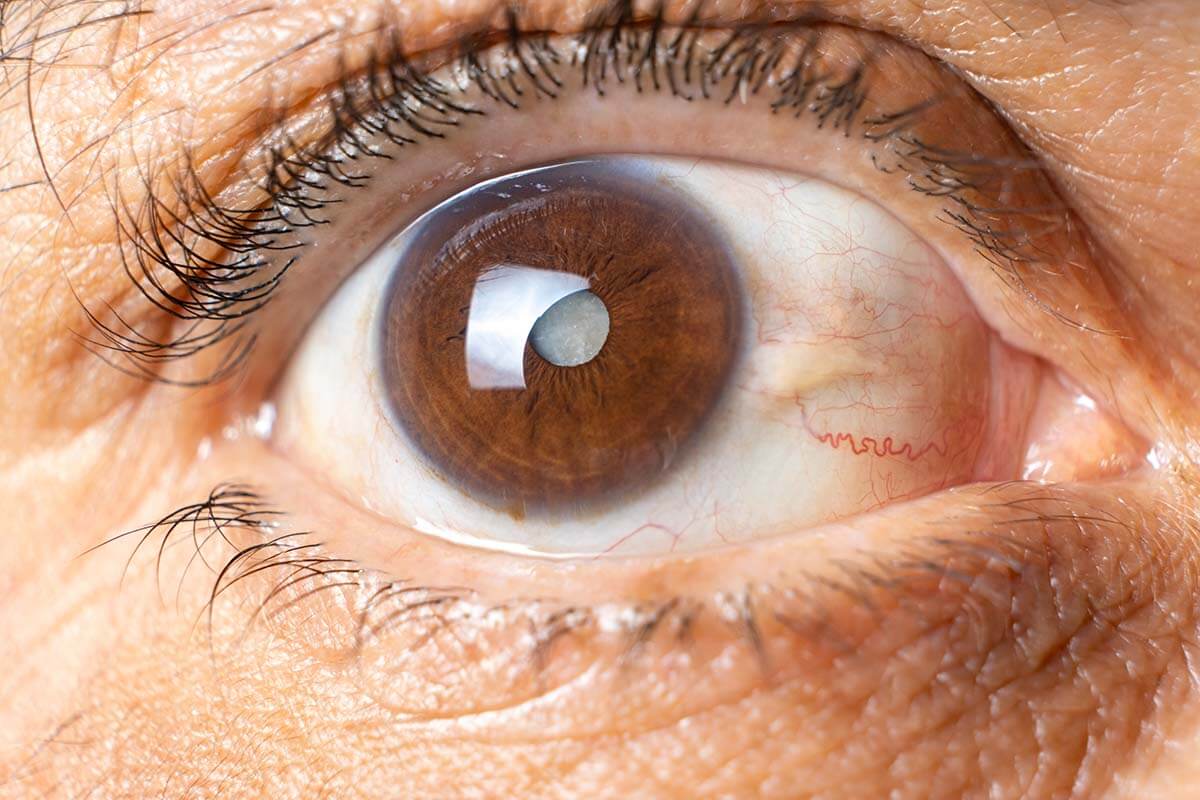
What is Irvine–Gass Syndrome? Irvine–Gass Syndrome, also known as pseudophakic cystoid macular edema (PCME), is a condition that can develop after cataract surgery. It involves fluid buildup in the macula, the part of the retina responsible for sharp, central vision. Named after S. Rodman Irvine and J. Donald M. Gass, who first described it in the mid-20th century, this syndrome can lead to symptoms like blurred vision, distorted lines, and light sensitivity. While modern surgical techniques have reduced its incidence, certain risk factors like previous eye diseases, complex surgeries, and systemic conditions like diabetes can increase the likelihood of developing this condition.
What is Irvine–Gass Syndrome?
Irvine–Gass Syndrome, also known as pseudophakic cystoid macular edema (PCME) or postcataract cystoid macular edema (CME), is a condition that can develop after cataract surgery. It involves fluid accumulation in the macula, the part of the retina responsible for sharp, central vision. Let's dive into some key facts about this syndrome.
-
Definition and Causes
Irvine–Gass Syndrome is a type of macular edema that occurs after cataract surgery. Surgical trauma disrupts the blood-retinal barrier, increasing capillary permeability in the macula and causing fluid buildup. -
Incidence and Risk Factors
The incidence varies but is generally lower with modern surgical techniques, ranging between 0.1% and 1.95%. Risk factors include previous eye diseases, complex surgeries, certain medications, intraoperative complications, and systemic conditions like diabetes.
Symptoms of Irvine–Gass Syndrome
Recognizing the symptoms early can help in managing the condition effectively. Here are the primary symptoms associated with Irvine–Gass Syndrome.
-
Decreased Visual Acuity
Patients often experience blurred vision, described as fuzzy or hazy. -
Distortion of Vision
Straight lines may appear wavy, and there may be central scotoma, an area of decreased or lost vision in the visual field. -
Metamorphopsia
This is the perception of a grid of straight lines as wavy and sometimes separated with dark areas. -
Photophobia
Sensitivity to light is another common symptom. -
Pain or Discomfort
Mild pain or discomfort can vary from patient to patient.
Acute vs. Chronic Presentation
Irvine–Gass Syndrome can present itself in two ways: acute and chronic. Understanding these can help in timely intervention.
-
Acute Presentation
Symptoms usually appear soon after cataract surgery, often within weeks. These symptoms can be more severe but are usually responsive to treatment, typically including corticosteroids. -
Chronic Presentation
Chronic cases may take longer to manifest and can be more challenging to manage. Symptoms might be milder but persistent, sometimes lasting for several months.
Diagnosing Irvine–Gass Syndrome
Accurate diagnosis is crucial for effective treatment. Here are the primary diagnostic methods used.
-
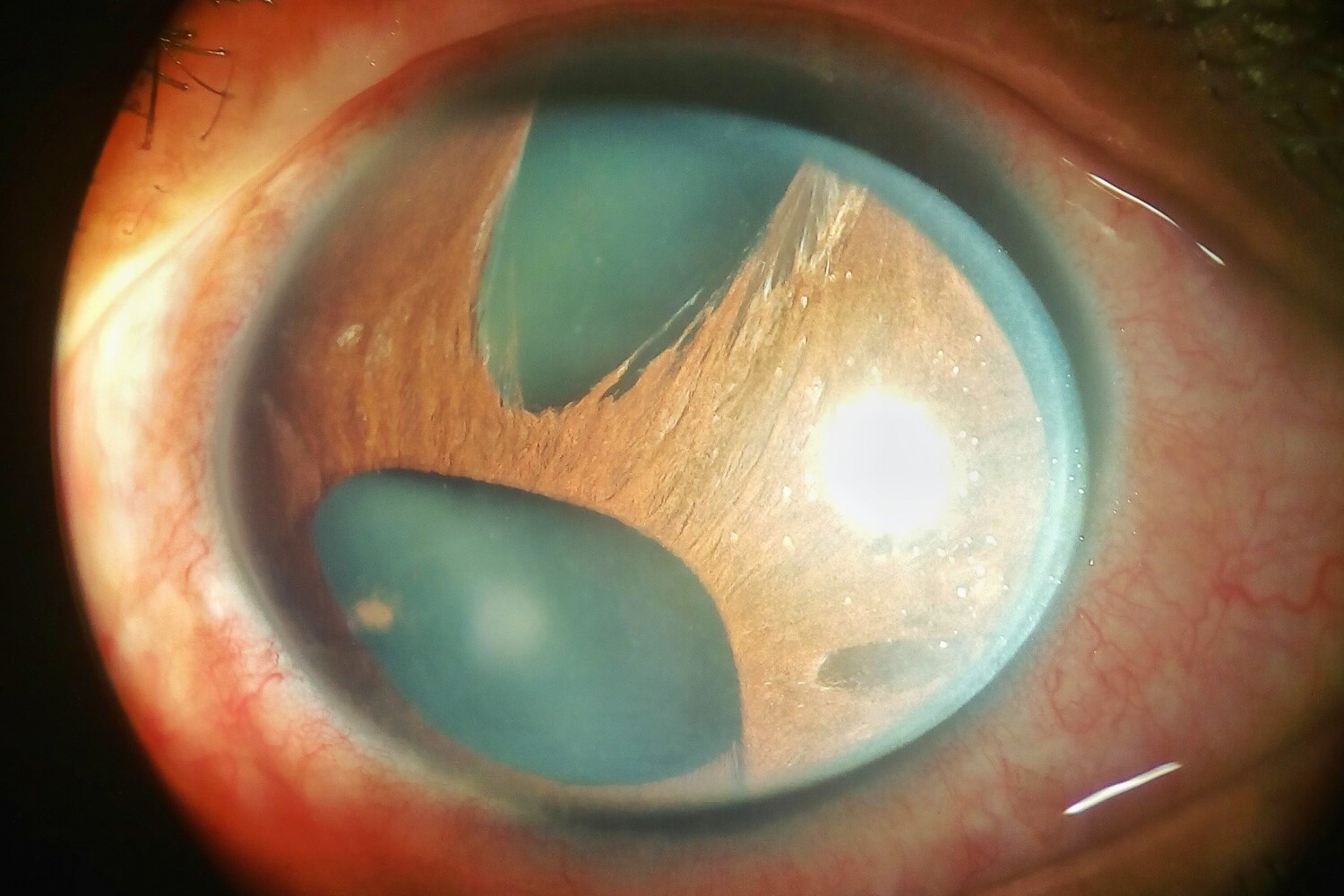
Optical Coherence Tomography (OCT)
This non-invasive imaging test allows healthcare providers to see cross-sectional images of the retina, helping them detect any swelling or changes in the macula. -
Fluorescein Angiography
A fluorescent dye is injected into the bloodstream, highlighting blood vessels in the back of the eye for detailed imaging. This test helps rule out other potential causes of vision loss.
Pathophysiology and Treatment
Understanding the underlying mechanisms and treatment options can aid in managing the condition effectively.
-
Pathophysiology
Surgical manipulation causes significant release of inflammatory mediators, including arachidonic acid, cytokines, lysozyme, and vascular endothelial growth factor (VEGF). This inflammatory response triggers vasodilation and increased vascular permeability in the retina. -
First-Line Treatment
Corticosteroids are frequently administered to block the release of inflammatory mediators. They also act on interleukins and VEGF, encouraging fluid reabsorption by the retinal pigment epithelium. -
Second-Line Treatment
Topical NSAIDs are often used in combination with corticosteroids. A meta-analysis has shown that their use is beneficial for the treatment of chronic CME. -
Additional Therapies
Intravitreal administration of anti-VEGF agents and pars plana vitrectomy may be considered if corticosteroids prove ineffective.
Management and Complications
Effective management can prevent complications and improve quality of life for patients.
-
Management Options
Current management options focus on reducing inflammation and managing fluid accumulation. The choice of treatment depends on the severity of symptoms and the patient's overall health. -
Complications
If left untreated, Irvine–Gass Syndrome can lead to significant complications, including foveolar photoreceptor damage and visual impairment.
Prevention and Clinical Significance
Preventive measures and understanding the clinical significance can help in reducing the incidence of Irvine–Gass Syndrome.
-
Prevention
While it cannot be completely prevented, several measures can reduce the risk, including modern surgical techniques, proper postoperative care, and managing systemic conditions. -
Clinical Significance
Irvine–Gass Syndrome is one of the most common causes of visual loss after cataract surgery. Early diagnosis and intervention are essential to mitigate its effects and prevent long-term visual impairment.
Future Research Directions
Despite advancements, there is still a need for further research to improve treatment protocols and diagnostic tools.
- Future Research Directions
Future studies should focus on developing more effective treatment protocols, particularly for chronic cases, and exploring new diagnostic tools to improve early detection and intervention.
Key Points on Irvine–Gass Syndrome
Irvine–Gass Syndrome, or pseudophakic cystoid macular edema, is a complication after cataract surgery. It involves fluid buildup in the macula, leading to blurry vision and distortion. Older surgical techniques had higher incidences, but modern methods have reduced this to 0.1-1.95%. Risk factors include previous eye diseases, complex surgeries, and systemic conditions like diabetes.
Symptoms range from decreased visual acuity to photophobia. Diagnosis relies on clinical exams, OCT, and fluorescein angiography. Treatment often involves corticosteroids, NSAIDs, and sometimes anti-VEGF agents. While many cases resolve on their own, persistent ones need prolonged care.
Understanding this syndrome is crucial for preventing long-term visual impairment. Early diagnosis and intervention can make a significant difference. Managing risk factors and following up post-surgery are key steps in reducing its impact.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.