Villaret’s Syndrome might sound like a complex medical term, but understanding it can be quite straightforward. This rare condition involves a combination of symptoms due to damage in specific nerves. Symptoms often include hoarseness, difficulty swallowing, and a drooping eyelid. These occur because the syndrome affects the lower cranial nerves and the sympathetic nerves. Causes can range from infections to tumors pressing on these nerves. Knowing about Villaret’s Syndrome is crucial for early diagnosis and treatment. In this post, we’ll explore 30 intriguing facts about this condition, shedding light on its symptoms, causes, and treatments. Ready to learn more? Let’s dive in!
Key Takeaways:
- Villaret’s Syndrome is a rare neurological disorder that can be caused by infections, tumors, trauma, vascular issues, or autoimmune disorders. It can lead to a variety of symptoms, making it challenging to diagnose and treat.
- Early diagnosis and treatment are crucial for a good outcome in Villaret’s Syndrome. Treatment options include medications, surgery, physical therapy, speech therapy, and lifestyle changes. Ongoing therapy and support systems play a vital role in recovery.
What is Villaret’s Syndrome?
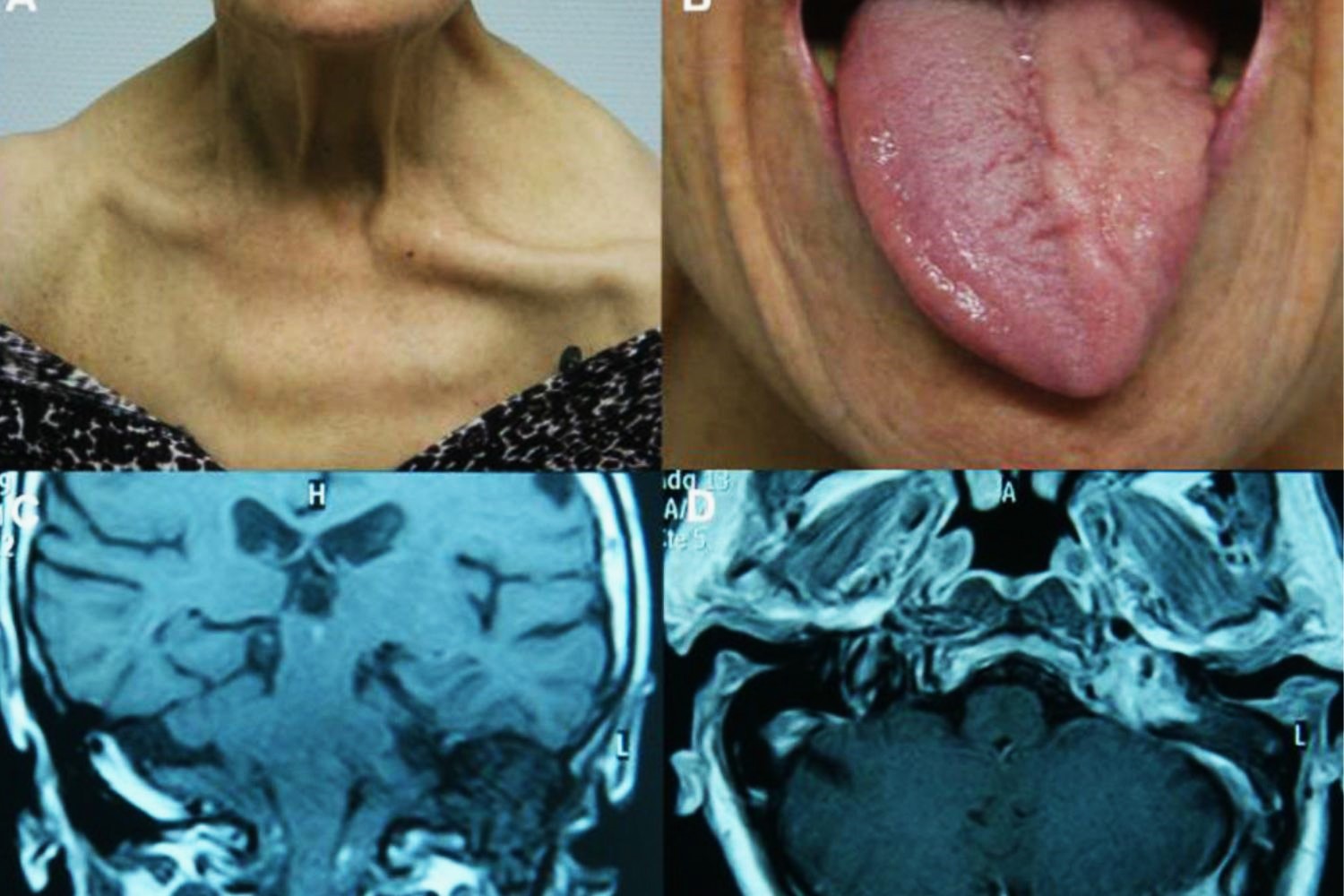
Villaret’s Syndrome is a rare neurological disorder that affects the nerves in the neck and head. It can cause a variety of symptoms due to the involvement of multiple cranial nerves. Understanding this condition can be quite complex, but here are some fascinating facts to help you grasp it better.
Causes of Villaret’s Syndrome
Villaret’s Syndrome can be triggered by several underlying conditions. Knowing these causes can help in early diagnosis and treatment.
- Infections: Bacterial or viral infections can lead to inflammation, affecting the nerves in the neck and head.
- Tumors: Growths in the neck or base of the skull can compress nerves, leading to symptoms.
- Trauma: Injuries to the neck or head can damage nerves, causing the syndrome.
- Vascular Issues: Problems with blood vessels, such as aneurysms or thrombosis, can impact nerve function.
- Autoimmune Disorders: Conditions like lupus or multiple sclerosis can cause nerve inflammation.
Symptoms of Villaret’s Syndrome
The symptoms of Villaret’s Syndrome can vary widely, making it a challenging condition to diagnose. Here are some of the most common signs.
- Horner’s Syndrome: This includes drooping eyelids, constricted pupils, and lack of sweating on one side of the face.
- Hoarseness: Damage to the vagus nerve can cause changes in voice.
- Difficulty Swallowing: The glossopharyngeal nerve’s involvement can make swallowing hard.
- Facial Pain: Trigeminal nerve issues can lead to severe facial pain.
- Hearing Loss: Auditory nerve damage can result in partial or complete hearing loss.
Diagnosis of Villaret’s Syndrome
Diagnosing Villaret’s Syndrome involves a combination of clinical evaluation and diagnostic tests. Here’s how doctors typically approach it.
- Medical History: A thorough review of the patient’s medical history is crucial.
- Physical Examination: Doctors look for signs like Horner’s Syndrome and other neurological deficits.
- Imaging Tests: MRI and CT scans help identify tumors, vascular issues, or other structural problems.
- Blood Tests: These can detect infections or autoimmune markers.
- Electromyography (EMG): This test measures the electrical activity of muscles and nerves.
Treatment Options for Villaret’s Syndrome
Treatment for Villaret’s Syndrome focuses on addressing the underlying cause and managing symptoms. Here are some common approaches.
- Medications: Antibiotics for infections, steroids for inflammation, or pain relievers for symptom management.
- Surgery: Removing tumors or repairing vascular issues may be necessary.
- Physical Therapy: Helps improve muscle strength and coordination.
- Speech Therapy: Assists with swallowing and speech difficulties.
- Lifestyle Changes: Managing stress and maintaining a healthy diet can support overall well-being.
Prognosis and Recovery
The outlook for Villaret’s Syndrome varies depending on the cause and severity. Here’s what you need to know about recovery.
- Early Diagnosis: Early detection and treatment improve the chances of a good outcome.
- Chronic Conditions: Some underlying causes, like autoimmune disorders, may require long-term management.
- Rehabilitation: Ongoing therapy can help regain lost functions.
- Support Systems: Family and community support play a crucial role in recovery.
- Monitoring: Regular follow-ups with healthcare providers ensure that any changes in condition are promptly addressed.
Interesting Facts about Villaret’s Syndrome
Here are some lesser-known yet intriguing facts about Villaret’s Syndrome that highlight its complexity and rarity.
- Named After: The syndrome is named after French neurologist Maurice Villaret, who first described it in the early 20th century.
- Rare Condition: It is extremely rare, with only a few documented cases worldwide.
- Multifaceted Symptoms: The syndrome can mimic other neurological disorders, making diagnosis tricky.
- Research: Ongoing research aims to better understand the syndrome and improve treatment options.
- Awareness: Increased awareness among healthcare providers can lead to earlier diagnosis and better outcomes for patients.
Final Thoughts on Villaret’s Syndrome
Villaret’s Syndrome, a rare neurological disorder, affects the lower cranial nerves and sympathetic nerves. Symptoms include hoarseness, difficulty swallowing, and facial pain. Understanding these signs can lead to quicker diagnosis and better management. Though rare, awareness is crucial for those in medical fields and individuals experiencing unexplained symptoms. Treatment often involves addressing the underlying cause, which can range from infections to tumors. Early intervention can significantly improve quality of life.
Stay informed about rare conditions like Villaret’s Syndrome. Knowledge empowers patients and healthcare providers alike. If you or someone you know shows symptoms, seek medical advice promptly. Awareness and education are key in managing and treating rare disorders. Keep this information handy, and share it with others. It might just make a difference in someone’s life.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
