Mitochondrial Trifunctional Protein Deficiency is a rare genetic disorder that affects the body's ability to break down certain fats into energy, especially during periods without food. This condition can lead to serious health issues, including muscle weakness, heart problems, and liver disease. Symptoms often appear in infancy or early childhood and can vary widely in severity. Diagnosis typically involves genetic testing, blood tests, and muscle biopsies. Treatment focuses on managing symptoms and preventing complications, often through a specialized diet and regular medical monitoring. Understanding this condition is crucial for those affected and their families, as early intervention can significantly improve quality of life.
Key Takeaways:
- Mitochondrial Trifunctional Protein Deficiency (MTPD) is a rare genetic disorder affecting fat breakdown, leading to various symptoms. Diagnosis, dietary management, and support are crucial for individuals living with MTPD.
- Early diagnosis and ongoing management are key for individuals with MTPD. Research into gene therapy and clinical trials offer hope for improved treatments and a potential cure in the future.
Understanding Mitochondrial Trifunctional Protein Deficiency
Mitochondrial Trifunctional Protein Deficiency (MTPD) is a rare genetic disorder that affects the body's ability to break down certain fats. This condition can lead to serious health issues, especially in infants and young children. Here are some key facts to help you understand MTPD better.
-
MTPD is a metabolic disorder: It disrupts the normal process of breaking down long-chain fatty acids into energy.
-
Caused by mutations: Mutations in the HADHA or HADHB genes cause MTPD.
-
Inherited condition: MTPD follows an autosomal recessive inheritance pattern, meaning both parents must carry the mutated gene.
-
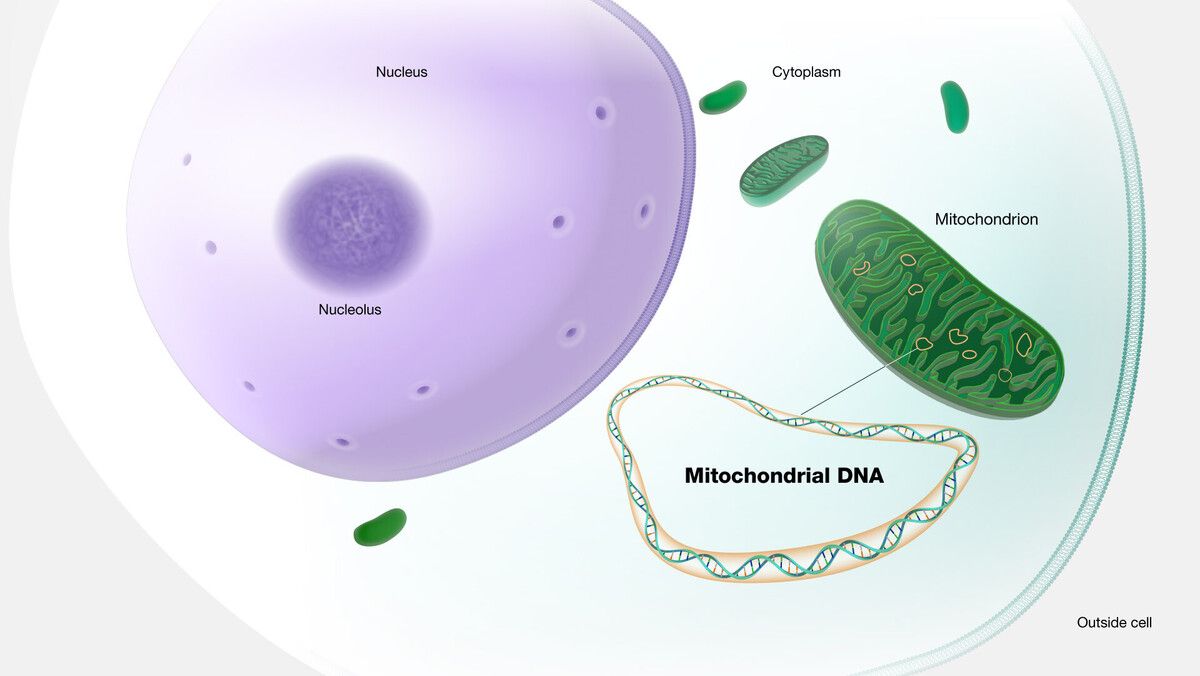
Affects mitochondria: The disorder specifically impacts the mitochondria, the energy-producing structures within cells.
-
Symptoms vary: Symptoms can range from mild to severe and may include muscle weakness, heart problems, and liver issues.
-
Early onset: Symptoms often appear in infancy or early childhood.
-
Hypoglycemia risk: Children with MTPD are at risk of hypoglycemia, or low blood sugar levels.
-
Cardiomyopathy: Some individuals may develop cardiomyopathy, a disease of the heart muscle.
-
Liver dysfunction: Liver problems are common in those with MTPD.
-
Muscle pain: Muscle pain and weakness can occur, especially during physical activity.
Diagnosis and Treatment
Diagnosing and treating MTPD can be challenging due to its rarity and the variability of symptoms. Here are some important facts about the diagnosis and treatment of this condition.
-
Newborn screening: Some regions include MTPD in their newborn screening programs.
-
Blood tests: Blood tests can detect abnormal levels of certain fatty acids.
-
Genetic testing: Genetic testing confirms the diagnosis by identifying mutations in the HADHA or HADHB genes.
-
Muscle biopsy: A muscle biopsy may be performed to examine the mitochondria.
-
Dietary management: A low-fat, high-carbohydrate diet helps manage symptoms.
-
Medium-chain triglycerides: Supplements with medium-chain triglycerides (MCTs) provide an alternative energy source.
-
Frequent meals: Eating small, frequent meals helps maintain blood sugar levels.
-
Avoid fasting: Fasting can trigger symptoms, so it should be avoided.
-
Medications: Some medications may help manage symptoms, such as those for heart problems.
-
Regular monitoring: Regular medical check-ups are essential to monitor the condition.
Living with MTPD
Living with MTPD requires careful management and support. Here are some facts about daily life and long-term outlook for individuals with this condition.
-
Lifelong condition: MTPD is a lifelong condition that requires ongoing management.
-
Support groups: Support groups can provide valuable resources and emotional support.
-
Education: Educating family members and caregivers is crucial for effective management.
-
Emergency plan: Having an emergency plan in place is important for managing acute episodes.
-
Physical activity: Moderate physical activity is beneficial but should be carefully monitored.
-
School accommodations: Children with MTPD may need special accommodations at school.
-
Medical alert: Wearing a medical alert bracelet can be lifesaving in emergencies.
-
Nutritional support: Working with a dietitian ensures proper nutritional management.
-
Mental health: Mental health support is important for coping with the challenges of MTPD.
-
Research and advancements: Ongoing research aims to improve understanding and treatment of MTPD.
Prognosis and Future Directions
The prognosis for individuals with MTPD varies widely. Here are some facts about the long-term outlook and future directions in research and treatment.
-
Variable prognosis: Prognosis depends on the severity of the condition and the effectiveness of management.
-
Early intervention: Early diagnosis and intervention improve outcomes.
-
Potential complications: Complications can include heart failure, liver failure, and developmental delays.
-
Life expectancy: Life expectancy varies but can be normal with proper management.
-
Gene therapy: Research into gene therapy offers hope for future treatments.
-
Clinical trials: Clinical trials are ongoing to find new treatments and improve existing ones.
-
Patient registries: Patient registries help researchers collect data and improve understanding of MTPD.
-
Advocacy: Advocacy groups work to raise awareness and support research efforts.
-
Funding: Funding for research is crucial to finding better treatments and a potential cure.
-
Hope for the future: Advances in medical research continue to offer hope for those affected by MTPD.
Final Thoughts on Mitochondrial Trifunctional Protein Deficiency
Understanding Mitochondrial Trifunctional Protein Deficiency (MTPD) is crucial for those affected. This rare genetic disorder impacts the body's ability to break down certain fats, leading to serious health issues. Early diagnosis and treatment can make a significant difference in managing symptoms and improving quality of life. Genetic counseling is recommended for families with a history of MTPD to understand the risks and options available.
Research continues to evolve, offering hope for better treatments and possibly a cure in the future. Staying informed and connected with healthcare providers and support groups can provide valuable resources and emotional support. Knowledge empowers individuals and families to navigate the challenges of MTPD more effectively.
By spreading awareness and understanding, we can contribute to a better future for those living with this condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
