Carbohydrate-Deficient Glycoprotein Syndrome (CDGS), also known as Congenital Disorders of Glycosylation (CDG), is a group of inherited disorders that mess with how our bodies make glycoconjugates. These disorders can affect many parts of the body, but they often hit the central nervous system the hardest. People with CDGS might have severe developmental delays, low muscle tone, and brain abnormalities. They can also face issues like hypoglycemia, seizures, and liver disease. CDGS usually follows an autosomal recessive inheritance pattern, meaning you need two faulty genes to get it. Diagnosing CDGS involves specific tests, but treatment options are limited, making research crucial for better understanding and management.
Key Takeaways:
- Carbohydrate-Deficient Glycoprotein Syndrome (CDGS) is an inherited disorder affecting glycoconjugate production, leading to severe developmental delays and neurological impairments.
- CDGS primarily impacts the nervous system, causing neurological issues, hormonal imbalances, and reproductive challenges. Currently, there are limited effective therapies available for most CDGS cases.
What is Carbohydrate-Deficient Glycoprotein Syndrome?
Carbohydrate-Deficient Glycoprotein Syndrome (CDGS) is a group of inherited disorders that affect the body's ability to produce glycoconjugates properly. These disorders can impact various organs and systems, often with severe effects on the central nervous system.
- CDGS is a generic term for a group of inherited disorders with primary defects in glycoconjugate biosynthesis.
- The syndrome is also known as congenital disorders of glycosylation (CDG), reflecting the primary biochemical defects in the N-glycosylation pathway.
How is CDGS Inherited?
Understanding how CDGS is passed down through families can help in diagnosing and managing the condition.
- CDGS typically follows an autosomal recessive inheritance pattern, meaning that an individual must inherit two defective genes (one from each parent) to express the condition.
What are the Primary Biochemical Defects?
The biochemical defects in CDGS primarily affect the N-glycosylation pathway, which is crucial for the synthesis of proteins and lipids.
- The primary biochemical defects in CDGS are in the N-glycosylation pathway, which occurs in the cytoplasm and endoplasmic reticulum.
- The most common form of CDGS (type I) is caused by a defect in the phosphomannomutase 2 enzyme, which is essential for mannose processing.
What are the Clinical Presentations?
CDGS can present in various ways, affecting multiple systems in the body.
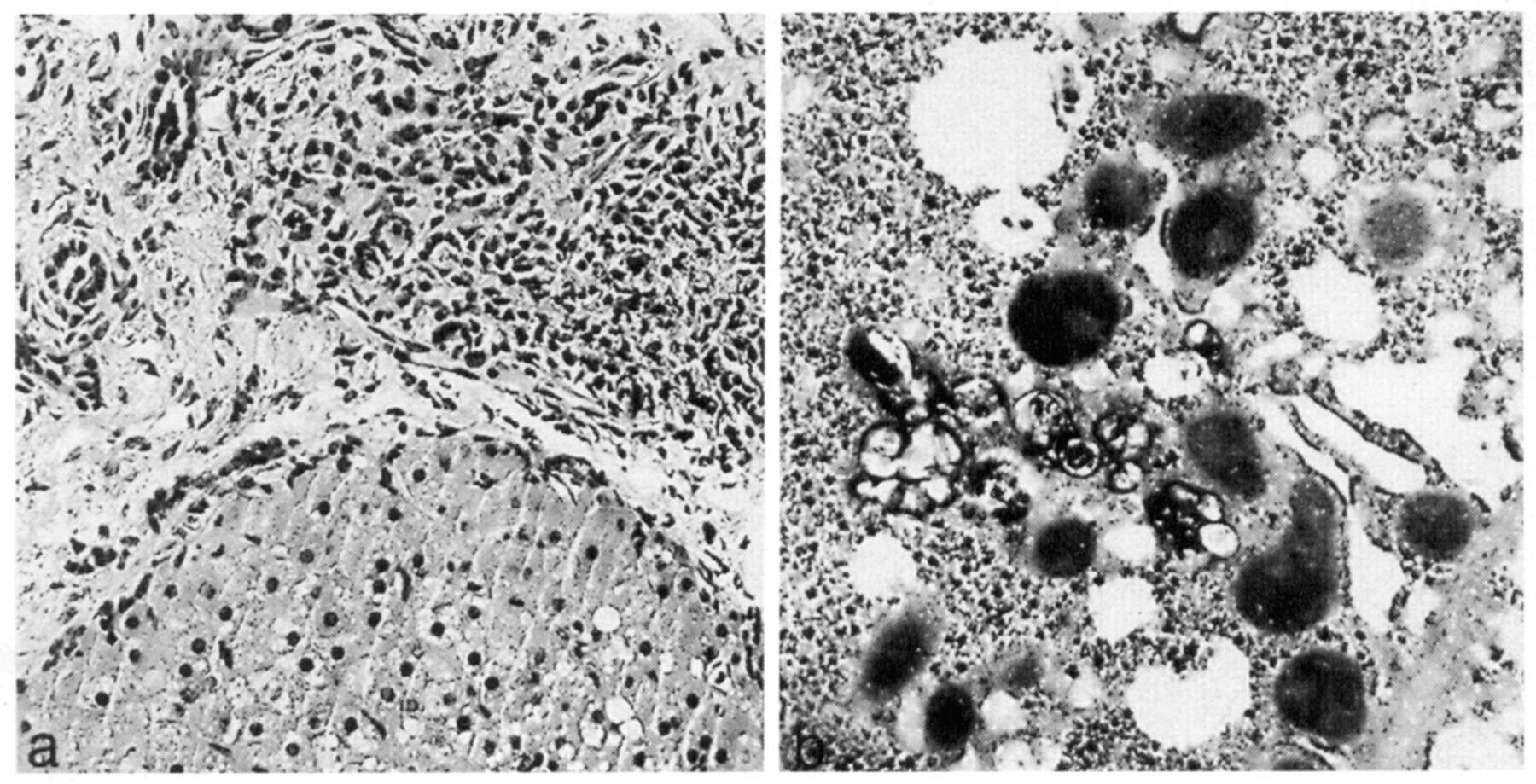
- The clinical presentation of CDGS can vary widely among individuals, but common features include severe developmental delay, low muscle tone in infancy, and brain abnormalities.
- Other features include hypoglycemia, seizures, stroke-like episodes, retinal damage, impaired heart contractility, vomiting, liver disease, diarrhea, and a bleeding tendency.
How Does CDGS Affect the Nervous System?
The central nervous system is often severely impacted by CDGS, leading to various neurological issues.
- The central nervous system is often severely affected, leading to neurological impairment. This can manifest as early onset psychomotor retardation, non-progressive ataxia associated with cerebellar hypoplasia, stable mental retardation, variable peripheral neuropathy, and strabismus.
What are the Endocrine Aspects?
CDGS can also affect endocrine function, particularly in terms of gonadotropin regulation.
- CDGS can affect endocrine function, particularly in terms of gonadotropin regulation. Hypergonadotropic hypogonadism with deficient FSH rather than LH action has been observed in some cases.
- Serum FSH levels are normal in newborns and prepubertal children but elevate in female toddlers and teenagers, as well as in adolescent males. Serum LH concentrations display an analogous age-dependent pattern.
What About Hormone Binding Glycoproteins?
Deficiencies in hormone-binding glycoproteins are common in CDGS, leading to various hormonal imbalances.
- Deficiencies of hormone-binding glycoproteins are common in CDGS. This can lead to abnormal thyroid-binding globulin levels and increased serum TSH concentrations during infancy.
- A subgroup of female patients may present with hypersomatotropism and/or hyperprolactinemia.
How is Growth Hormone Response Affected?
During adolescence, patients with CDGS may exhibit altered glucose metabolism and hormonal regulation.
- During adolescence, patients with CDGS may exhibit an exaggerated insulin response to glucagon, along with paradoxically augmented growth hormone release. This indicates altered glucose metabolism and hormonal regulation.
What Diagnostic Tests are Available?
Reliable diagnostic tests can help identify CDGS, although prenatal diagnosis and heterozygote detection are not yet available.
- A reliable diagnostic test for CDGS involves isoelectric focusing of serum transferrin, which shows a cathodal shift due to partial sialic acid deficiency.
- High serum concentrations of carbohydrate-deficient transferrin (CDT) can be used to verify the diagnosis.
What are Secondary CDG Syndromes?
CDGS should be differentiated from secondary CDG syndromes, which arise from defects in other metabolic pathways.
- CDGS should be differentiated from secondary CDG syndromes such as classical galactosemia. Secondary CDG syndromes arise from defects in other metabolic pathways that affect glycoprotein synthesis.
How Does CDGS Present in Adults?
In adults, CDGS type I presents with various neurological symptoms and some degree of hepatic dysfunction.
- In adults, CDGS type I is characterized by early onset psychomotor retardation, slight facial dysmorphic features, some degree of hepatic dysfunction, and in one case, pericardial effusion. After the age of 15, the disease mainly presents with neurological symptoms like non-progressive ataxia associated with cerebellar hypoplasia, stable mental retardation, variable peripheral neuropathy, and strabismus.
What are Other Physical Manifestations?
CDGS can also cause physical deformities and retinal issues.
- A third of the patients have generalized seizures, usually sporadic, and all have retinal pigmentary degeneration. Additionally, all patients have more or less pronounced thoracic deformity.
How Does CDGS Affect Puberty and Reproduction?
Reproductive issues are common in CDGS, with no female patients passing puberty.
- No female patient with CDGS has passed puberty. The oldest female patient showed premature aging. This indicates severe reproductive issues associated with the syndrome.
Are There Any Effective Therapies?
Currently, no effective therapies exist for most CDGS cases, except for a rare subtype.
- In rare cases of CDGS type Ib (phosphomannose isomerase deficiency), oral administration of mannose may reverse symptoms in some patients. This is the only effective therapy available for this subtype.
Understanding CDGS: A Lifelong Journey
Carbohydrate-deficient glycoprotein syndrome (CDGS), also known as congenital disorders of glycosylation (CDG), presents a complex challenge for affected individuals and their families. This group of inherited disorders impacts various organs and systems, with the central nervous system often bearing the brunt. Symptoms range from severe developmental delays and neurological impairments to endocrine dysfunctions and growth issues. Diagnosing CDGS involves specific tests like isoelectric focusing of serum transferrin, but treatment options remain limited, especially for most subtypes. While oral mannose offers hope for some, particularly those with CDGS type Ib, many patients face a lifelong struggle with no effective therapy. Research continues to seek better understanding and potential treatments. Despite the hurdles, individuals with CDGS can lead socially functional lives, albeit with significant support. Awareness and ongoing research are crucial for improving outcomes and quality of life for those affected by this challenging condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


