What is Idiopathic Pneumonia Syndrome (IPS)? Imagine having pneumonia-like symptoms but no infection causing them. That's IPS. It often affects people who have had a hematopoietic stem cell transplant (HSCT). Symptoms include fever, chills, coughing, and breathing problems. The condition is serious, with a high mortality rate. Diagnosing IPS involves ruling out infections through tests like bronchoalveolar lavage (BAL) and imaging. Risk factors include older age, graft-versus-host disease (GVHD), and certain conditioning regimens used in HSCT. Despite aggressive treatment, the prognosis remains poor. Understanding IPS is crucial for improving patient outcomes and developing better treatments.
What is Idiopathic Pneumonia Syndrome?
Idiopathic Pneumonia Syndrome (IPS) is a serious condition that can occur in patients who have undergone hematopoietic stem cell transplantation (HSCT). It mimics pneumonia but without any infection in the lungs.
-
Definition and Incidence: IPS is a set of pneumonia-like symptoms with no sign of infection in the lung. The incidence of IPS after allogeneic HSCT ranges from 2.2% to 15%.
-
Causes and Risk Factors: Often linked to noninfectious diffuse lung injury, IPS can be triggered by the conditioning regimen used in HSCT. Older age, graft-versus-host disease (GVHD), and multi-organ failure are significant risk factors.
Symptoms and Diagnosis
Recognizing the symptoms and diagnosing IPS can be challenging due to its similarity to other lung conditions.
-
Symptoms: Symptoms include fever, chills, coughing, and breathing problems. Lack of oxygen may also occur, leading to severe complications.
-
Diagnosis: Diagnosis is based on widespread alveolar injury with pneumonia-like symptoms, without evidence of active lower respiratory tract infection. Methods include bronchoalveolar lavage (BAL) and imaging studies.
-
Diagnostic Criteria: Two major requirements for diagnosing IPS are widespread alveolar injury and absence of active lower respiratory tract infection. New methods like biomarkers for fungal infections and multiplex PCR for respiratory viruses are increasingly used.
Pathogen Detection and Impact
Understanding the role of pathogens in IPS is crucial for better management and treatment.
-
Pathogen Detection: Studies show that about half of IPS cases may be linked to hidden infections, with pathogens like human herpesvirus-6 (HHV-6), human rhinovirus (HRV), cytomegalovirus (CMV), and Aspergillus detected in BAL samples.
-
Impact of Pathogens on Mortality: The presence of pathogens in IPS cases is associated with increased mortality. Patients with pathogens detected in BAL had worse day-100 survival compared to those without pathogens.
Clinical Phenotypes and Course
IPS presents in various forms and progresses rapidly, making early detection and treatment vital.
-
Clinical Phenotypes: IPS encompasses a spectrum of clinical presentations, including various forms of lung injury and inflammation.
-
Incubation Period: The incubation period ranges from 4 to 106 days, with most cases occurring around 22 days after transplantation.
-
Mortality Rate: The mortality rate for IPS is high, ranging from 50% to 90% despite aggressive supportive care.
Treatment and Risk Factors
Managing IPS involves supportive care and understanding the risk factors to prevent its occurrence.
-
Supportive Treatment: Treatment focuses on managing symptoms and preventing further lung damage. Steroids are often used, but their effectiveness varies. Mechanical ventilation is often required, indicating a poor prognosis.
-
Risk Factors by Age Group: Older patients (older than 40 years) are at higher risk, especially those undergoing conventional conditioning regimens containing high-dose total body irradiation (TBI). High-dose TBI significantly increases the risk for IPS compared to non-TBI-based regimens in older patients.
Graft-Versus-Host Disease and Diagnosis
GVHD plays a significant role in the development of IPS, and accurate diagnosis is essential for effective management.
-
Acute Graft-Versus-Host Disease (GVHD): Acute GVHD is a significant risk factor for developing IPS. Patients with grade IV acute GVHD are at higher risk.
-
Diagnosis by Lung Biopsy or Autopsy: IPS is often diagnosed by lung biopsy or autopsy, which can confirm widespread alveolar injury.
Interstitial Pneumonitis and Incidence Rates
Understanding the complications and incidence rates of IPS can help in early detection and treatment.
-
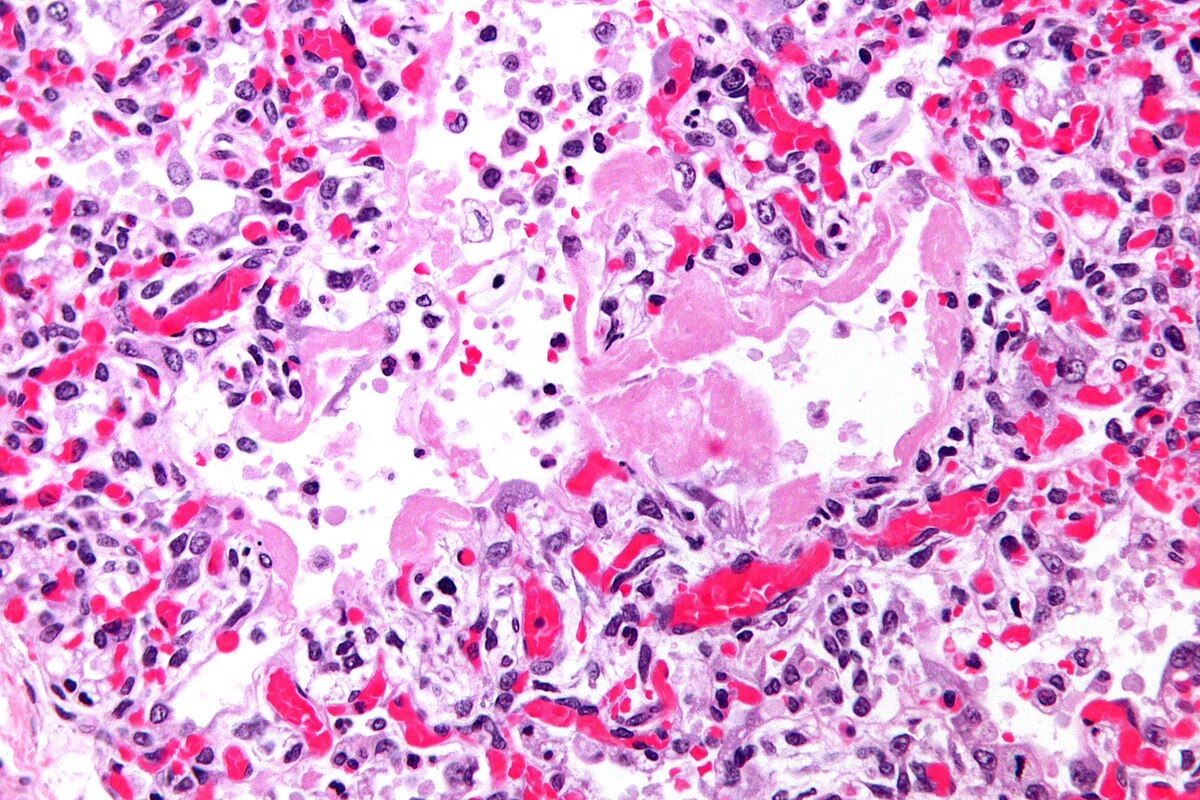
Interstitial Pneumonitis: Interstitial pneumonitis is a significant complication after conventional myeloablative HSCT. It is a form of noninfectious diffuse lung injury that can lead to IPS.
-
Incidence Rates: The incidence rate of IPS after allogeneic HSCT varies widely, ranging from 4% to 12% in different studies.
Clinical Course and Complications
The rapid progression and severe complications of IPS highlight the need for prompt and effective treatment.
-
Clinical Course: IPS typically occurs early after transplantation and progresses rapidly. The condition is associated with a high mortality rate due to severe respiratory failure and multi-organ dysfunction.
-
Renal Insufficiency and Mechanical Ventilation: The presence of renal insufficiency at the onset of IPS and the need for mechanical ventilation are associated with increased risks for death after IPS.
Lung Damage and Future Research
Lung damage from the conditioning regimen plays a crucial role in IPS development, and ongoing research aims to improve outcomes.
-
Lung Damage and Conditioning Regimen: Lung damage from the conditioning regimen plays a crucial role in the development of IPS after HSCT. High-dose TBI and other toxic effects of myeloablative conditioning increase the risk for IPS.
-
Future Research Directions: Further research is needed to understand the pathogenesis of IPS and develop more effective diagnostic and therapeutic strategies. New diagnostic methods like metagenomic next-generation sequencing (NGS) may help identify hidden pathogens and improve diagnostic precision.
Final Thoughts on Idiopathic Pneumonia Syndrome
Idiopathic Pneumonia Syndrome (IPS) is a serious condition that can occur after hematopoietic stem cell transplantation (HSCT). It presents with pneumonia-like symptoms but lacks any infectious cause. With an incidence rate ranging from 2.2% to 15%, IPS remains a significant concern for patients undergoing HSCT. Risk factors include older age, graft-versus-host disease (GVHD), and multi-organ failure. Diagnosis relies on ruling out infections through methods like bronchoalveolar lavage and imaging studies. Despite aggressive supportive care, the mortality rate for IPS is alarmingly high, between 50% and 90%. Steroids and mechanical ventilation are common treatments, though their effectiveness varies. Ongoing research aims to improve diagnostic precision and develop targeted therapies. Understanding IPS's risk factors, symptoms, and treatment options is crucial for better management and outcomes.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


