What is Benign Autosomal Dominant Myopathy? It's a rare genetic disorder that affects skeletal muscles, leading to muscle weakness. This condition is inherited in an autosomal dominant pattern, meaning a single copy of the mutated gene from one parent can cause the disease. Symptoms often appear in early childhood but can also start in adolescence or later. Muscle weakness varies in severity and may affect different muscle groups. The most common genetic cause is mutations in the DNM2 gene. While there's no cure, supportive care and physical therapy can help manage symptoms. Understanding this condition is crucial for those affected and their families.
Understanding Benign Autosomal Dominant Myopathy
Benign autosomal dominant myopathy is a rare genetic disorder that affects the skeletal muscles. It is characterized by muscle weakness and other related symptoms. Let's dive into 20 key facts about this condition to better understand its impact and management.
-
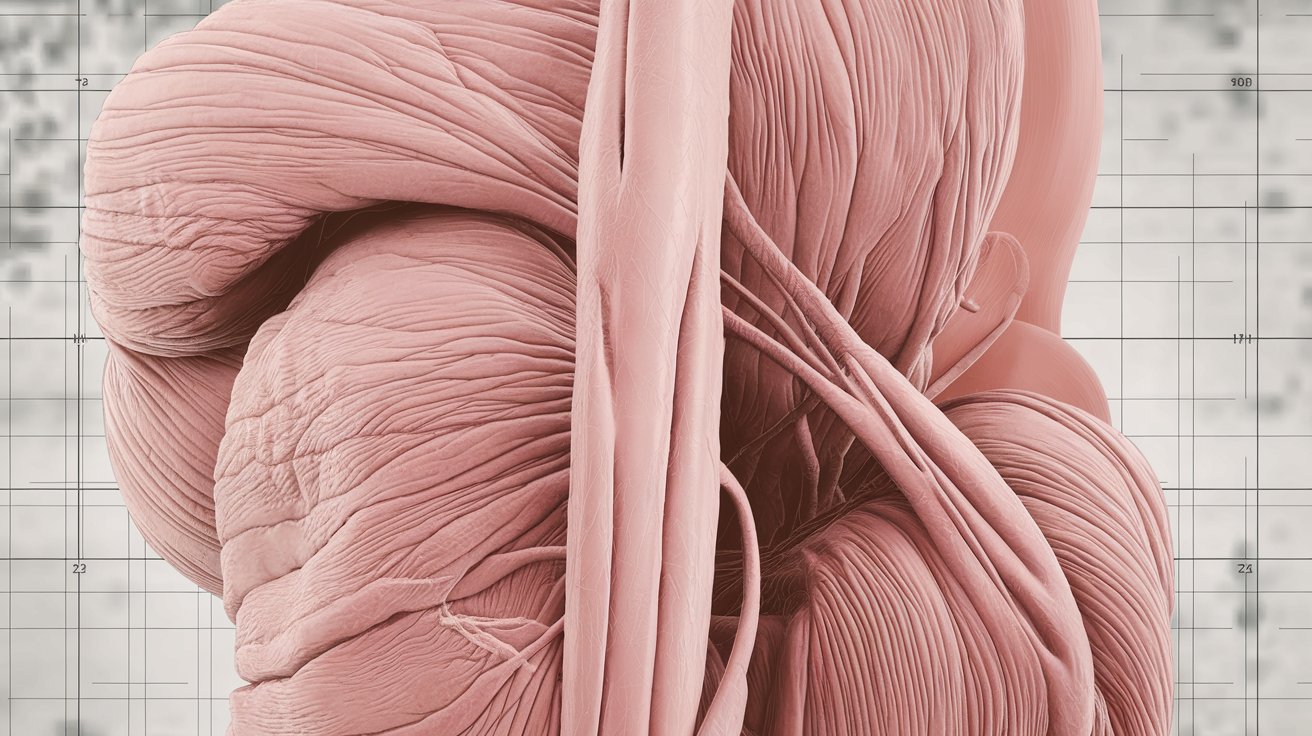
Definition: This myopathy affects skeletal muscles, leading to varying degrees of muscle weakness. The severity can differ from person to person and may target specific muscle groups.
-
Inheritance Pattern: Inherited in an autosomal dominant pattern, meaning one parent with the mutated gene can pass it to their child with a 50% chance.
-
Prevalence: The exact prevalence remains unknown, but it is considered a rare condition, affecting a small percentage of the population.
-
Age of Onset: Symptoms can appear at different ages, typically starting in early childhood but sometimes not until adolescence or later in life.
Symptoms and Diagnosis
Understanding the symptoms and how the condition is diagnosed can help in early detection and management.
-
Symptoms: Muscle weakness is the primary symptom, which can vary in severity and affect different muscle groups. Common signs include low muscle tone, weakness in distal/proximal muscles, rib cage deformities, drooping eyelids, eye muscle weakness, and facial muscle weakness.
-
Muscle Biopsy Findings: Muscle biopsies often show centrally placed nuclei and type 1 muscle fiber predominance. Oxidative stains may reveal radial sarcoplasmic strands in fibers with central nuclei.
-
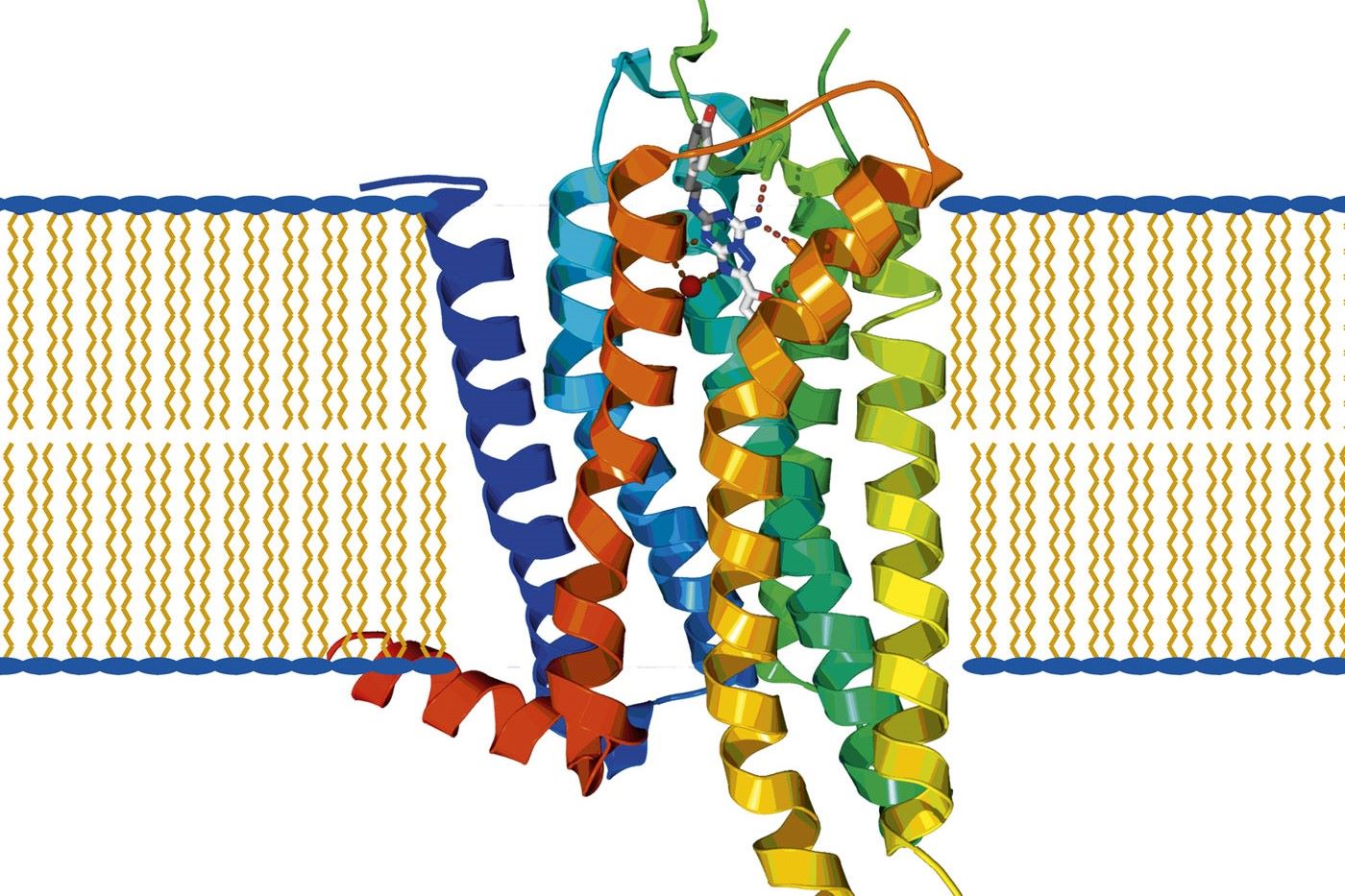
Genetic Causes: The most common genetic cause is mutations in the DNM2 gene on chromosome 19p13.2. Other rare genes like BIN1 and CCDC78 can also cause similar symptoms.
-
Diagnostic Approach: Diagnosis involves histopathological findings combined with clinical features. Genetic testing confirms mutations in the DNM2 or other related genes. Muscle MRI can show early involvement of specific muscle groups.
Differential Diagnoses and Prenatal Diagnosis
Differentiating benign autosomal dominant myopathy from other conditions is crucial for accurate diagnosis and management.
-
Differential Diagnoses: Conditions like other congenital myopathies with distal involvement, myotonic dystrophy, and fascio-scapulo-humeral dystrophy need to be ruled out if facial involvement is prominent.
-
Prenatal Diagnosis: If a family member's mutation is known, prenatal diagnosis is possible, allowing for early detection and preparation.
Management and Progression
Managing benign autosomal dominant myopathy involves a multidisciplinary approach to address symptoms and improve quality of life.
-
Management: No curative treatment exists. Supportive care includes physical therapy, bracing, and sometimes surgery to address specific complications.
-
Progression: The disease usually progresses slowly. Muscle strength may gradually decline, potentially leading to loss of independent ambulation after the sixth decade.
-
Cardiorespiratory Function: Generally normal in most cases, but early onset patients might develop restrictive respiratory impairment over time.
Neuropathic Signs and Family History
Recognizing neuropathic signs and understanding family history can aid in diagnosis and management.
-
Neuropathic Signs: Absence of tendon reflexes and fibrillations or reduced compound muscle action potential on electrophysiological exams may be present.
-
Family History: A thorough family history helps identify other affected members and understand the inheritance pattern. Genetic counseling is recommended for all patients and families.
Supportive Care and Research
Supportive care and ongoing research are vital in managing the condition and improving patient outcomes.
-
Supportive Care: Managing airway, breathing, circulation, hydration, and intensive care as needed. Physical therapy and bracing help maintain muscle function and prevent further deterioration.
-
Drug Therapy: No specific drug therapy exists, but medications may manage associated symptoms like muscle spasms or pain.
-
Surgical Interventions: Sometimes necessary to address complications like contractures or respiratory issues, usually part of a comprehensive management plan.
-
Research Activities: Ongoing research focuses on understanding genetic causes, developing diagnostic tools, and exploring potential therapies. Studies aim to improve diagnostic accuracy and treatment outcomes.
-
Patient Education: Crucial for effective management. Patients and families need to understand the disease, its progression, and available management options. Lifestyle modifications like a balanced diet and regular physical activity help maintain muscle strength.
Understanding Benign Autosomal Dominant Myopathy
Benign autosomal dominant myopathy is a rare genetic disorder causing muscle weakness. It’s inherited in an autosomal dominant pattern, meaning a single copy of the mutated gene can cause the disease. Symptoms like hypotonia, ptosis, and muscle weakness often appear in early childhood but can start later. Diagnosis involves genetic testing, muscle biopsies, and MRI scans. While there’s no cure, supportive care, physical therapy, and sometimes surgery help manage symptoms. The condition progresses slowly, with most patients maintaining normal cardiorespiratory function. Research continues to uncover more about the genetic causes and potential treatments. Understanding this condition helps patients and families manage it better, ensuring a better quality of life.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.