Sporotrichosis is a fungal infection that often gets overlooked, yet it can have serious consequences. Caused by the fungus Sporothrix schenckii, this infection typically affects the skin but can spread to other parts of the body. How do you get sporotrichosis? Usually, it happens through a scratch or puncture wound from contaminated plant material like thorns, hay, or moss. Gardeners, farmers, and florists are particularly at risk. Symptoms include nodules or ulcers on the skin, which can be mistaken for other conditions. Is sporotrichosis contagious? No, it doesn't spread from person to person. However, early diagnosis and treatment are crucial to prevent complications. Treatment often involves antifungal medications, which can take several months to be effective. Understanding sporotrichosis helps in taking preventive measures and seeking timely medical advice.
Key Takeaways:
- Sporotrichosis, also known as "rose gardener's disease," is a fungal infection that primarily affects the skin and can spread to other parts of the body. It is not contagious and can be treated effectively with antifungal medications.
- People who work with soil and plants, such as gardeners, are at higher risk of contracting sporotrichosis. Wearing protective clothing, practicing good hygiene, and seeking early treatment are essential for prevention and management.
What is Sporotrichosis?
Sporotrichosis, often called "rose gardener's disease," is a fungal infection caused by the fungus Sporothrix schenckii. This infection typically affects the skin but can spread to other parts of the body. Here are some intriguing facts about this disease.
-
Sporotrichosis is a fungal infection that primarily affects the skin, though it can also impact the lungs, bones, and joints.
-
The fungus responsible for sporotrichosis, Sporothrix schenckii, is found in soil, plants, and decaying vegetation.
-
Rose gardeners are at risk because the fungus often enters the body through small cuts or punctures from thorns.
-
Sporotrichosis is not contagious. It cannot be spread from person to person.
-
Symptoms usually appear within one to twelve weeks after exposure to the fungus.
Symptoms and Diagnosis
Understanding the symptoms and how sporotrichosis is diagnosed can help in early detection and treatment.
-
Initial symptoms include small, painless bumps on the skin that can become larger and resemble ulcers.
-
The infection can spread along the lymph nodes, causing a series of nodules that follow the path of the lymphatic system.
-
In rare cases, sporotrichosis can affect the lungs, leading to symptoms similar to tuberculosis.
-
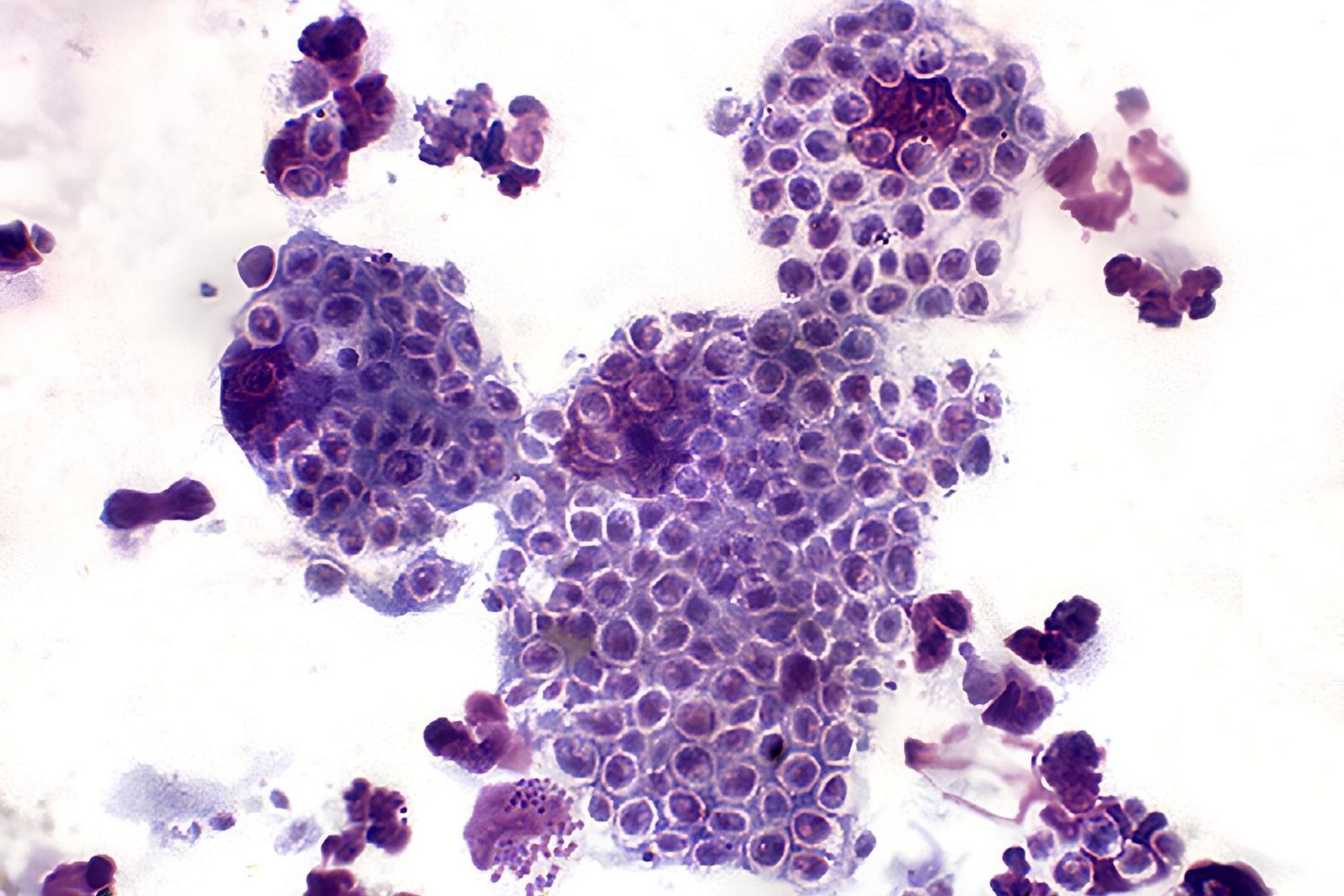
Diagnosis is typically made through a biopsy of the affected tissue, where the fungus can be identified under a microscope.
-
A culture test can also be used to grow the fungus from a sample, confirming the diagnosis.
Treatment Options
Once diagnosed, sporotrichosis can be treated effectively with antifungal medications.
-
The most common treatment is itraconazole, an antifungal medication taken orally.
-
For severe cases, amphotericin B may be administered intravenously.
-
Treatment duration can vary from three to six months, depending on the severity of the infection.
-
In some cases, potassium iodide solution is used, especially in resource-limited settings.
-
Early treatment is crucial to prevent the infection from spreading to other parts of the body.
Risk Factors and Prevention
Knowing the risk factors and how to prevent sporotrichosis can help reduce the chances of contracting the infection.
-
People who work with soil and plants, such as farmers and gardeners, are at higher risk.
-
Wearing protective clothing like gloves and long sleeves can help prevent cuts and punctures that allow the fungus to enter the skin.
-
Good hygiene practices such as washing hands and cleaning wounds promptly can reduce the risk of infection.
-
Pets can also be affected by sporotrichosis, particularly cats, which can then transmit the fungus to humans through scratches or bites.
-
Avoiding contact with stray animals and ensuring pets are healthy can help prevent transmission.
Geographic Distribution
Sporotrichosis is more common in certain parts of the world, and understanding its distribution can help in awareness and prevention.
-
The infection is most prevalent in tropical and subtropical regions.
-
Countries like Brazil, Mexico, and Peru report higher cases of sporotrichosis.
-
In the United States, the disease is more common in southern states, particularly those with warm, humid climates.
-
Outbreaks have been reported in specific communities, often linked to environmental factors or occupational exposure.
-
Climate change may influence the distribution of sporotrichosis, potentially expanding its range.
Historical Context
Sporotrichosis has a rich history, with significant milestones in its discovery and understanding.
-
The disease was first described in 1898 by Benjamin Schenck, an American medical student.
-
The fungus was named Sporothrix schenckii in honor of Schenck's discovery.
-
Early treatments included potassium iodide, which is still used in some cases today.
-
Advancements in antifungal medications have significantly improved the prognosis for those affected by sporotrichosis.
-
Research continues to explore new treatments and better understand the disease's mechanisms.
Interesting Facts
Here are some additional fascinating tidbits about sporotrichosis that you might find intriguing.
-
Sporotrichosis can affect animals such as cats, dogs, and horses, making it a concern for veterinarians.
-
The disease is sometimes called "rose handler's disease" due to its association with thorny plants.
-
Sporotrichosis can mimic other skin conditions, making accurate diagnosis essential for proper treatment.
-
The fungus can survive in the environment for long periods, especially in moist, organic matter.
-
Public health campaigns in endemic areas focus on educating at-risk populations about prevention and early detection.
Research and Future Directions
Ongoing research aims to improve our understanding and management of sporotrichosis.
-
Scientists are exploring new antifungal agents that may offer more effective treatment options.
-
Genetic studies of the fungus help researchers understand its virulence and resistance mechanisms.
-
Epidemiological studies track the spread and impact of sporotrichosis in different regions.
-
Public health initiatives aim to reduce the incidence of sporotrichosis through education and improved hygiene practices.
-
Collaboration between veterinarians and medical professionals is crucial for managing cases that involve both humans and animals.
Sporotrichosis in Pop Culture
While not as well-known as some other diseases, sporotrichosis has made its way into popular culture in various ways.
-
The disease has been featured in medical dramas and documentaries, highlighting its impact on affected individuals.
-
Books and articles about gardening often mention sporotrichosis as a risk for avid gardeners.
-
Public awareness campaigns sometimes use creative methods, such as cartoons or social media, to educate people about the disease.
-
Sporotrichosis has inspired some artists and writers to create works that explore the human experience of dealing with a chronic illness.
-
Educational programs in schools and community centers often include information about sporotrichosis in health and science curricula.
Final Thoughts
Sporotrichosis is a fascinating and complex disease with many aspects to explore. From its causes and symptoms to treatment and prevention, understanding this infection can help reduce its impact on individuals and communities.
-
Awareness and education are key to preventing sporotrichosis and ensuring early treatment for those affected.
-
Continued research will likely lead to new insights and improved management strategies for this fungal infection.
-
Community involvement in public health initiatives can help reduce the incidence of sporotrichosis in endemic areas.
-
Healthcare professionals play a crucial role in diagnosing and treating sporotrichosis, ensuring better outcomes for patients.
-
Sporotrichosis serves as a reminder of the importance of understanding and respecting the natural world, as well as the potential risks it can pose to human health.
Final Thoughts on Sporotrichosis
Sporotrichosis, often called "rose gardener's disease," isn't just a gardener's concern. This fungal infection, caused by Sporothrix schenckii, can affect anyone who comes into contact with contaminated soil, plants, or even animals. Recognizing symptoms early, like skin ulcers or nodules, is crucial for effective treatment. While it's treatable with antifungal medications, prevention remains key. Wearing gloves and protective clothing when handling plants or soil can significantly reduce risk. Understanding the basics of sporotrichosis helps in staying informed and safe. Stay vigilant, and don't hesitate to seek medical advice if you suspect an infection. Knowledge is power, and being aware of sporotrichosis can make a big difference in managing and preventing this infection.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
